Abstract
Background
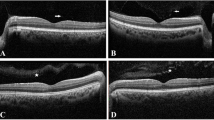
To investigate the effect of iron overload on macular perfusion among transfusion-dependent thalassemia (TDT) patients using optical coherence tomography angiography (OCTA)
Methods
The study is a prospective observational case–control study. It included 27 eyes from 27 children with transfusion-dependent β-thalassemia and 25 eyes from 25 age-matched controls.
All participants were evaluated clinically and with OCTA Avanti RTVue-XR system (Optovue) to assess macular microvascular changes, by measuring vessels density (VDs) and foveal avascular zone (FAZ) area, at both superficial and deep retinal plexuses and at choriocapillaris level.
Results
Foveal and parafoveal zones were significantly thinner among thalassemia patients, with significantly larger FAZ area at the level of both superficial and deep retinal plexuses when compared with control group. The thalassemia group showed significant lower values compared with the controls regarding whole-image, foveal, and parafoveal deep VD. There were significant negative correlations between serum ferritin and deep (whole image and parafoveal) VD (r = − 0.429, P = 0.026, and r = − 0.452, P = 0.018, respectively). Choriocapillaris VDs (whole image and foveal) showed significant negative correlations with serum ferritin levels (r = − 0.390, P = 0.044 and r = − 0.401, P = 0.038, respectively)
Conclusions
Macular microvascular changes were detected by OCTA examination in patients with TDT, mostly due to iron overload effect, as we selected patients on iron-chelating agent with the least harmful effect on the retina. The most affected layer is the DCP. Changes at the deep layer could be used as a sensitive biomarker for early macular perfusion changes in those patients.
Trial registration
Study registration number is UMIN000042657, date of registration: 2020/12/04 (retrospectively registered).






Similar content being viewed by others
Change history
11 January 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00417-022-05555-3
Abbreviations
- TI:
-
Thalassemia intermedia
- NTDT:
-
Non-transfusion-dependent thalassemia
- TM:
-
Thalassemia major
- TDT:
-
Transfusion-dependent thalassemia
- OCTA:
-
Optical coherence tomography angiography
- BCVA:
-
Best-corrected visual acuity
- LogMAR VA:
-
Logarithm of the minimum angle of resolution visual acuity
- BIO:
-
Binocular indirect ophthalmoscopy
- GAT:
-
Goldmann applanation tonometry
- CFP:
-
Color fundus photography
- SSI:
-
Signal strength index
- SPSS:
-
Statistical package for the social sciences
- SSADA:
-
Split-spectrum amplitude-decorrelation angiography
- SCP:
-
Superficial capillary plexus
- ILM:
-
Internal limiting membrane
- IPL:
-
Inner plexiform layer
- DCP:
-
Deep capillary plexus
- OPL:
-
Outer plexiform layer
- VD:
-
Vessel area density
- FAZ:
-
Foveal avascular zone
- ROI:
-
Circle region of interest
- DFP:
-
Deferiprone
- ICP:
-
Intermediate capillary plexus
References
Yang Y, Dai BT (2011) The iron overload and iron-chelating therapying of β-thalassemia J. J Pediatr Pharm 17(3):58–61
Beijing Angel Mom Charity Foundation, China Siyuan Foundation for poverty alleviation, China Philanthropy Research Institute of Beijing Normal University (2016) Blue Paper of Thalassemia in China [M]. China Social Publishing House
Pistoia L, Meloni A, Salvadori S et al (2019) Cardiac involvement by CMR in different genotypic groups of major thalassemia patients. J Blood Cells Mol Dis 77:1–7
Angastiniotis M, Modell B (1998) Global epidemiology of hemoglobin disorders. Ann N Y Acad Sci 30(850):251–269
Vichinsky EP (2005) Changing patterns of thalassemia worldwide. J Ann NY Acad Sci 1054:18–24. https://doi.org/10.1196/annals.1345.003
El Beshlawy A, Mokhtar G, Abd El Ghafar E, Abd El Dayem S, El-Sayed M, Aly A, Farok M (2008) Assessment of puberty in relation to L-carnitine and hormonal replacement therapy in β-thalassemia patients. Trop Pediatr 54(6):375–381
Viprakasit V, Ekwattanakit S (2018) Clinical classification, screening and diagnosis for thalassemia. Hematol Oncol Clin North Am 32(2):193–211
Hakeem GLA, Mousa SO, Moustafa AN, Mahgoob MH, Hassan EE (2018) Health Qual Life Outcomes. 16(1):59
Taher AT, Saliba AN (2017) Hematology Am Soc Hematol Educ Program. 2017(1):265–271
Aydinok Y, Porter JB, Piga A et al (2015) Prevalence and distribution of iron overload in patients with transfusion-dependent anemias differs across geographic regions: results from the CORDELIA study. Eur J Haematol 95(3):244–253
Blasiak J, Sklodowska A, Ulinska M, Szaflik JP (2009) Iron and age-related macular degeneration. Klin Oczna 111:174–177
Mishra AK, Tiwari A (2013) Iron overload in Beta thalassaemia major and intermedia patients. Maedica (Bucur) 8(4):328–332
Taneja R, Malik P, Sharma M, Agarwal MC (2010) Multiple transfused thalassemia major: ocular manifestations in a hospital-based population. Indian J Ophthalmol f 58:125
Bhoiwala DL, Dunaief JL (2016) Retinal abnormalities in β-thalassemia major. Surv Ophthalmol 61(1):33–50. https://doi.org/10.1016/j.survophthal.2015.08.005
Heydarian S, Jafari R, Dailami KN, Hashemi H, Jafarzadehpour E, Heirani M, Yekta A, Mahjoob M, Khabazkhoob M (2020) Ocular abnormalities in beta thalassemia patients: prevalence, impact, and management strategies. Int Ophthalmol 40(2):511–527
Song D, Dunaief JL (2013) Retinal iron homeostasis in health and disease. Front Aging Neurosci 5:24
Cossu G, Abbruzzese G, Matta G et al (2014) Efficacy and safety of deferiprone for the treatment of pantothenate kinase-associated neurodegeneration (PKAN) and neurodegeneration with brain iron accumulation (NBIA): results from a four years follow-up. Parkinsonism Relat Disord 20:651–654
Simon S, Athanasiov PA, Jain R et al (2012) Desferrioxamine related ocular toxicity: a case report. Indian J Ophthalmol 60(4):315–317
Viola F, BarteselliDell’arti GL et al (2012) Abnormal fundus autofluorescence results of patients in long-term treatment with deferoxamine. Ophthalmology 119(8):1693–1700
Olivieri NF, Nathan DG, MacMillan JH, Wayne AS, Liu PP, McGee A, Martin M, Koren G, Cohen AR (1994) Survival in medically treated patients with homozygous beta-thalassemia. N Engl J Med. 331(9):574–8. https://doi.org/10.1056/NEJM199409013310903
Belhoul KM, Bakir ML, Saned MS, Kadhim AM, Musallam KM, Taher AT (2012) Serum ferritin levels and endocrinopathy in medically treated patients with β thalassemia major. Ann Hematol 91(7):1107–1114
Bates NM, Tian J, Smiddy WE et al (2018) Relationship between the morphology of the foveal avascular zone, retinal structure, and macular circulation in patients with diabetes mellitus. Sci Rep 8:5355
Gill A, Cole ED, Novais EA et al (2017) Visualization of changes in the foveal avascular zone in both observed and treated diabetic macular edema using optical coherence tomography angiography. Int J Retina Vitreous 3:19
Spaide RF (2016) Retinal vascular cystoid macular edema: review and new theory. Retina 36:1823–1842
Couturier A, Mane V, Bonnin S et al (2015) Capillary plexus anomalies in diabetic retinopathy on optical coherence tomography angiography. Retina 35:2384–2391
Güler Kazancı E, Korkmaz MF, Can ME (2020) Optical coherence tomography angiography findings in young β-thalassemia patients. Eur J Ophthalmol 30(3):600–607
Georgalas I, Makris G, Papaconstantinou D, Petrou P, Chalkiadaki E, Droutsas K, Andreanos K, Kanakis M (2019) A pilot optical coherence tomography angiography study on superficial and deep capillary plexus foveal avascular zone in patients with beta-thalassemia major. Invest Ophthalmol Vis Sci. 60(12):3887–3896
Carraro MC, Rossetti L, Gerli GC (2001) Prevalence of retinopathy in patients with anemia or thrombocytopenia. Eur J Haematol 67:238–244
Incorvaia C, Parmeggiani F, Costagliola C, Perri P, D’Angelo S, Sebastiani A (2003) Quantitative evaluation of the retinal venous tortuosity in chronic anaemic patients affected by beta thalassaemia major. Eye (Lond) 17:324–329
Cho M, Aaker G, D’Amico DJ, Kiss S (2011) Peripheral vascular abnormalities in b-thalassemia major detected by ultra-widefield fundus imaging. Retin Cases Brief Rep 5:339–342
El-Shazly AA, Elkitkat RS, Ebeid WM, Deghedy MR (2016) Correlation between subfoveal choroidal thickness and foveal thickness in thalassemic patients. Retina 36(9):1767–1772
Ulusoy MO, Türk H, Kıvanç SA (2019) Spectral domain optical coherence tomography findings in Turkish sickle-cell disease and beta thalassemia major patients. J Curr Ophthalmol. 31(3):275–280
Haase VH (2013) Regulation of erythropoiesis by hypoxia-inducible factors. Blood Rev 27(1):41–53
Simsek A, Tekin M, Bilak S, Karadag AS, Konca C, Almis H (2016) Choroidal thickness in children with beta thalassemia major. Optom Vis Sci 93(6):600–606
Arifoglu HB, Kucuk B, Duru N et al (2018) Assessing posterior ocular structures in β-thalassemia minor. Int Ophthalmol 38:119–125
Author information
Authors and Affiliations
Contributions
HRA participated in conception and design of this work, data acquisition (OCTA examination for all participants), collection and analysis, in literature search and manuscript writing. IANO participated in data collection (ophthalmic examination for all participants), analysis and statistical analysis, and in literature search and manuscript writing. SOM participated in data collection (pediatric evaluation) and data analysis and manuscript editing. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study had gained approval from Local Research Ethics Committee, Faculty of Medicine, Minia University Hospitals. The study was conducted in accordance with the tenets of the Helsinki Declaration. Study registration number is UMIN000042657.
Informed consent
Written consent form was signed by parents or legal guardians for their child’s participation in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
AttaAllah, H.R., Mousa, S.O. & Omar, I.A.N. Macular microvascular changes in children with transfusion-dependent beta-thalassemia. Graefes Arch Clin Exp Ophthalmol 259, 3283–3293 (2021). https://doi.org/10.1007/s00417-021-05275-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05275-0