Abstract
Objective
Dyspnea can be present as non-motor symptom in patients with Parkinson’s disease (PD). Deep brain stimulation (DBS) of the subthalamic nucleus (STN) improves motor and non-motor symptoms in PD. However, new-onset dyspnea has been reported after DBS surgery. We have studied respiratory characteristics of PD patients with bilateral STN-DBS to assess the impact of DBS on pulmonary function.
Methods
STN-DBS PD patients with dyspnea after surgery (cases) were matched with STN-DBS PD patients without dyspnea (controls). Motor and pulmonary function were assessed with stimulation and without medication (on stim/off med), and without stimulation and medication (off stim/off med). Pulmonary function was investigated with spirometry and dyspnea with the Medical Research Council Dyspnea Scale (MRCDS) and the Borg Scale (BS).
Results
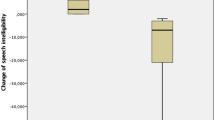
Seven cases (five men, 58.30 ± 6.70 years of age) and seven controls (six men, 61.10 ± 6.30 years of age) were enrolled. MRCDS and BS revealed the presence of dyspnea in both groups. No significant changes in pulmonary function were found in both cases and controls in on stim/off med vs. off stim/off med condition (p < 0.05), and in cases vs. controls in on stim/ off med condition (p < 0.05).
Conclusions
No impact of STN-DBS on pulmonary function was found in cases. Impaired perception of dyspnea and spread of stimulation surrounding the STN might account for new-onset dyspnea after DBS surgery. Dyspnea was detected also in controls using ad hoc questionnaires. Our findings suggest further investigation of this non-motor symptom in PD patients.

Similar content being viewed by others
References
Susan HF, Lang AE (2007) Motor and nonmotor fluctuations. In: Handbook of clinical neurology. Elsevier, Edinburgh, pp 159–184
Parshall MB, Schwartzstein RM, Adams L, Banzett RB, Manning HL, Bourbeau J et al; American Thoracic Society Committee on Dyspnea (2012) An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med 4:435–452
Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP et al (2009) The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson's disease. Mov Disord 1641–1649
Baille G, Chenivesse C, Perez T, Machuron F, Dujardin K, Devos D et al (2019) Dyspnea: an underestimated symptom in Parkinson's disease. Parkinsonism Relat Disord 60:162–166
Baille G, Perez T, Devos D, Machuron F, Dujardin K, Chenivesse C et al (2019) Dyspnea is a specific symptom in Parkinson's disease. J Parkinson’s Dis 9(4):785–791
Onodera H, Okabe S, Kikuchi Y, Tsuda T, Itoyama Y (2000) Impaired chemosensitivity and perception of dyspnea in Parkinson’s disease. Lancet 9231:739–740
Storch A, Schneider CB, Wolz M, Sturwald Y, Nebe A, Odin P et al (2013) Nonmotor fluctuations in Parkinson disease: severity and correlation with motor complications. Neurology 9:800–809
De Pandis MF, Starace A, Stefanelli F, Marruzzo P, Meoli I, De Simone G et al (2002) Modification of respiratory function parameters in patients with severe Parkinson’s disease. Neurol Sci Suppl 2:69–70
Herer B, Arnulf I (2001) Housset B Effects of levodopa on pulmonary function in Parkinson’s disease. Chest 2:387–393
Guedes LU, Rodrigues JM, Fernandes AA, Cardoso FE, Parreira VF (2012) Respiratory changes in Parkinson’s disease may be unrelated to dopaminergic dysfunction. Arq Neuropsiquiatr 11:847–851
Vijayan S, Singh B, Ghosh S, Stell R, Mastaglia FL (2020) Brainstem ventilatory dysfunction: a plausible mechanism for dyspnea in Parkinson's Disease? Mov Disord. https://doi.org/10.1002/mds.27932(epub ahead of print, review)
Pal PK, Sathyaprabha TN, Tuhina P et al (2007) Pattern of subclinical pulmonary dysfunctions in Parkinson's disease and the effect of levodopa. Mov Disord 22(3):420–424
Rice JE, Antic R, Thompson PD (2002) Disordered respiration as a levodopa-induced dyskinesia in Parkinson’s disease. Mov Disord 3:524–527
Dafsari HS, Silverdale M, Strack M, Rizos A, Ashkan K, Mahlstedt P et al (2018) EUROPAR and the IPMDS Non Motor PD Study Group. Nonmotor symptoms evolution during 24 months of bilateral subthalamic stimulation in Parkinson's disease. Mov Disord 33(3):421–430
Jiang L, Poon WS, Moro E, Xian W, Yang C, Zhu XL et al (2017) Early versus late application of subthalamic deep brain stimulation to Parkinson's disease patients with motor complications (ELASS): protocol of a multicentre, prospective and observational study. BMJ Open 16 7(11):e018610
Hyam JA, Brittain JS, Paterson DJ, Davies RJ, Aziz TZ, Green AL (2012) Controlling the lungs via the brain: a novel neurosurgical method to improve lung function in humans. Neurosurgery 70(2):469–478
Chalif JI, Sitsapesan HA, Pattinson KT, Herigstad M, Aziz TZ, Green AL (2014) Dyspnea as a side effect of subthalamic nucleus deep brain stimulation for Parkinson's disease. Respir Physiol Neurobiol 192:128–133
Kawaguchi M, Samura K, Miyagi Y, Okamoto T, Yamasaki R, Sakae N et al (2020) The effects of chronic subthalamic stimulation on nonmotor symptoms in advanced Parkinson's disease, revealed by an online questionnaire program. Acta Neurochir (Wien) 162(2):247–255
Kumar R, Lozano AM, Kim YJ et al (1998) Double-blind evaluation of subthalamic nucleus deep brain stimulation in advanced Parkinson's disease. Neurology 51(3):850–855
Fahn S, Elton RL, Committee motUd (1987) Unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB (eds) Recent developments in Parkinson’s disease. MacMillan Health Care Information, Florham Park, pp 153–164
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA (1999) Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54:581–586
Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Papathanasiou JV, Ilieva E, Marinov B (2013) Six-minute walk test: an effective and necessary tool in modern cardiac rehabilitation. Hellenic J Cardiol 54:126–130
Chapman KR, Cox G, Davis L, Gottschalk R, Ho B, Nedar A, et al. (2014) Independent health facilities, clinical practice parameters and facility standards, pulmonary function facilities, 4th edn. College of Physicians and Surgeons of Ontario, Toronto
Yanase M, Kataoka H, Kawahara M et al (2008) Fixed epiglottis associated with subthalamic nucleus stimulation in Parkinson's disease. J Neurol Neurosurg Psychiatry 79(3):332–333
Weiner P, Inzelberg R, Davidovich A, Nisipeanu P, Magadle R, Berar-Yanay N, Carasso RL (2002) Respiratory muscle performance and the Perception of dyspnea in Parkinson’s disease. Can J Neurol Sci 29:68–72
Komiya H, Kimura K, Kishida H, Kawasaki T, Hamada K, Koizumi H, Ueda N, Tanaka F (2019) Adjustment of subthalamic deep brain stimulation parameters improves wheeze and dyspnea in Parkinson's disease. Front Neurol 13:10–1317
Temperli P, Ghika J, Villemure JG, Burkhard PR, Bogousslavsky J, Vingerhoets FJ (2003) How do parkinsonian signs return after discontinuation of subthalamic DBS? Neurology 60:78–81
Acknowledgements
The authors thank Dr. Kenneth R. Chapman, MD, Asthma and Airway Centre, Toronto Western Hospital, UHN, University of Toronto, Toronto, Ontario, Canada, for his help in supervising respiratory data collection. The authors also thank Christopher Meaney, Toronto Western Hospital, UHN, University of Toronto, Toronto, Ontario, Canada, for his help in statistical analysis of data
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Sara Meoni reports no disclosures. Ana C. Bradi reports no disclosures. Pettarusp Wadia reports no disclosures. Yu-Yan Poon reports no disclosures. Elena Moro has received honoraria from Abbott, Medtronic and Newronika for consulting service and lecturing.
Ethical approval
The study was approved by the Research Ethics Board of the University Health Network, Toronto, Ontario, Canada. All subjects could understand the details of the study and gave informed consent to participate.
Rights and permissions
About this article
Cite this article
Meoni, S., Bradi, A.C., Wadia, P. et al. Dyspnea after subthalamic deep brain stimulation in Parkinson’s disease: a case–control study. J Neurol 267, 3054–3060 (2020). https://doi.org/10.1007/s00415-020-09976-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09976-0