Abstract
Background and purpose
The significance of white matter hyperintensities (WMHs) in the setting of mechanical thrombectomy (MT) remains poorly documented. We assessed whether pre-existing WMHs burden was associated with baseline clinical and imaging factors and neurological outcome in patients undergoing MT.
Methods
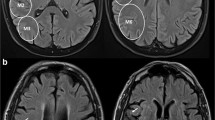
This retrospective single-center study included consecutive acute ischemic stroke (AIS) patients with stroke due to large vessel occlusion treated with MT. WMHs were assessed on baseline T2 fluid-attenuated inversion recovery magnetic resonance imaging. Neurological outcome was assessed at day 90 by the modified Rankin Scale (mRS). We analyzed the association between WMH burden and clinical and imaging factors by univariate and multivariate logistic regression analyses.
Results
Between July 2013 and June 2019, 293 patients with anterior circulation AIS met the inclusion criteria. WMHs burden was not associated to baseline NIHSS score severity (OR 0.89, 95% CI 0.54–1.49, p = 0.66), poor collateral status, Higashida score < 3 (OR 1.5 95% CI 0.62–3.56, p = 0.36), higher DWI volume (OR 0.69, 95% CI 0.41–1.15, p = 0.16) or to a lower recanalization rate, TICI 0/2a (OR 0.98 95% CI 0.56–1.69, p = 0.95). WMHs severity did not influence the risk of parenchymal hemorrhage (OR 0.97 95% 0.26–3, p = 0.96). WMHs burden was not an independent predictor of poor outcome in multivariate analysis. The rate of futile recanalization in patients with TICI grades 2b and 3 according to mRs score at 3 months was not influenced by WMHs burden.
Conclusions
WMHs burden does not seem to influence clinical outcome and imaging parameters in patients treated by MT.

Similar content being viewed by others
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. HERMES collaborators. Lancet 387:1723–1731
Campbell BCV, Ma H, Ringleb PA, Parsons MW, Churilov L, Bendszus M, Levi CR et al. EXTEND, ECASS-4, and EPITHET Investigators (2019) Extending thrombolysis to 4·5-9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet 394(10193):139–147
Kidwell CS (2013) MRI biomarkers in acute ischemic stroke: a conceptual framework and historical analysis. Stroke 2:570–578
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, DAWN Trial Investigators et al (2018) Thrombectomy 6–24 h after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, DEFUSE 3 Investigators et al (2018) Thrombectomy for stroke at 6–16 h with selection by perfusion imaging. N Engl J Med 378:708–718
Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, WAKE-UP Investigators et al (2018) MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med 7:611–622
Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM et al (2018) Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. HERMES collaborators. Lancet Neurol 10:895–904
Shi ZS, Loh Y, Liebeskind DS, Saver JL, Gonzalez NR, Tateshima S et al (2012) Leukoaraiosis predicts parenchymal hematoma after mechanical thrombectomy in acute ischemic stroke. Stroke 43:1806–1811
Henninger N, Lin E, Haussen DC, Lehman LL, Takhtani D, Selim M et al (2013) Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke 44:61–67
Giurgiutiu DV, Yoo AJ, Fitzpatrick K, Chaudhry Z, Leslie-Mazwi T, Schwamm LH (2015) Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerv Surg 5:326–330
Ishikawa M, Sugawara H, Nagai M, Kusaka G, Tanaka Y, Naritaka H (2017) Collateral flow and white matter disease in patients with internal carotid artery occlusion. Eur Neurol 1–2:56–65
Ay H, Arsava EM, Rosand J et al (2008) Severity of leukoaraiosis and susceptibility to infarct growth in acute stroke. Stroke 39:1409–1413
Atchaneeyasakul K, Leslie-Mazwi T, Donahue K, Giese AK, Rost NS (2017) White matter hyperintensity volume and outcome of mechanical thrombectomy with stentriever in acute ischemic stroke. Stroke 10:2892–2894
Boulouis G, Bricout N, Benhassen W, Ferrigno M, Turc G, Bretzner M et al (2019) White matter hyperintensity burden in patients with ischemic stroke treated with thrombectomy. Neurology. 93(16):e1498–e1506
Gilberti N, Gamba M, Premi E et al (2017) Leukoaraiosis is a predictor of futile recanalization in acute ischemic stroke. J Neurol 264:448–452
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy: ASPECTS Study Group: Alberta Stroke Programme Early CT Score. Lancet 355:1670–1674
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am. J. Roentgenol 149:351–356
Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J et al (2003) Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 34:e109–e137
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 9136:1245–1251
Rocha M, Jovin TG (2017) Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke 48:2621–2627
Liebeskind DS (2003) Collateral circulation. Stroke 34:2279–2284
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM et al (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials; HERMES collaborators. Lancet 10029:1723–1731
Munoz Maniega S, Chappell FM, Valdes Hernandez MC et al (2017) Integrity of normal-appearing white matter: influence of age, visible lesion burden and hypertension in patients with small-vessel disease. J Cereb Blood Flow Metab 37:644–656
Wardlaw JM, Makin SJ, Valdés Hernández MC et al (2017) Blood–brain barrier failure as a core mechanism in cerebral small vessel disease and dementia: evidence from a cohort study. Alzheimers Dement 13:634–643
van Leijsen EMC, Bergkamp MI, van Uden IWM et al (2018) Progression of white matter hyperintensities preceded by heterogeneous decline of microstructural integrity. Stroke 49:1386–1393
Wardlaw JM, Smith C, Dichgans M (2019) Small vessel disease: mechanisms and clinical implications. Lancet Neurol 18(7):684–696
Miyao S, Takano A, Teramoto J, Takahashi A (1992) Leukoaraiosis in relation to prognosis for patients with lacunar infarction. Stroke 10:1434–1438
Jeong SH, Ahn SS, Baik M, Kim KH, Yoo J, Kim K, Lee HS et al (2018) Impact of white matter hyperintensities on the prognosis of cryptogenic stroke patients. PLoS One 13(4):e0196014
Choi KH, Kim JH, Kang KW, Kim JT, Choi SM, Lee SH et al (2018) Impact of microbleeds on outcome following recanalization in patients with acute ischemic stroke. Stroke. https://doi.org/10.1161/strokeaha.118.023084
Rudilosso S, Laredo C, Vivancos C, Urra X, Llull L, Renú A et al (2019) Leukoaraiosis may confound the interpretation of CT perfusion in patients treated with mechanical thrombectomy for acute ischemic stroke. AJNR Am J Neuroradiol 8:1323–1329
Funding
This work was supported by the RHU MARVELOUS (ANR-16-RHUS-0009) of l’Université Claude Bernard Lyon 1 (UCBL), within the program “Investissements d’Avenir” operated by the French National Research Agency (ANR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflict of interest and no disclosure.
Ethical standards
This research was conducted according to the ethical standards issued by the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Mechtouff, L., Nighoghossian, N., Amaz, C. et al. White matter burden does not influence the outcome of mechanical thrombectomy. J Neurol 267, 618–624 (2020). https://doi.org/10.1007/s00415-019-09624-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09624-2