Abstract
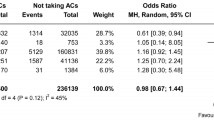
Since there are contradictory data regarding the association of antiplatelet pretreatment (AP) with safety and efficacy outcomes of intravenous thrombolysis (IVT) for acute ischemic stroke (AIS), we conducted a systematic review and meta-analysis of available randomized-controlled clinical trials (RCTs) to investigate the association of AP with outcomes of AIS patients treated with intravenous alteplase. The outcome events of interest included symptomatic intracranial hemorrhage (sICH), fatal ICH, complete recanalization (CR), 3-month favorable functional outcome (FFO, mRS score 0–1), 3-month functional independence (FI, mRS score 0–2), and mortality. The corresponding odds ratios (ORs) were calculated for all the outcome events using random-effects model. The adjusted age and admission NIHSS OR (ORadjusted) were also estimated for all available outcomes. We included 7 RCTs (4376 patients, 33.7% with AP). In unadjusted analyses, AP was associated with higher likelihood of sICH (OR = 1.89, 95% CI 1.40–2.56), death (OR = 1.59, 95% CI 1.24–2.03), and lower likelihood of 3-month FI (OR = 0.69, 95% CI 0.56–0.85). No association was detected between AP and fatal ICH (OR = 1.53, 95% CI 0.75–3.15), 3-month FFO (OR = 0.79, 95% CI 0.58–1.07), and CR (OR = 0.64, 95% CI 0.04–11.66). After adjustment for age and admission stroke severity, AP was not related to sICH (ORadjusted = 1.67, 95% CI 0.75–3.72), 3-month FI (ORadjusted = 0.88, 95% CI 0.54–1.42), or death (ORadjusted = 1.01, 95% CI 0.55–1.86) in adjusted analyses. In conclusion, after adjusting for confounders, AP was not associated with a higher risk of sICH and worse 3-month functional outcome in AIS treated with intravenous alteplase. Antiplatelet intake prior to tPA-bolus should not be used as a reason to withhold or lower alteplase dose in AIS patients treated with IVT.




Similar content being viewed by others
References
Jauch EC, Saver JL, Adams HP Jr et al (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44:870–947
Hacke W, Lichy C (2008) Thrombolysis for acute stroke under antiplatelet therapy: safe enough to be beneficial? Nat Clin Pract Neurol 4:474–475
Uyttenboogaart M, Luijckx GJ (2010) Intravenous thrombolysis for patients with ischaemic stroke on antiplatelet therapy: a blessing in disguise? Eur J Neurol 17:177–178
Zinkstok SM, Beenen LF, Majoie CB, Marquering HA, de Haan RJ, Roos YB (2014) Early deterioration after thrombolysis plus aspirin in acute stroke: a post hoc analysis of the Antiplatelet Therapy in Combination with Recombinant t-PA Thrombolysis in Ischemic Stroke trial. Stroke 45:3080–3082
Anderson CS, Robinson T, Lindley RI et al (2016) Low-dose versus standard-dose intravenous alteplase in acute ischemic stroke. N Engl J Med 374:2313–2323
Robinson T, Lindley R, Lavados P et al (2016) Benefits and risks of low versus standard-dose alteplase in patients with prior antiplatelet therapy: the ENCHANTED trial (ESOC6-1434). Eur Stroke J 1:711
Liberati A, Altman DG, Tetzlaff J et al (2009) The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Tsivgoulis G, Zand R, Katsanos AH et al (2016) Risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis in patients with acute ischemic stroke and high cerebral microbleed burden: a meta-analysis. JAMA Neurol 73:675–683
Tsivgoulis G, Zand R, Katsanos AH et al (2015) Safety and outcomes of intravenous thrombolysis in dissection-related ischemic stroke: an international multicenter study and comprehensive meta-analysis of reported case series. J Neurol 262:2135–2143
Tsivgoulis G, Ribo M, Rubiera M et al (2013) Real-time validation of transcranial Doppler criteria in assessing recanalization during intra-arterial procedures for acute ischemic stroke: an international, multicenter study. Stroke 44:394–400
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Bero LA (2013) Why the Cochrane risk of bias tool should include funding source as a standard item [editorial]. Cochrane Database Syst Rev 12:000075
Strbian D, Seiffge DJ, Breuer L et al (2013) Validation of the DRAGON score in 12 stroke centers in anterior and posterior circulation. Stroke 44:2718–2721
Strbian D, Engelter S, Michel P et al (2012) Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol 71:634–641
Tsivgoulis G, Katsanos AH, Mavridis D, Magoufis G, Arthur A, Alexandrov AV (2016) Mechanical thrombectomy improves functional outcomes independent of pretreatment with intravenous thrombolysis. Stroke 47:1661–1664
Deeks JJ, Higgins JP, Altman DG (2008) Chapter 9: Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions website. http://handbook.cochrane.org/chapter_9/9_analysing_data_and_undertaking_meta_analyses.htm. Updated March 2011. Accessed 4 Feb 2014
Sterne JA, Sutton AJ, Ioannidis JP et al (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002
Tsivgoulis G, Zand R, Katsanos AH et al (2015) Safety of intravenous thrombolysis in stroke mimics: prospective 5-year study and comprehensive meta-analysis. Stroke 46:1281–1287
Goyal N, Tsivgoulis G, Zand R et al (2015) Systemic thrombolysis in acute ischemic stroke patients with unruptured intracranial aneurysms. Neurology 85:1452–1458
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Alexandrov AV, Molina CA, Grotta JC et al (2004) Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 351:2170–2178
Hacke W, Kaste M, Fieschi C et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 352:1245–1251
Hacke W, Kaste M, Bluhmki E et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359:1317–1329
Sandercock P, Wardlaw JM, Lindley RI et al (2012) The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 379:2352–2363
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Molina CA, Barreto AD, Tsivgoulis G et al (2009) Transcranial ultrasound in clinical sonothrombolysis (TUCSON) trial. Ann Neurol 66:28–38
Larrue V, von Kummer R, Müller A, Bluhmki E (2001) Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke 32:438–441
Bluhmki E, Chamorro A, Dávalos A et al (2009) Stroke treatment with alteplase given 3.0–4.5 h after onset of acute ischaemicstroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 8:1095–1102
Lindley RI, Wardlaw JM, Whiteley WN et al (2015) Alteplase for acute ischemic stroke: outcomes by clinically important subgroups in the Third International Stroke Trial. Stroke 46:746–756
Dachs RJ, Burton JH, Joslin J (2008) A user’s guide to the NINDS rt-PA stroke trial database. PLoS Med 5:e113
Saqqur M, Tsivgoulis G, Molina CA et al (2008) Symptomatic intracerebral hemorrhage and recanalization after IV rt-PA: a multicenter study. Neurology 71:1304–1312
Chen S, Lu X, Zhang W et al (2016) Does prior antiplatelet treatment increase the risk of hemorrhagic transformation and unfavorable outcome on day 90 after intravenous thrombolysis in acute ischemic stroke patients? J Stroke Cerebrovasc Dis 25:1366–1370
Enomoto Y, Yoshimura S, Egashira Y, Yamagami H, Sakai N (2016) The risk of intracranial hemorrhage in japanese patients with acute large vessel occlusion; subanalysis of the RESCUE-Japan registry. J Stroke Cerebrovasc Dis 25:1076–1080
Dorado L, Millán M, de la Ossa NP et al (2010) Influence of antiplatelet pre-treatment on the risk of intracranial haemorrhage in acute ischaemic stroke after intravenous thrombolysis. Eur J Neurol 17:301–306
Meseguer E, Labreuche J, Guidoux C et al (2015) Outcomes after stroke thrombolysis according to prior antiplatelet use. Int J Stroke 10:163–169
Ibrahim MM, Sebastian J, Hussain M et al (2010) Does current oral antiplatelet agent or subtherapeutic anticoagulation use have an effect on tissue-plasminogen-activator-mediated recanalization rate in patients with acute ischemic stroke? Cerebrovasc Dis 30:508–513
Luo S, Zhuang M, Zeng W, Tao J (2016) Intravenous thrombolysis for acute ischemic stroke in patients receiving antiplatelet therapy: a systematic review and meta-analysis of 19 studies. J Am Heart Assoc. doi:10.1161/JAHA.116.003242
Pan X, Zhu Y, Zheng D, Liu Y, Yu F, Yang J (2015) Prior antiplatelet agent use and outcomes after intravenous thrombolysis with recombinant tissue plasminogen activator in acute ischemic stroke: a meta-analysis of cohort studies and randomized controlled trials. Int J Stroke 10:317–323
Guyatt GH, Sackett DL, Sinclair JC, Hayward R, Cook DJ, Cook RJ (1995) Users’ guides to the medical literature. IX. A method for grading health care recommendations. Evidence-Based Medicine Working Group. JAMA 274:1800–1804
Pan Y, Chen Q, Liao X et al (2015) Preexisting dual antiplatelet treatment increases the risk of post-thrombolysis intracranial hemorrhage in Chinese stroke patients. Neurol Res 37:64–68
Diedler J, Ahmed N, Sykora M et al (2010) Safety of intravenous thrombolysis for acute ischemic stroke in patients receiving antiplatelet therapy at stroke onset. Stroke 41:288–294
Author information
Authors and Affiliations
Contributions
Conception and design of the study: GT, AHK, PDS, and AVA. Acquisition of data: GT and AHK. Analysis of data: GT and AHK. Drafting the manuscript: GT, AHK, RZ, VKS, MK, SG, ED, AWA, PDM, PDS, and AVA.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Sources of funding
Dr. Georgios Tsivgoulis has been supported by European Regional Development Fund—Project FNUSA-ICRC (No. CZ.1.05/1.1.00/02.0123).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tsivgoulis, G., Katsanos, A.H., Zand, R. et al. Antiplatelet pretreatment and outcomes in intravenous thrombolysis for stroke: a systematic review and meta-analysis. J Neurol 264, 1227–1235 (2017). https://doi.org/10.1007/s00415-017-8520-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8520-1