Abstract
Purpose
Chronic rhinosinusitis (CRS) disease burden is associated with pulmonary status in asthmatic CRS patients. Asthma-related emergency department (ED) usage is a predictor of asthma-related mortality. We sought to determine whether measures of CRS disease burden are associated with asthma-related ED usage.
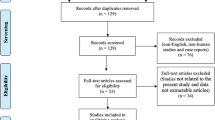
Methods
We prospectively recruited 263 asthmatic CRS patients for this cross-sectional study. CRS burden was measured using the 22-item Sinonasal Outcome Test (SNOT-22), and patient-reported CRS-related antibiotic usage and CRS-related oral corticosteroids usage over the preceding year. Asthma-related ED visits over the prior year were also assessed.
Results
Of all participants, 18.6% had at least 1 asthma-related ED visit (mean 0.3 ED visits for the whole cohort). Asthma-related ED usage was associated with SNOT-22 score [adjusted rate ratio (RR) = 1.02, 95% CI 1.01–1.03, p = 0.040] and CRS-related oral corticosteroids usage in the past year (RR = 1.52, 95% CI 1.26–1.83, p < 0.001). From the SNOT-22 score, asthma-related ED usage was only associated with the nasal subdomain score (RR = 1.08, 95% CI 1.03–1.13, p = 0.001). These measures of CRS disease burden could be used with good sensitivity and specificity to detect patients with asthma-related ED usage in the past year, the majority of whom were undertreated for their asthma.
Conclusions
Measures of CRS disease burden are associated with and can be used to detect, patients having asthma-related ED usage. These results further solidify the connection between CRS and asthma disease courses, and also present an opportunity to use CRS disease burden as a tool for identifying—and implementing greater treatment of—patients at highest risk for asthma-related mortality.
Similar content being viewed by others
References
Fokkens WJ, Lund VJ, Mullol J et al (2012) European position paper on rhinosinusitis and nasal polyps 2012. Rhinol Suppl 23:298
Orlandi RR, Kingdom TT, Hwang PH et al (2016) International consensus statement on allergy and rhinology: rhinosinusitis. Int Forum Allergy Rhinol 6(Suppl 1):S209
Campbell AP, Phillips KM, Hoehle LP et al (2017) Depression symptoms and lost productivity in chronic rhinosinusitis. Ann Allergy Asthma Immunol 118:286–289
Hoehle LP, Phillips KM, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2016) Symptoms of chronic rhinosinusitis differentially impact general health-related quality of life. Rhinology 54:316–322
Phillips KM, Hoehle LP, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2017) Acute exacerbations mediate quality of life impairment in chronic rhinosinusitis. J Allergy Clin Immunol Pract 5:422–426
Speth MM, Hoehle LP, Phillips KM, Caradonna DS, Gray ST, Sedaghat AR (2018) Changes in chronic rhinosinusitis symptoms differentially associate with improvement in general health-related quality of life. Ann Allergy Asthma Immunol 121:195–199
Sedaghat AR, Hoehle LP, Gray ST (2018) Chronic rhinosinusitis control from the patient and physician perspectives. Laryngoscope Investig Otolaryngol 3:419–433
Banoub RG, Phillips KM, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2018) Relationship between chronic rhinosinusitis exacerbation frequency and asthma control. Laryngoscope 128:1033–1038
Phillips KM, Hoehle LP, Bergmark RW et al (2017) Chronic rhinosinusitis severity is associated with need for asthma-related systemic corticosteroids. Rhinology 55:211–217
Phillips KM, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2016) Association of severity of chronic rhinosinusitis with degree of comorbid asthma control. Ann Allergy Asthma Immunol 117:651–654
Phillips KM, Bergmark RW, Hoehle LP, Caradonna DS, Gray ST, Sedaghat AR (2018) Chronic rhinosinusitis exacerbations are differentially associated with lost productivity based on asthma status. Rhinology 56:323–329
Phillips KM, Talat R, Caradonna DS, Gray ST, Sedaghat AR (2019) Quality of life impairment due to chronic rhinosinusitis in asthmatics is mediated by asthma control. Rhinology 57:430–435
Jalaludin BB, Smith MA, Chey T, Orr NJ, Smith WT, Leeder SR (1999) Risk factors for asthma deaths: a population-based, case-control study. Aust NZ J Public Health 23:595–600
To T, Zhu J, Williams DP et al (2016) Frequency of health service use in the year prior to asthma death. J Asthma 53:505–509
Reddel HK, Taylor DR, Bateman ED et al (2009) An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 180:59–99
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS et al (2015) Clinical practice guideline (update): adult sinusitis. Otolaryngology–head and neck surgery. Off J Am Acad Otolaryngol Head Neck Surg 152:S39
Hoehle LP, Phillips KM, Caradonna DS, Gray ST, Sedaghat AR (2018) A contemporary analysis of clinical and demographic factors of chronic rhinosinusitis patients and their association with disease severity. Ir J Med Sci 187:215–221
Phillips KM, Hoehle L, Bergmark RW, Caradonna DS, Gray ST, Sedaghat AR (2017) Reversal of smoking effects on chronic rhinosinusitis after smoking cessation. Otolaryngol Head Neck Surg 157:737–742
Yamasaki A, Hoehle LP, Phillips KM et al (2018) Association between systemic antibiotic and corticosteroid use for chronic rhinosinusitis and quality of life. Laryngoscope 128:37–42
Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP (2009) Psychometric validity of the 22-item sinonasal outcome test. Clinical otolaryngology: official journal of ENT-UK. Off J Nether Soc Oto-Rhino-Laryngol Cervico-Facial Surg 34:447–454
Sedaghat AR, Gray ST, Caradonna SD, Caradonna DS (2015) Clustering of chronic rhinosinusitis symptomatology reveals novel associations with objective clinical and demographic characteristics. Am J Rhinol Allergy 29:100–105
Feng AL, Wesely NC, Hoehle LP et al (2017) A validated model for the 22-item sino-nasal outcome test subdomain structure in chronic rhinosinusitis. Int Forum Allergy Rhinol 7:1140–1148
Schatz M, Sorkness CA, Li JT et al (2006) Asthma control test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol 117:549–556
Team RDC (2011) R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria
Robin X, Turck N, Hainard A et al (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform 12:77
Jarvis D, Newson R, Lotvall J et al (2012) Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy 67:91–98
Stevens WW, Peters AT, Suh L et al (2015) A retrospective, cross-sectional study reveals that women with CRSwNP have more severe disease than men. Immun Inflamm Dis 3:14–22
EPR-3. NAEPP expert panel report 3: guidelines for the diagnosis and treatment of asthma. Bethesda (MD): US Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute 2007
Cao PP, Wang ZC, Schleimer RP, Liu Z (2019) Pathophysiologic mechanisms of chronic rhinosinusitis and their roles in emerging disease endotypes. Ann Allergy Asthma Immunol 122:33–40
Harlin SL, Ansel DG, Lane SR, Myers J, Kephart GM, Gleich GJ (1988) A clinical and pathologic study of chronic sinusitis: the role of the eosinophil. J Allergy Clin Immunol 81:867–875
ten Brinke A, Grootendorst DC, Schmidt JT et al (2002) Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol 109:621–626
Alobid I, Benitez P, Bernal-Sprekelsen M, Guilemany JM, Picado C, Mullol J (2005) The impact of asthma and aspirin sensitivity on quality of life of patients with nasal polyposis. Qual Life Res 14:789–793
Batra PS, Kern RC, Tripathi A et al (2003) Outcome analysis of endoscopic sinus surgery in patients with nasal polyps and asthma. Laryngoscope 113:1703–1706
Jankowski R, Moneret-Vautrin DA, Goetz R, Wayoff M (1992) Incidence of medico-surgical treatment for nasal polyps on the development of associated asthma. Rhinology 30:249–258
Slavin RG (1992) Asthma and sinusitis. J Allergy Clin Immunol 90:534–537
Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza DC (1999) Long-term impact of functional endoscopic sinus surgery on asthma. Otolaryngology–head and neck surgery. Off J Am Acad Otolaryngol-Head Neck Surg 121:66–68
Lund VJ (1999) The effect of sinonasal surgery on asthma. Allergy 54(Suppl 57):141–145
Schlosser RJ, Smith TL, Mace J, Soler ZM (2017) Asthma quality of life and control after sinus surgery in patients with chronic rhinosinusitis. Allergy 72:483–491
Bresciani M, Paradis L, Des Roches A et al (2001) Rhinosinusitis in severe asthma. J Allergy Clin Immunol 107:73–80
Pearlman AN, Chandra RK, Chang D et al (2009) Relationships between severity of chronic rhinosinusitis and nasal polyposis, asthma, and atopy. Am J Rhinol Allergy 23:145–148
Campbell AP, Phillips KM, Hoehle LP et al (2018) Association between asthma and chronic rhinosinusitis severity in the context of asthma control. Otolaryngol Head Neck Surg 158:386–390
Johnson LH, Chambers P, Dexheimer JW (2016) Asthma-related emergency department use: current perspectives. Open Access Emerg Med 8:47–55
Nath JB, Hsia RY (2015) Children’s emergency department use for asthma, 2001–2010. Acad Pediatr 15:225–230
Bergmark RW, Hoehle LP, Chyou D et al (2018) Association of socioeconomic status, race and insurance status with chronic rhinosinusitis patient-reported outcome measures. Otolaryngol Head Neck Surg 158:571–579
Bergmark RW, Ishman SL, Phillips KM, Cunningham MJ, Sedaghat AR (2018) Emergency department use for acute rhinosinusitis: insurance dependent for children and adults. Laryngoscope 128:299–303
Bergmark RW, Sedaghat AR (2017) Disparities in health in the United States: an overview of the social determinants of health for otolaryngologists. Laryngoscope Investig Otolaryngol 2:187–193
Acknowledgements
The authors gratefully acknowledge the contribution of the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no potential conflicts or financial relationships.
Ethical approval
This study and its design was approved by the institutional human studies committee.
Informed consent
All patients provided informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gleadhill, C., Speth, M.M., Gengler, I. et al. Chronic rhinosinusitis disease burden is associated with asthma-related emergency department usage. Eur Arch Otorhinolaryngol 278, 93–99 (2021). https://doi.org/10.1007/s00405-020-06259-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-06259-2