Abstract
Purpose
Treatment guidelines have not been established for unknown primary head and neck squamous cell carcinoma (SCC). For these patients, chemoradiotherapy (CRT) can provide a better prognosis than that for patients with other head and neck cancers. The presence of HPV in the tumor is associated with a better outcome. However, not all patients with HPV-positive unknown primary head and neck SCC experience good treatment outcomes in actual clinical settings.
Methods
We thus retrospectively determined the Ki-67 proliferation index and p16 expression status to assess the associations of these parameters with treatment outcomes of patients with unknown primary head and neck SCC.
Results
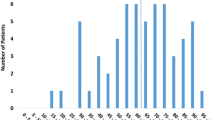
The subjects were 13 patients who underwent CRT after surgery or excision biopsy between 1999 and 2016. The 2- and 5-year overall survival (OS) rate was 76.9% and 68.4%, respectively. The prognostic factor was age. There was no significant difference in survival between patients with a high Ki-67 vs. low Ki-67 or between patients with p16-positive vs. p16-negative metastases OS. However, all p16-positive patients with low Ki-67 showed good locoregional control.
Conclusions
The combination of ki67 expression and p16 expression status may allow prediction of local control more accurately than p16 expression status alone.



Similar content being viewed by others
References
Demiroz C, Vainshtein JM, Koukourakis GV et al (2014) Head and neck squamous cell carcinoma of unknown primary: neck dissection and radiotherapy or definitive radiotherapy. Head Neck 36:1589–1595. https://doi.org/10.1002/hed.23479
Mirghani H, Amen F, Tao Y et al (2015) Increased radiosensitivity of HPV-positive head and neck cancers: molecular basis and therapeutic perspectives. Cancer Treat Rev 41:844–852. https://doi.org/10.1016/j.ctrv.2015.10.001
Fakhry C, Westra WH, Li S et al (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100:261–269. https://doi.org/10.1093/jnci/djn011
Kofler B, Laban S, Busch CJ et al (2014) New treatment strategies for HPV-positive head and neck cancer. Eur Arch Otorhinolaryngol 271:1861–1867. https://doi.org/10.1007/s00405-013-2603-0
Kimple RJ, Harari PM (2014) Is radiation dose reduction the right answer for HPV-positive head and neck cancer? Oral Oncol 50:560–564. https://doi.org/10.3978/j.issn.2305-5839.2015.01.37
Patel RS, Clark J, Wyten R et al (2007) Squamous cell carcinoma from an unknown head and neck primary site: a “selective treatment” approach. Arch Otolaryngol Head Neck Surg 133:1282–1287
Cerezo L, Raboso E, Ballesteros AI (2011) Unknown primry cancer of the head and neck:a multidisciplinary approach. Clin Transl Oncol 13:88–97. https://doi.org/10.1007/s12094-011-0624-y
Boscolo-Rizzo P, Gava A et al (2007) Carcinoma metastatic to cervical lymph nodes from an occult primary tumor: the outcome after combined-modality therapy. Ann Surg Oncol 14:1575–1582
Strojan P, Ferlito A, Lanqendijk JA et al (2013) Contemporary management of lymph node metastases from an unknown primary to the neck:II. a review of therapeutic options. Head Neck 35:286–293. https://doi.org/10.1002/hed.21899
Werner JA, Dünne AA (2001) Value of neck dissection in patients with squamous cell carcinoma of unknown primary. Onkologie 24:16–20
Grau C, Johansen LV, Jakobsen J et al (2000) Cervical lymph node metastases from unknown primary tumors. Results from a national survey by the Danish Society for Head and Neck Oncology. Radiother Oncol 55:121–129
Argiris A, Smith SM, Stenson K et al (2003) Concurrent chemoradiotherapy for N2 or N3 squamous cell carcinoma of the head and neck from an occult primary. Ann Oncol 14:1306–1311
Nieder C, Ang KK (2002) Cervical lymph node metastases from occult squamous cell carcinoma. Curr Treat Options Oncol 3:33–40
Ligey A, Gentil J, Créhange G et al (2009) Impact of target volumes and radiation technique on loco-regional control and survival for patients with unilateral cervical lymph node metastases from an unknown primary. Radiother Oncol 93:483–487. https://doi.org/10.1016/j.radonc.2009.08.027
Chen AM, Meshman J, Hsu S et al (2018) Oropharynx-directed ipsilateral irradiation for p16-positive squamous cell carcinoma involving the cervical lymph nodes of unknown primary origin. Head Neck 40:227–232. https://doi.org/10.1002/hed.24906
Dixon PR, Au M, Hosni A et al (2016) Impact of p16 expression, nodal status, and smoking on oncologic outcomes of patients with head and neck unknown primary squamous cell carcinoma. Head Neck 38:1347–1353. https://doi.org/10.1002/hed.24441
Straetmans J, Vent J, Lacko M et al (2015) Management of neck metastases of unknown primary origin united in two European centers. Eur Arch Otorhinolaryngol 272:195–205
Szentkuti G, Danos K, Brauswetter D et al (2015) Correlations between prognosis and regional biomarker profiles in head and neck squamous cell carcinomas. Pathol Oncol Res 21:643–650. https://doi.org/10.1007/s12253-014-9869-4
Gioacchini FM, Alicandri-Ciufelli M, Magliulo G et al (2015) The clinical relevance of Ki-67 expression in laryngeal squamous cell carcinoma. Eur Arch Otorhinolaryngol 272:1569–1576. https://doi.org/10.1007/s00405-014-3117-0
National Cancer Institute Common terminology criteria for adverse events v4.0 (CTCAE) (2016) http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcae_4_with_lay_terms.pdf. Accessed 12 November 2017
RTOG 1016 Protocol Information (2016) Phase III Trial of Radiotherapy Plus Cetuximab Versus Chemoradiotherapy in HPV-Associated Oropharynx Cancer Radiation Therapy Oncology Group. https://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1016. Accessed 11 May 2018
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, Westra WH, Chung CH, Jordan RC, Lu C, Kim H, Axelrod R, Silverman CC, Redmond KP, Gillison ML (2012) Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 363:24–35. https://doi.org/10.1056/NEJMoa0912217
Park GC, Lee M, Roh JL et al (2012) Human papillomavirus and p16 detection in cervical lymph node metastases from an unknown primary tumor. Oral Oncol 48:1250–1256. https://doi.org/10.1016/j.oraloncology.2012.05.026
Cuaron J, Rao S, Wolden S, Zelefsky M et al (2016) Patterns of failure in patients with head and neck carcinoma of unknown primary treated with radiation therapy. Head Neck 38:E426–E431. https://doi.org/10.1002/hed.24013
Prigge ES, Toth C, Dyckhoff G et al (2015) p16(INK4a) /Ki-67 co-expression specifically identifies transformed cells in the head and neck region. Int J Cancer 136:1589–1599. https://doi.org/10.1002/ijc.29130
Linxweiler M, Bochen F, Wemmert S et al (2015) Combination of p16(INK4a)/Ki67 immunocytology and HPV polymerase chain reaction for the noninvasive analysis of HPV involvement in head and neck cancer. Cancer Cytopathol 123:219–229. https://doi.org/10.1002/cncy.21512
Ciesielska U, Zatonski T, Nowinska K et al (2017) Expression of cell cycle-related proteins p16, p27 and Ki-67 proliferating marker in laryngeal squamous cell carcinomas and in laryngeal papillomas. Anticancer Res 37:2407–2415
Liu J, Zhang M, Rose B et al (2015) Ki67 expression has prognostic significance in relation to human papillomavirus status in oropharyngeal squamous cell carcinoma. Ann Surg Oncol 22:1893–1900. https://doi.org/10.1245/s10434-014-4237-x
Rittà M, De Andrea M, Mondini M et al (2009) Cell cycle and viral and immunologic profiles of head and neck squamous cell carcinoma as predictable variables of tumor progression. Head Neck 31:318–327. https://doi.org/10.1002/hed.20977
Machtay M, Moughan J, Trotti A et al (2008) Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol 26:3582–3589. https://doi.org/10.1200/JCO.2007.14.8841
Givens DJ, Karnell LH, Gupta AK et al (2009) Adverse events associated with concurrent chemoradiation therapy in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 135:1209–1217. https://doi.org/10.1001/archoto.2009.174
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidlines®) Senior adult oncology Version 2.2014. © 2014 National Comprehensive Cancer Network, Inc. NCCN.org. Accessed 1 Nov 2018
Lewis JS Jr, Thorstad WL, Chernock RD et al (2010) p16 positive oropharyngeal squamous cell carcinoma:an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol 34:1088–1096. https://doi.org/10.1097/PAS.0b013e3181e84652
Smeets SJ, Hesselink AT, Speel EJ et al (2007) A novel algorithm for reliable detection of human papillomavirus in paraffin embedded head and neck cancer specimen. Int J Cancer 21:2465–2472
Chernock RD, El-Mofty SK, Thorstad WL et al (2009) HPV-related nonkeratinizing squamous cell carcinoma of the oropharynx: utility of microscopic features in predicting patient outcome. Head Neck Pathol 3:186–194. https://doi.org/10.1007/s12105-009-0126-1
Penault-Llorca F, André F, Sagan C, Lacroix-Triki M et al (2009) Ki67 expression and docetaxel efficacy in patients with estrogen receptor-positive breast cancer. J Clin Oncol 27:2809–2815. https://doi.org/10.1200/JCO.2008.18.2808
Gillison ML, D’Souza G, Westra W et al (2008) Distinct risk factor profiles for human papillomavirus type 16-positive and Human papillomavirus type 16-negative head and neck cancers. J Natl Cancer Inst 100:407–420. https://doi.org/10.1093/jnci/djn025
Fallai C, Perrone F, Licitra L et al (2009) Oropharygeal squamous cell carcinoma treated with radiotherapy or radiochemotherapy: prognostic role of P53 and HPV status. Int J Radiat Oncol Biol Phys 75:1053–1059. https://doi.org/10.1016/j.ijrobp.2008.12.088
Acknowledgements
The authors thank Bierta Barfod for her contribution to the language editing of this manuscript.
Funding
No specific funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical approval retrospective studies
This study was approved by the institutional review board, and patient informed consent was obtained. (Trial registration number: Nihon University Itabashi Hospital Clinical Research Center RK-170214-9).
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article. Documentation of informed consent for treatment was signed by each patient and placed in the patient’s medical record.
Research data policy
The dataset supporting the conclusions of this article is included within the article.
Consent for publication
copy of the written consent is available for review by the Editor-in-Chief of this journal.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maebayashi, T., Ishibashi, N., Aizawa, T. et al. Roles of Ki-67 and p16 as biomarkers for unknown primary head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 276, 1221–1229 (2019). https://doi.org/10.1007/s00405-019-05338-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05338-3