Abstract
Purpose
To evaluate upper esophageal sphincter (UES) activity in patients with benign glottic lesions.
Methods
Twenty-three patients with benign vocal fold (VF) lesions scheduled for manometric evaluation were enrolled as the study group (SG); 20 healthy subjects without vocal pathology or dysphagia were included as the control group (CG). UES residual, basal, relaxation time and peak pharyngeal pressures were evaluated by manometry. The reflux symptom index (RSI) and reflux finding score (RFS) were used to estimate the clinical findings of laryngopharyngeal reflux, and the voice handicap index (VHI) was measured in both groups. The patients’ data were compared using the Mann–Whitney test and t test.
Results
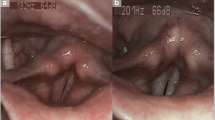
The diagnoses in the SG were vocal nodules, vocal polyps, vocal cysts, sulcus vocalis, or Reinke’s edema. The evaluation scores (RSI, RFS, and VHI) were significantly higher in the SG than in the CG (P < 0.05). UES basal and relaxation pressures, relaxation time, and peak pharyngeal pressures did not differ between the SG and the CG (P > 0.05).
Conclusion
UES manometric pressure was similar in patients with VF mucosal lesions and controls. Studies involving larger populations are necessary to confirm the manometric changes in the UES and to elucidate the pathogenesis of benign VF lesions.


Similar content being viewed by others
References
Wong RKH, Hanson DG, Warring PJ, Shaw G (2000) ENT manifestations of gastroesophageal reflux. Am J Gastroenterol 95:S15–S22
Axford SE, Sharp N, Ross PE, Pearson JP, Dettmar PW, Panetti M et al (2001) Cell biology of laryngeal epithelial defenses in health and disease: preliminary studies. Ann Otol Rhinol Laryngol 110:1099–1108
Mearin F, Ponce J, Ponce M et al (2012) Frequency and clinical implications of supraesophageal and dyspeptic symptoms in gastroesophageal reflux disease. Eur J Gastroenterol Hepatol 24:665–674
Shaker R, Babaei A, Naini SR (2014) Prevention of esophagopharyngeal reflux by augmenting the upper esophageal sphincter pressure barrier. Laryngoscope 124:2268–2274
Beaver ME, Karow CM (2012) Clinical utility of 24 hour pharyngeal pH monitoring for hoarseness. J Laryngol Voice 2:60–63
Koufman JA (1991) The otolaryngologic manifestations of gastroesophageal reflux disease: a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101(Suppl 53):1–78
Babaei A, Venu M, Naini SR, Gonzaga J, Lang IM, Massey BT, Jadcherla S, Shaker R (2015) Impaired upper esophageal sphincter reflexes in patients with supraesophageal reflux disease. Gastroenterology 149:1381–1391
Vardar R, Sweis R, Anggiansah A, Wong T, Fox MR (2013) Upper esophageal sphincter and esophageal motility in patients with chronic cough and reflux: assessment by high-resolution manometry. Dis Esophagus 26:219–225
Chung JH, Tae K, Lee YS, Jeong JH, Cho SH, Kim KR, Park CW, Han DS (2009) The significance of laryngopharyngeal reflux in benign vocal mucosal lesions. Otolaryngol Head Neck Surg 141:369–373
Powell J, Cocks HC (2013) Mucosal changes in laryngopharyngeal reflux-prevalence, sensitivity, specificity and assessment. Laryngoscope 123:985–991
Belafsky PC, Postma GN, Koufman JA (2001) Validity and reliability of the reflux finding Score (RFS). Laryngoscope 111:1313–1317
Belafsky PC, Postma GN, Koufman JA (2001) Validity and reliability of the reflux symptom index (RSI). Laryngoscope 111:1313–1317
Koufman JA, Amin MR, Panetti M (2000) Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg 123:385–388
Adhami T, Goldblum JR, Richter JE, Vaezi MF (2004) The role of gastric and duodenal agents in laryngeal injury: an experimental canine model. Am J Gastroenterol 99:2098–2106
Karkos PD, Wilson JA (2006) Empiric treatment of laryngopharyngeal reflux with proton pump inhibitors: a systematic review. Laryngoscope 116:144–148
Francis DO, Patel DA, Sharda R et al (2016) Patient-reported outcome measures related to laryngopharyngeal reflux: a systematic review of instrument development and validation. Otolaryngol Head Neck Surg 155:923–935
Benjamin T, Zackria S, Lopez R, Richter J, Thota PN (2017) Upper esophageal sphincter abnormalities and high resolution esophageal manometry findings in patients with laryngopharyngeal reflux. Scand J Gastroenterol 52:816–821
Passaretti S, Mazzoleni G, Vailati C, Testoni PA (2016) Oropharyngeal acid reflux and motility abnormalities of the proximal esophagus. World J Gastroenterol 22:8991–8998
Szczesniak MM, Williams RB, Brake HM, Maclean JC, Cole IE, Cook IJ (2010) Upregulation of the esophago-UES relaxation response: a possible pathophysiological mechanism in suspected reflux laryngitis. Neurogastroenterol Motil 22:381–386
Kahrilas PJ, Dodds WJ, Dent J, Haeberle B, Hogan WJ, Arndorfer RC (1987) Effect of sleep, spontaneous gastroesophageal reflux, and a meal on upper esophageal sphincter pressure in normal human volunteers. Gastroenterology 92:466–471
Vakil NB, Kahrilas PJ, Dodds WJ, Vanagunas A (1989) Absence of an upper esophageal sphincter response to acid reflux. Am J Gastroenterol 84:606–610
Kahrilas PJ, Jonsson A, Denison H, Wernersson B, Hughes N, Howden CW (2012) Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol 10:612–619
Babaei A, Massey B, Hogan W, Rahimi S, DeMara M, Shaker R (2013) Regurgitation can indicate either true esophago-pharyngeal reflux (EPR) event or upper esophageal sphincter (UES) and sub-sphincter proximal esophageal acid exposure. Gastroenterology 144:S839
Funding
No financial disclosure for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Kibar, E., Erdur, O. & Ozturk, K. Evaluation of upper esophageal sphincter in benign vocal lesions. Eur Arch Otorhinolaryngol 275, 3033–3037 (2018). https://doi.org/10.1007/s00405-018-5175-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5175-1