Abstract
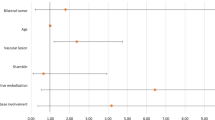
The objective of this study was to analyze the possible correlation between Shamblin’s classification and post-surgical morbidity in the treatment of carotid body tumors (CBTs). Seventy-two patients with carotid body tumors were seen over a 22-year period. Twenty-three patients were excluded as they did not comply with the criteria of the objectives. All patients were grouped according to Shamblin’s classification. We propose a modification to this classification and make a comparison by analyzing the surgical time and bleeding, as well as the neurological and vascular damage. We resected 50 CBTs in 49 patients, ranging in age from 18 to 73 years. Three groups were formed: group I with 8 (16%) patients, group II with 17 (34%) and group III with 24 (49%). Post-surgical neurological damage was observed in one patient (12.5%) from group I, in six (35%) from group II and in nine patients (37.5%) from group III. Vascular sacrifice had to be performed in 21% of class II tumors and in 8.7% of class III. None of the class I tumors required vascular sacrifice. No statistically significant difference existed for vascular or neurological risk in relation to Shamblin’s classification. However, when analyzed according to the classification proposed herein, there was a correlation between Shamblin’s classification and vascular sacrifice ( P =0.001). There was a statistically significant correlation between the original Shamblin and the modified Shamblin regarding surgical time and bleeding. Shamblin’s classification predicts only vascular morbidity. Neurological morbidity is not reflected in it and only reflects the surgeon’s experience with CBT resections. Surgical time and bleeding are directly related to the Shamblin as it reflects the size of tumors in relation to the blood vessels. Shamblin’s classification must be modified to be more objective so that the international reports can accurately reflect the morbidity related to it.


Similar content being viewed by others
References
Carrau R, Myers E, Johnson J (1990) Management of tumors arising in the parapharyngeal space. Laryngoscope 100:583–589
Davidge-Pitts KJ, Pantanowitz D (1984) Carotid body tumor. Surg Ann 16:203–207
Gordon-Taylor G (1982) On carotid body tumors. BMJ 284:1507–1508
Granados-Garcia M, Rascon-Ortiz M, Herrera-Gomez A, Luna-Ortiz K (2004) Reconstrucción de arteria carótida interna con trasposición de arteria carótida externa en resección de tumores del cuerpo carotídeo. Cir Cir 72:457–459
Lees CD, Levine H, Beven E, Tucker H (1981) Tumors of the carotid body. Am J Surg 142:362–365
Leonetti J, Donzelli J, Littooy F, Farrel B (1997) Perioperative strategies in the management of carotid body tumors. Otolaryngol Head Neck Surg 117:111–115
Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Granados-Garcia M, Herrera-Gomez A (2005) Carotid body tumors: review of a 20-year experience. Oral Oncol 41:56–61
Patetsios P, Gable D, Garret W, Lamont J, Kuhn J, Shutze W, Kourlis H, Grimsley B, Pearl Gj, Smith BL, Talkington CM, Thompson JE (2002) Management of carotid body paragangliomas and review of a 30-year experience. Ann Vasc Surg 16:331–338
Plukker JTM, Brongers EP, Vermey A, Krikke A, van den Dungen JJAM (2001) Outcome of surgical treatment for carotid body paraganglioma. Br J Surg 88:1382–1386
Rosen I, Palmer J, Goldberg M, Mustard R (1981) Vascular problems associated with carotid body tumors. Am J Surg 142:459–463
Shamblin WR, Remine WH, Sheps SG, Harrison EG (1971) Carotid body tumor (chemodectoma). Clinicophatologic analysis of 90 cases. Am J Surg 122:732–739
Westerband A, Hunter GC, Cintora I, Coulthard SW, Hinni ML, Gentile AT, Devine J, Mills JL (1998) Current trends in the detection and management of carotid body tumors. J Vasc Surg 28:84–93
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00405-006-0121-z.
Rights and permissions
About this article
Cite this article
Luna-Ortiz, K., Rascon-Ortiz, M., Villavicencio-Valencia, V. et al. Does Shamblin’s classification predict postoperative morbidity in carotid body tumors? A proposal to modify Shamblin’s classification. Eur Arch Otorhinolaryngol 263, 171–175 (2006). https://doi.org/10.1007/s00405-005-0968-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-005-0968-4