Abstract
Purpose
The trend of delaying childbirth has resulted in a growing number of advanced-aged women who are opting for preimplantation genetic testing (PGT) to screen for monogenic diseases or structural chromosomal rearrangements (PGT-M and PGT-SR). This increase in demand necessitates the development of a clinical predictive model for live birth outcomes in these women. Therefore, the objective of this study is to construct a comprehensive predictive model that assesses the likelihood of achieving a successful live birth in advanced-aged women undergoing PGT-M and PGT-SR treatments.
Methods
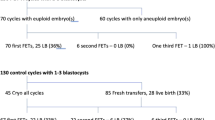
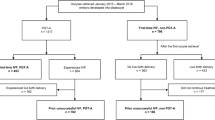
A retrospective cohort study of 37–45-year-old women undergoing preimplantation genetic testing for monogenic disease or structural chromosomal rearrangement cycles from 2010 to 2021 was conducted at a university hospital reproductive centre. The purpose was to develop a clinical predictive model for live birth in these women. The main outcome studied was the cumulative live birth rate in the first or subsequent cycles. Developing a decision tree enabled a comprehensive study of clinical parameters and expected outcomes.
Results
The analysis included 158 women undergoing 753 preimplantation genetic testing cycles. The cumulative live birth rate was 37.342% (59/158). Decision tree analysis revealed that women aged ≤ 40.1 or women > 40.1 with one or more top-quality transferable embryos in their first cycle had the best chance for a live baby (56% and 41%, respectively). Those older than 40.1 without top-quality embryos and seven or fewer dominant follicles had no live births. A Kaplan–Meier curve showed that for autosomal dominant diseases, there was a negligible increase in live birth rate after three cycles, compared to six cycles in autosomal recessive inheritance.
Conclusion
In older women, the chance of delivering after repeated cycles is higher in those with at least one top-quality unaffected embryo in their first preimplantation genetic testing cycle. Additional preimplantation genetic testing cycles after three in carriers of an autosomal dominant disorder and six in those with an autosomal recessive disorder should be considered prudently.


Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Sullivan-Pyke C, Dokras A (2018) Preimplantation genetic screening and preimplantation genetic diagnosis. Obstet Gynecol Clin 45:113–125
Butler R, Nakhuda G, Guimond C, Jing C, Lee N, Hitkari J, Tallon N, Taylor B, Yuzpe A (2019) Analysis of PGT-M and PGT-SR outcomes at a Canadian fertility clinic. Prenat Diagn 39:866–870
Verpoest W, Haentjens P, De Rycke M, Staessen C, Sermon K, Bonduelle M, Devroey P, Liebaers I (2009) Cumulative reproductive outcome after preimplantation genetic diagnosis: a report on 1498 couples. Hum Reprod 24:2951–2959
Zanetti BF, Braga DPAF, Azevedo MC, Setti AS, Figueira RCS, Iaconelli A, Borges E (2019) Preimplantation genetic testing for monogenic diseases: a Brazilian IVF centre experience. JBRA Assist Reprod 23:99–105
Coonen E, van Montfoort A, Carvalho F, Kokkali G, Moutou C, Rubio C, De Rycke M, Goossens V (2020) ESHRE PGT Consortium data collection XVI-XVIII: cycles from 2013 to 2015. Hum Reprod Open 2020:hoaa043
Van Der Kelen A, Santos-Ribeiro S, De Vos A, Verdyck P, De Rycke M, Berckmoes V, Tournaye H, Blockeel C, De Vos M, Hes FJ et al (2021) Parameters of poor prognosis in preimplantation genetic testing for monogenic disorders. Hum Reprod 36:2558–2566
Ben-Nagi J, Jones B, Naja R, Amer A, Sunkara S, SenGupta S, Serhal P (2019) Live birth rate is associated with oocyte yield and number of biopsied and suitable blastocysts to transfer in preimplantation genetic testing (PGT) cycles for monogenic disorders and chromosomal structural rearrangements. Eur J Obstet Gynecol Reprod Biol X 4:100055
Tur-Kaspa I, Bernal A, Tkachenko N, Pawlovska J, Rechitsky S, Verlinsky Y (2007) To PGD or not to PGD: is there a magic number of oocytes to start with? Fertil Steril 88:S231–S232
Tur-Kaspa I (2012) Clinical management of in vitro fertilization with preimplantation genetic diagnosis. Semin Reprod Med 30:309–322
Hamilton BE, Martin JA, Osterman MJ, Driscoll AK, Rossen LM (2018) Births: provisional data for 2017 (Vital Statistics Rapid Release Report 004). Hyattsville, MD: National Center for Health Statistics
Martin JA, Hamilton BE, Osterman MJK (2017) Births in the United States. NCHS Data Brief 2018:1–8
Birenbaum-Carmeli D (2016) Thirty-five years of assisted reproductive technologies in Israel. Reprod Biomed Soc Online 2:16–23
Bercovich O, Almog B, Fouks Y, Kalma Y, Hasson J, Azem F, Cohen Y (2021) A decision tree analysis applied to women aged 43–45: who should be referred for ovum donation? Reprod BioMed Online 44:112–118
Malcov M, Gold V, Peleg S, Frumkin T, Azem F, Amit A, Ben-Yosef D, Yaron Y, Reches A, Barda S et al (2017) Improving preimplantation genetic diagnosis (PGD) reliability by selection of sperm donor with the most informative haplotype. Reprod Biol Endocrinol 15:31
Sermon K, De Rycke M (2007) Single cell polymerase chain reaction for preimplantation genetic diagnosis: methods, strategies, and limitations. Methods Mol Med 132:31–42
Frumkin T, Peleg S, Gold V, Reches A, Asaf S, Azem F, Ben-Yosef D, Malcov M (2017) Complex chromosomal rearrangement-a lesson learned from PGS. J Assist Reprod Genet 34:1095–1100
Committee ACoOaGCoGPaP (2014) Female age-related fertility decline. Committee Opinion No. 589. Fertil Steril 101:633–634
Sullivan AK, Marcus M, Epstein MP, Allen EG, Anido AE, Paquin JJ, Yadav-Shah M, Sherman SL (2005) Association of FMR1 repeat size with ovarian dysfunction. Hum Reprod 20:402–412
Acknowledgements
None.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
OB: data collection, data analysis, data interpretation and writing of the manuscript. GK: data collection, data interpretation. TS: manuscript revision. BA: study design, manuscript revision and final approval. YK: data collection, manuscript revision and final approval. RR: manuscript revision. FA: manuscript revision and final approval. MM: data collection, study design and manuscript revision. YC: study design, writing of the manuscript, manuscript revision and final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The protocol of this retrospective study was approved by the institutional review board of the Tel Aviv Soraski Medical Centre’s ethics committee (0149-20-TLV).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bercovich, O., Klar, G., Shaulov, T. et al. A clinical predictive model for live birth in women of advanced age undergoing PGT cycles. Arch Gynecol Obstet 309, 1083–1090 (2024). https://doi.org/10.1007/s00404-023-07329-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-023-07329-6