Abstract
Objective
This study aimed to investigate the effectiveness and safety of a method combining double-balloon catheter for cervical ripening and intravenous drip of oxytocin on the induction of term labor, providing the reference for clinical safety.
Methods
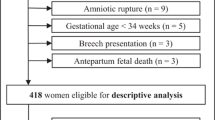
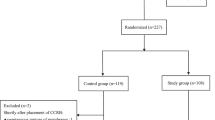
A total of 120 pregnant women with a gestation between 37+0 and 41+6 weeks, indications of labor induction, singleton pregnancy with cephalic presentation were enrolled. The patients were divided into the research group receiving cervical dilation balloon combined with intravenous drip of oxytocin and the control group receiving an intravenous drip of oxytocin at a concentration of 0.5% for labor induction (n = 60 for each). The effectiveness and safety of labor induction were evaluated by the rates of successful cervical ripening promotion and labor induction, as well as the vaginal delivery rate, induced labor time, total duration of labor, the total amount of postpartum hemorrhage within 24 h after giving birth, the incidences of postpartum hemorrhage, cervical laceration, puerperal infection and neonatal outcomes.
Results
There was no statistical difference in the basal demographic and clinical characteristics, including ages, gestational weeks, delivery times and Bishop scores at admission between two groups. The rate of successful cervical ripening promotion (research vs. control = 90.00% vs. 55.00%), the rate of successful induction (95.00% vs. 40.00%), the vaginal delivery rate (93.33% vs. 63.33%), the induced labor time (15.03 ± 5.40 vs. 30.68 ± 10.82 h), and the total duration of labor (8.12 ± 2.65 vs. 15.01 ± 6.06 h) were significantly different between two groups (all P < 0.05). There was no significant difference in the total amount of postpartum hemorrhage, incidences of postpartum hemorrhage, cervical laceration, puerperal infection as well as the neonatal outcomes, including neonatal weight, neonatal asphyxia and incidence of meconium aspiration syndrome between two groups.
Conclusions
Compared to labor induction of oxytocin, the method combining double-balloon catheter for cervical ripening and intravenous drip of oxytocin for the induction of term labor has a higher vaginal delivery rate, shorter total duration of labor, and does not increase the incidences of postpartum hemorrhage and neonatal infection, which is a more effective and safer method for induction of term labor.
Similar content being viewed by others
References
Bacak SJ, Olsonchen C, Pressman E (2015) Timing of induction of labor. Semin Perinatol 39:450–458
Alimena S, Nold C, Herson V, Fang YM (2016) Rates of intrauterine fetal demise and neonatal morbidity at term: determining optimal timing of delivery. J Matern Fetal Neonatal Med 30:181–185
Torricelli M, Voltolini C, Conti N, Bocchi C, Severi FM, Petraglia F (2013) Weight gain regardless of pre-pregnancy BMI and influence of fetal gender in response to labor induction in postdate pregnancy. J Matern Fetal Neonatal Med 26:1016–1019
Rezaie KK, Keikha F, Rezaie KK, Abdollahimohammad A, Salehin S (2014) Perinatal outcome after diagnosis of oligohydramnious at term. Iran Red Crescent Med J 16:e11772
Moore TR (2011) The role of amniotic fluid assessment in indicated preterm delivery. Semin Perinatol 35:286–291
Shibata T, Nakago S, Kato H, Tokuda H, Matsuki R, Kotsuji F (2016) Management of severe pregnancy-induced hypertension after 34 weeks of gestation: a prospective study to reduce the rate of cesarean section. Hypertens Pregnancy 35:82–90
Garcia-Simon R, Montañes A, Clemente J, Del Pino MD, Romero MA, Fabre E, Oros D (2015) Economic implications of labor induction. Int J Gynaecol Obstet 133:112–115
Feghali MN, Caritis SN, Catov JM, Scifres CM (2016) Timing of delivery and pregnancy outcomes in women with gestational diabetes. Am J Obstet Gynecol 215:241–243
Kalra B, Gupta Y, Kalra S (2016) Timing of delivery in gestational diabetes mellitus: need for person-centered, shared decision-making. Diabetes Therapy 7:1–6
Committee EI, Committee MFM, Liu K, Case A (2011) Advanced reproductive age and fertility. Int J Gynecol Obstet 33:1165
Behboudigandevani S, Ziaei S, Farahani FK, Jasper M (2015) The perspectives of iranian women on delayed childbearing: a qualitative study. J Nurs Res 23:313–321
Balasch J, Gratacós E (2012) Delayed childbearing: effects on fertility and the outcome of pregnancy. Curr Opin Obstet Gynecol 24:187
Olusanya BO, Solanke OA (2012) Perinatal correlates of delayed childbearing in a developing country. Arch Gynecol Obstet 285:951–957
Joseph KS, Allen AC, Dodds L, Turner LA, Scott H, Liston R (2005) The perinatal effects of delayed childbearing. Obstet Gynecol 105:1410–1418
Rath W (2005) A clinical evaluation of controlled-release dinoprostone for cervical ripening—a review of current evidence in hospital and outpatient settings. J Perinat Med 33:491–499
Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM (2011) Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol 117:805
Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL (2011) Methods of induction of labour: a systematic review. BMC Pregnancy Childbirth 11:84
Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Medley N, Dias S, Jones LV, Gyte G, Caldwell DM (2016) Which method is best for the induction of labour? A systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol Assess 20:1–584
Kehl S, Böhm L, Weiss C, Heimrich J, Dammer U, Baier F, Sütterlin M, Beckmann MW, Faschingbauer F (2016) Timing of sequential use of double-balloon catheter and oral misoprostol for induction of labor. J Obstet Gynaecol Res 42:1495–1501
Kansu-Celik H, Gun-Eryılmaz O, Dogan NU, Haktankaçmaz S, Cinar M, Yilmaz SS, Gülerman C (2017) Prostaglandin E2 induction of labor and cervical ripening for term isolated oligohydramnios in pregnant women with Bishop score ≤5. J Chin Med Assoc 80:169–172
Kacvinska A, Drab M, Totka A, Holoman K, Gabor M (2016) The effect of prostaglandin induced labor and selected factors on the occurrence and extent of birth-canal injuries. Bratisl Lek Listy 117:511–514
Tolcher MC, Holbert MR, Weaver AL, Mcgree ME, Olson JE, El-Nashar SA, Famuyide AO, Brost BC (2015) Predicting cesarean delivery after induction of labor among nulliparous women at term. Obstet Gynecol 126:1059–1068
Jozwiak M, Mol BW, Bloemenkamp KW (2010) Induction of labour in nulliparous women with an unfavourable cervix. BJOG 117:892
Iliodromiti Z, Antonakopoulos N, Sifakis S, Tsikouras P, Daniilidis A, Dafopoulos K, Botsis D, Vrachnis N (2012) Endocrine, paracrine, and autocrine placental mediators in labor. Hormones 11:397–409
Zhao Y, Koga K, Osuga Y, Izumi G, Takamura M, Harada M, Hirata T, Hirota Y, Yoshino O, Fujii T (2013) Cyclic stretch augments production of neutrophil chemokines and matrix metalloproteinase-1 in human uterine smooth muscle cells. Am J Reprod Immunol 69:240–247
Gonzalez JM, Dong Z, Romero R, Girardi G (2011) Cervical remodeling/ripening at term and preterm delivery: the same mechanism initiated by different mediators and different effector cells. PLoS ONE 6:e26877
Ivars J, Garabedian C, Devos P, Therby D, Carlier S, Deruelle P, Subtil D (2016) Simplified Bishop score including parity predicts successful induction of labor. Eur J Obstet Gynecol Reprod Biol 203:309–314
Springhall E, Wallace EM, Stewart L, Knight M, Mockler JC, Davies-Tuck M (2017) Customised management of the third stage of labour. Aust N Z J Obstet Gynaecol 57:302–307
Malmnäs C (1969) Induction of labour in the second and third trimester of pregnancy by a cervical balloon and intrauterine oxytocin infusion. Acta Obstet Gynecol Scand 48(Suppl 3):18+
Dueñas-Garcia OF, Young CA, Mikhail M (2010) Uterine rupture secondary to the use a cook balloon as tamponade. J Minim Invas Gyn 17:S187
Ducarme G, Grange J, Vital M (2016) Expansion dilatation balloons for cervical ripening in obstetric practice. J Gynecol Obstet Biol Reprod (Paris) 45:112–119
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported by the grants from the Nature Science Foundation of China (81470015 and 81670256), the Science and Technology Project of Special Funds of Guangzhou (2014J4100168), Guangdong Science and Technology Project (2016A020216005, 2015B090903063 and 2015A020212006), the Natural Science Foundation of Guangdong Province (2014A030313079) and Guangzhou Science and Technology Project (201510010052).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of Longgang District Center Hospital of Shenzhen.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wu, X., Wang, C., Li, Y. et al. Cervical dilation balloon combined with intravenous drip of oxytocin for induction of term labor: a multicenter clinical trial. Arch Gynecol Obstet 297, 77–83 (2018). https://doi.org/10.1007/s00404-017-4564-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4564-9