Abstract
Background
As the incidence of colorectal cancer tends to be younger, early-onset colorectal cancer (EOCRC) has attracted more attention in recent years. We aimed to assess the optimal lymph node staging system among EOCRC patients, and then, establish informative assessment models for prognosis prediction.
Methods
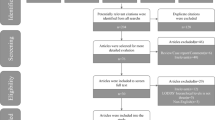
Data of EOCRC were retrieved from the Surveillance, Epidemiology, and End Results database. Survival prediction ability of three lymph node staging systems including N stage of the tumor node metastasis (TNM) staging system, lymph node ratio (LNR), and log odds of positive lymph nodes (LODDS) was assessed and compared using Akaike information criterion (AIC), Harrell’s concordance index (C-index), and likelihood ratio (LR) test. Univariate and multivariate Cox regression analyses were conducted to identify the prognostic predictors for overall survival (OS) and cancer-specific survival (CSS). Effectiveness of the model was demonstrated by receiver operative curve and decision curve analysis.
Results
A total of 17,535 cases were finally included in this study. All three lymph node staging systems showed significant performance in survival prediction (p < 0.001). Comparatively, LODDS presented a better ability of prognosis prediction with lower AIC (OS: 70,510.99; CSS: 60,925.34), higher C-index (OS: 0.6617; CSS: 0.6799), and higher LR test score (OS: 998.65; CSS: 1103.09). Based on independent factors identified from Cox regression analysis, OS and CSS nomograms for EOCRC were established and validated.
Conclusions
LODDS shows better predictive performance than N stage or LNR among patients with EOCRC. Novel validated nomograms based on LODDS could effectively provide more prognostic information than the TNM staging system.





Similar content being viewed by others
Data availability
The data generated and analyzed during the current study are available in the SEER database, which could be obtained via the SEER*Stat software (http://seer.cancer.gov/seerstat/) from the latest version of the SEER database of the National Cancer Institute (NCI).
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Burnett-Hartman AN, Lee JK, Demb J, Gupta S (2021) An update on the epidemiology, molecular characterization, diagnosis, and screening strategies for early-onset colorectal cancer. Gastroenterology 160(4):1041–1049
Kolarich A, George TJ Jr, Hughes SJ, Delitto D, Allegra CJ, Hall WA et al (2018) Rectal cancer patients younger than 50 years lack a survival benefit from NCCN guideline-directed treatment for stage II and III disease. Cancer 124(17):3510–3519
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ et al (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21(15):2912–2919
Baqar AR, Wilkins S, Wang W, Oliva K, McMurrick P (2020) Log odds of positive lymph nodes is prognostically equivalent to lymph node ratio in non-metastatic colon cancer. BMC Cancer 20(1):762
Shen F, Cui J, Cai K, Pan H, Bu H, Yu F (2018) Prognostic accuracy of different lymph node staging systems in rectal adenocarcinoma with or without preoperative radiation therapy. Jpn J Clin Oncol 48(7):625–632
Zhang CH, Li YY, Zhang QW, Biondi A, Fico V, Persiani R et al (2018) The prognostic impact of the metastatic lymph nodes ratio in colorectal cancer. Front Oncol 8:628
Arrichiello G, Pirozzi M, Facchini BA, Facchini S, Paragliola F, Nacca V et al (2022) Beyond N staging in colorectal cancer: current approaches and future perspectives. Front Oncol 12:937114
Spolverato G, Ejaz A, Kim Y, Squires MH, Poultsides G, Fields RC et al (2015) Prognostic performance of different lymph node staging systems after curative intent resection for gastric adenocarcinoma. Ann Surg 262(6):991–998
Wang MS, Wang MZ, Wang Z, Song Y, Gao P, Wang P et al (2021) Comparison of three lymph node staging methods for predicting outcome in breast cancer patients with mastectomy. Ann Transl Med 9(4):300
Jiang S, Zhang J, Zhang L, Xu Y, Zhao H, Sang X et al (2022) A novel nomogram based on log odds of positive lymph nodes to predict survival for non-metastatic gallbladder adenocarcinoma after surgery. Sci Rep 12(1):16466
Weiser MR (2018) AJCC 8th Edition: Colorectal Cancer. Ann Surg Oncol 25(6):1454–1455
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK et al (2021) Colon Cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 19(3):329–59
Benson AB, Venook AP, Al-Hawary MM, Azad N, Chen YJ, Ciombor KK et al (2022) Rectal Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 20(10):1139–67
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res 10(21):7252–7259
Kneuertz PJ, Chang GJ, Hu CY, Rodriguez-Bigas MA, Eng C, Vilar E et al (2015) Overtreatment of young adults with colon cancer: more intense treatments with unmatched survival gains. JAMA Surg 150(5):402–409
Ferrari A, Rognone A, Casanova M, Zaffignani E, Piva L, Collini P et al (2008) Colorectal carcinoma in children and adolescents: the experience of the Istituto Nazionale Tumori of Milan. Italy Pediatr Blood Cancer 50(3):588–593
Khan SA, Morris M, Idrees K, Gimbel MI, Rosenberg S, Zeng Z et al (2016) Colorectal cancer in the very young: a comparative study of tumor markers, pathology and survival in early onset and adult onset patients. J Pediatr Surg 51(11):1812–1817
Chang DT, Pai RK, Rybicki LA, Dimaio MA, Limaye M, Jayachandran P et al (2012) Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol 25(8):1128–1139
Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, Gallino G et al (2010) Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer 116(3):758–765
Wang MJ, Ping J, Li Y, Adell G, Arbman G, Nodin B et al (2015) The prognostic factors and multiple biomarkers in young patients with colorectal cancer. Sci Rep 5:10645
Huang B, Mo S, Zhu L, Xu T, Cai G (2016) The survival and clinicopathological differences between patients with stage IIIA and stage II rectal cancer: an analysis of 12,036 patients in the SEER database. Oncotarget 7(48):79787–79796
Cai H, Xu T, Zhuang Z, Zhang Y, Gao Y, Liu X et al (2021) Value of the log odds of positive lymph nodes for prognostic assessment of colon mucinous adenocarcinoma: analysis and external validation. Cancer Med 10(23):8542–8557
Huang Y, Ji L, Zhu J, Mao X, Sheng S, Hao S et al (2021) Lymph node status and its impact on the prognosis of left-sided and right-sided colon cancer: A SEER population-based study. Cancer Med 10(23):8708–8719
Lee CW, Wilkinson KH, Sheka AC, Leverson GE, Kennedy GD (2016) The log odds of positive lymph nodes stratifies and predicts survival of high-risk individuals among stage III rectal cancer patients. Oncologist 21(4):425–432
Petrucciani N, Carra MC, Martinez-Perez A, Vitali GC, Landi F, Genova P et al (2019) Comparison of different nodal staging in patients with locally advanced mid-low rectal cancer after long-term neoadjuvant chemoradiation therapy. Anticancer Res 39(4):2113–2120
Yang Y, Zheng J, Li Y (2022) Comparison of 4 lymph node staging systems for the prognostic prediction of esophagogastric junction adenocarcinoma with </=15 retrieved lymph nodes. Eur J Surg Oncol 48(5):1017–1024
Ogawa S, Itabashi M, Bamba Y, Yamamoto M, Sugihara K (2020) Superior prognosis stratification for stage III colon cancer using log odds of positive lymph nodes (LODDS) compared to TNM stage classification: the Japanese study group for postoperative follow-up of colorectal cancer. Oncotarget 11(33):3144–3152
Zhang QW, Zhang CH, Pan YB, Biondi A, Fico V, Persiani R et al (2020) Prognosis of colorectal cancer patients is associated with the novel log odds of positive lymph nodes scheme: derivation and external validation. J Cancer 11(7):1702–1711
Fortea-Sanchis C, Martinez-Ramos D, Escrig-Sos J (2018) The lymph node status as a prognostic factor in colon cancer: comparative population study of classifications using the logarithm of the ratio between metastatic and nonmetastatic nodes (LODDS) versus the pN-TNM classification and ganglion ratio systems. BMC Cancer 18(1):1208
Lu YJ, Lin PC, Lin CC, Wang HS, Yang SH, Jiang JK et al (2013) The impact of the lymph node ratio is greater than traditional lymph node status in stage III colorectal cancer patients. World J Surg 37(8):1927–1933
Zhu J, Hao J, Ma Q, Shi T, Wang S, Yan J et al (2021) A novel prognostic model and practical nomogram for predicting the outcomes of colorectal cancer: based on tumor biomarkers and log odds of positive lymph node scheme. Front Oncol 11:661040
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16(4):e173–e180
Iasonos A, Schrag D, Raj GV, Panageas KS (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26(8):1364–1370
Himbert C, Figueiredo JC, Shibata D, Ose J, Lin T, Huang LC et al (2021) Clinical characteristics and outcomes of colorectal cancer in the ColoCare Study: differences by age of onset. Cancers (Basel) 13(15)
Wu J, Lu L, Chen H, Lin Y, Zhang H, Chen E et al (2021) Prognostic nomogram to predict the overall survival of patients with early-onset colorectal cancer: a population-based analysis. Int J Colorectal Dis 36(9):1981–1993
Ge Y, Xiang R, Ren J, Song W, Lu W, Fu T (2021) A nomogram for predicting multiple metastases in metastatic colorectal cancer patients: a large population-based study. Front Oncol 11:633995
Hubbard J, Thomas DM, Yothers G, Green E, Blanke C, O’Connell MJ et al (2012) Benefits and adverse events in younger versus older patients receiving adjuvant chemotherapy for colon cancer: findings from the Adjuvant Colon Cancer Endpoints data set. J Clin Oncol 30(19):2334–2339
McMillan DC, McArdle CS (2009) The impact of young age on cancer-specific and non-cancer-related survival after surgery for colorectal cancer: 10-year follow-up. Br J Cancer 101(4):557–560
O’Connell JB, Maggard MA, Liu JH, Etzioni DA, Livingston EH, Ko CY (2004) Do young colon cancer patients have worse outcomes? World J Surg 28(6):558–562
Mauri G, Sartore-Bianchi A, Russo AG, Marsoni S, Bardelli A, Siena S (2019) Early-onset colorectal cancer in young individuals. Mol Oncol 13(2):109–131
Perea J, Arriba M, Rodriguez Y, Rueda D, Garcia JL, Perez J et al (2017) Frequency and impact of KRAS mutation in early onset colorectal cancer. Hum Pathol 61:221–222
Watson R, Liu TC, Ruzinova MB (2016) High frequency of KRAS mutation in early onset colorectal adenocarcinoma: implications for pathogenesis. Hum Pathol 56:163–170
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Deyu Xiang, Jiahao Feng, and Haina Lyu. Data analyses were performed by Zongyu Liang, Zhu Li, and Guangzhi Mai. Figures and tables were prepared by Qingshui Yang and Wanchuan Wang. The first draft of the manuscript was written by Zongyu Liang and Xiaobin Zhang. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Permission was obtained to retrieve SEER data files with the reference number 19019-Nov2021. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. No ethics approval was declared because the SEER is a publicly available database.
Consent to participate
As patient data were recorded in the SEER database without involving any individual identification, the present study was dispensed with signing informed consent forms.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zongyu Liang, Deyu Xiang, Jiahao Feng, and Haina Lyu are co-first authors and contributed equally to the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, Z., Xiang, D., Feng, J. et al. Log odds of positive lymph nodes show better predictive performance on the prognosis of early-onset colorectal cancer. Int J Colorectal Dis 38, 192 (2023). https://doi.org/10.1007/s00384-023-04490-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04490-x