Abstract
Background
Septic complications after colorectal surgery are frequent and sometimes life threatening. It is well known that inflammation impairs the healing process. It has been suggested that preoperative ongoing inflammation could increase the risk of postoperative infections. This study aimed to elucidate the role of preoperative inflammation on postoperative infectious complications and to understand if, through biological markers, it is possible to identify preoperatively patients at higher risk of infection.
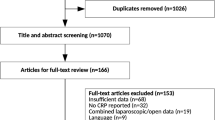
Methods
A prospective, observational study was conducted in three centers from November 2011 to April 2014. Consecutive patients undergoing elective colorectal surgery with anastomosis were included. Any ongoing infection was an exclusion criterion. C-reactive protein, albumin, prealbumin, and procalcitonin plasma levels were measured preoperatively. Postoperative infections were recorded according to the definitions of the Centers for Diseases Control. The areas under the receiver operating characteristic curve were analyzed and compared to assess the accuracy of each preoperative marker.
Results
Four-hundred and seventy two patients were analyzed. Infectious complications occurred in 118 patients (25 %) and mortality in 6 patients (1.3 %). In the univariate analysis, preoperative C-reactive protein and albuminemia were found significantly associated with postoperative infectious complications (P = 0.008 and P = 0.0002, respectively). Areas under the ROC curve for preoperative C-reactive protein and albuminemia were 0.57and 0.62, respectively.
Conclusions
This study confirms the association between preoperative inflammatory activity, hypoalbuminemia, and the onset of infections after surgery. Trials aiming to decrease the inflammatory activity before surgery in order to prevent postoperative complications are warranted.
Similar content being viewed by others
References
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K (2005) Postoperative mortality and morbidity in French patients undergoing colorectal surgery. Arch Surg 140:278–283
Facy O, Paquette B, Orry D, Binquet C, Masson D, Bouvier A, et al. (2016) Diagnostic accuracy of inflammatory markers as early predictors of infection after elective colorectal surgery: results from the IMACORS study. Ann Surg 263:961–966
De Magistris L, Azagra JS, Goergen M, De Blasi V, Arru L, Facy O (2013) Laparoscopic sigmoidectomy in moderate and severe diverticulitis: analysis of short-term outcomes in a continuous series of 121 patients. Surg Endosc 27:1766–1771
Bakker IS, Grossmann I, Henneman D, Havenga K, Wiggers T (2014) Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. Br J Surg 101:424–432
Cousin F, Ortega-Deballon P, Bourredjem A, Doussot A, Giaccaglia V, Fournel I (2016) Diagnostic accuracy of procalcitonin and C-reactive protein for the early diagnosis of intra-abdominal infection after elective colorectal surgery: a meta-analysis. Ann Surg
Moyes LH, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Preoperative systemic inflammation predicts postoperative infectious complications in patients undergoing curative resections for colorectal cancer. Br J Cancer 100:1236–1239
Kubo T, Ono S, Ueno H, Shinto E, Yamamoto J, Hase K (2013) Elevated preoperative C-reactive protein levels are a risk factor for the development of postoperative infectious complications following elective colorectal surgery. Langenbeck’s Arch Surg 398:965–971
González-Martínez S, Olona Tabueña N, Martín Baranera M, Martí-Saurí I, Moll JL, Má MG, et al. (2015) Proteínas mediadoras de la respuesta inflamatoria Como predictores de resultados adversos postoperatorios en pacientes quirúrgicos octogenarios: estudio prospectivo observacional. Cir Esp 93:166–173
Ortega-Deballon P, Radais F, Facy O, d’Athis P, Masson D, Charles PE, et al. (2010) C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J Surg 34:808–814
Nozoe T, Matsumata T, Sugimachi K (2000) Preoperative elevation of serum C-reactive protein is related to impaired immunity in patients with colorectal cancer. Am J Clin Oncol 23:263–266
WH H, LC C-M, Eisenstein S, Parry L, Cosman B, Ramamoorthy S (2015) Preoperative malnutrition assessments as predictors of postoperative mortality and morbidity in colorectal cancer: an analysis of ACS-NSQIP. Nutr J 14:91
Hennessey DB, Burke JP, Ni-Dhonochu T, Shields C, Winter DC, Mealy K (2010) Preoperative hypoalbuminemia is an independent risk factor for the development of surgical site infection following gastrointestinal surgery: a multi-institutional study. Ann Surg 252:325–329
Braga M, Wischmeyer PE, Drover J, Heyland DK (2013) Clinical evidence for pharmaconutrition in major elective surgery. JPEN J Parenter Enteral Nutr 37:66S–72S
Matsuda A, Furukawa K, Takasaki H, Suzuki H, Kan H, Tsuruta H, et al. (2006) Preoperative oral immune-enhancing nutritional supplementation corrects TH1/TH2 imbalance in patients undergoing elective surgery for colorectal cancer. Dis Colon Rectum 49:507–516
Okamoto Y, Okano K, Izuishi K, Usuki H, Wakabayashi H, Suzuki Y (2009) Attenuation of the systemic inflammatory response and infectious complications after gastrectomy with preoperative oral arginine and omega-3 fatty acids supplemented immunonutrition. World J Surg 33:1815–1821
Ortega-Deballon P, Ménégaut L, Fournel I, Orry D, Masson D, Binquet C, et al. (2015) Are adiponectin and leptin good predictors of surgical infection after colorectal surgery? A prospective study. Surg Infect 16:566–571
Lagabrielle JF, Tachet A, Boin V (2008) Dosage de la procalcitonine: comparaison des résultats obtenus sur Kryptor® (Brahms) et Vidas® (BioMérieux). Immunoanalyse Biol Spéc 23:245–250
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Royston P, Sauerbrei W (2004) A new approach to modelling interactions between treatment and continuous covariates in clinical trials by using fractional polynomials. Stat Med 23:2509–2525
Ataseven B, du Bois A, Reinthaller A, Traut A, Heitz F, Aust S, et al. (2015) Pre-operative serum albumin is associated with post-operative complication rate and overall survival in patients with epithelial ovarian cancer undergoing cytoreductive surgery. Gynecol Oncol 138:560–565
Bohl DD, Shen MR, Kayupov E, Della Valle CJ (2016) Hypoalbuminemia independently predicts surgical site infection, pneumonia, length of stay, and readmission after total joint arthroplasty. J Arthroplast 31:15–21
Frasson M, Flor-Lorente B, Rodriguez JL, Granero-Castro P, Hervás D, Alvarez Rico MA, et al. (2015) Risk factors for anastomotic leak after colon resection for cancer: multivariate analysis and nomogram from a multicentric, prospective, national study with 3193 patients. Ann Surg 262:321–330
Krarup PM, Jorgensen LN, Harling H, Group DCC (2014) Management of anastomotic leakage in a nationwide cohort of colonic cancer patients. J Am Coll Surg 218:940–949
Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA (2007) Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg 245:254–258
Kornmann VN, van Ramshorst B, Smits AB, Bollen TL, Boerma D (2014) Beware of false negative CT scan for anastomotic leakage after colonic surgery. Int J Color Dis 29:445–451
Telem DA, Chin EH, Nguyen SQ, Divino CM (2010) Risk factors for anastomotic leak following colorectal surgery: a case control study. Arch Surg 145:371–376
Mäkelä JT, Kiviniemi H, Laitinen S (2003) Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum 46:653–660
Golub R, Golub RW, Cantu R Jr, Stein HD (1997) A multivariate analysis of factors contributing to leakage of intestinal anastomosis. J Am Coll Surg 184:364–372
Zuo L, Li Y, Wang H, Zhu W, Zhang W, Gong J, et al. (2015) A practical predictive index for intra-abdominal septic complications after primary anastomosis for Crohn’s disease: change in C-reactive protein level before surgery. Dis Colon Rectum 58:775–781
Duvillard L, Ortega-Deballon P, Bourredjem A, Scherrer ML, Mantion G, Delhorme JB, et al. (2014) A case-control study of pre-operative levels of serum neutrophil gelatinase-associated lipocalin and other potential inflammatory markers in colorectal cancer. BMC Cancer 14:912
Ortega-Deballon P, Duvillard L, Scherrer M-L, Deguelte-Lardière S, Bourredjem A, Petit JM, et al. (2014) Preoperative adipocytokines as a predictor of surgical infection after colorectal surgery: a prospective survey. Int J Color Dis 29:23–29
Mullen JT, Davenport DL, Hutter MM, Hosokawa PW, Henderson WG, Khuri SF, et al. Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol 15:2164–2172
Gianotti L, Braga M, Nespoli L, Radaelli G, Beneduce A, Di Carlo V (2002) A randomized controlled trial of preoperative oral supplementation with a specialized diet in patients with gastrointestinal cancer. Gastroenterology 122:1763–1770
Akbarshahi H, Andersson B, Nordén M, Andersson R (2008) Perioperative nutrition in elective gastrointestinal surgery potential for improvement? Dig Surg 25:165–174
Marimuthu K, Varadhan KK, Ljungqvist O, Lobo DN (2012) A meta-analysis of the effect of combinations of immune modulating nutrients on outcome in patients undergoing major open gastrointestinal surgery. Ann Surg 255:1060–1068
Srinivasa S, Kahokehr AA, Yu TC, Hill AG (2011) Preoperative glucocorticoid use in major abdominal surgery: systematic review and meta-analysis of randomized trials. Ann Surg 254:183–191
Chapman SJ, Glasbey J, Kelly M, Khatri C, Nepogodiev D, Fitzgerald JE, et al. (2014) Impact of postoperative non-steroidal anti-inflammatory drugs on adverse events after gastrointestinal surgery. Br J Surg 101:1413–1423
Suezawa T, Aoki A, Kotani M, Tago M, Kobayashi O, Hirasaki A, et al. (2013) Clinical benefits of methylprednisolone in off-pump coronary artery bypass surgery. Gen Thorac Cardiovasc Surg 61:455–459
Acknowledgments
The authors are indebted to Elisabeth Devilliers, MD, for her heartfelt support to this project. The authors also thank the data monitoring board (Cassandra Porebski, Emilie Galizzi, Alexandra Felin, Amandine Martin, Fanny Lachaux, Donya Souhiel Da Costa, Joelle Fritsch, and Chrystelle Cappe), the safety monitoring board (Aurélie Grandvuillemin, PharmD), the administrative support team (Evelyne Phu and Maud Carpentier), the staff of the participant surgical departments for their help, Sandrine Vinault and Sandrine Daniel for their help with the statistical analysis, and Mr. Philip Bastable for the language revision of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent was obtained from all patients. The study was approved by the regional ethics committee CPP Est 1.
Funding source
The IMACORS study was funded by the Groupement de Coopération Sanitaire Grand-Est, the Regional Council of Burgundy, a French National Research Agency grant under the program “Investissements d’Avenir” (ANR-11-LABX-0021), and a grant from Brahms France SAS.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
De Magistris, L., Paquette, B., Orry, D. et al. Preoperative inflammation increases the risk of infection after elective colorectal surgery: results from a prospective cohort. Int J Colorectal Dis 31, 1611–1617 (2016). https://doi.org/10.1007/s00384-016-2620-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2620-8