Abstract
Aim of the study
The coexistence of Hirschsprung’s disease (HD) with anorectal malformation (ARM) is rare but many surgeons still ask pathologists to look for ganglia in the terminal rectum or fistula. In this study, we aimed to highlight the rarity of this association and question the necessity of histological evaluation.
Methods
After obtaining board review approval, rectal specimens of ARM patients who underwent corrective surgery in the last 8 years were re-analyzed by two blinded pathologists for the presence and structure of ganglia. Clinical and radiological data of patients retrieved from center records and correlated with histopathologic findings.
Main results
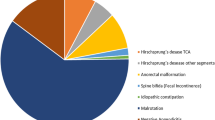
67 patients with ARM were identified, distal rectal specimen was obtained in 47. The median age at the time of surgery was 11 months (2 days–59 months). A normal pattern of ganglia was present in 51.1% (24/47), 29.7% (14/47) had aganglionosis and 19.1% (9/47) were inconclusive due to insufficient material. None of the aganglionic specimens showed other histological findings of HD. Patients were followed up regularly in the outpatient colorectal clinic for a median of 87 months (42–117 m). Only 6 experienced severe constipation (3 ganglionic, 2 no biopsy, 1 aganglionic), all of whom responded to a bowel management program, and none developed other manifestations of HD (abdominal distension, failure to thrive or enterocolitis) or required additional surgery.
Conclusions
Our results strongly suggest that the association of ARM and HD is extremely rare and the practice of searching for ganglia in the distal rectum or fistula of ARM patients should be discouraged to avoid potential misdiagnosis and overtreatment.


Similar content being viewed by others
References
Midrio P, Trovalusci E, Zanatta C et al (2020) Should the search for ganglia in the distal rectal fistula in patients with anorectal malformation be abandoned? J Pediatr Surg 55(10):2166–2169
Jiménez-Urueta PS, Alvarado-García R, Gallego-Grijalva JE (2005) Agangliosis del colon en pacientes con malformación anorectal. Análisis de 5 casos [Colon aganglionosis in patients with anorectal malformation. Analysis of five cases]. Cir Cir 73(4):283–285
Arbell D, Gross E, Orkin B et al (2006) Imperforate anus, malrotation, and Hirschsprung’s disease: a rare and important association. J Pediatr Surg 41(7):1335–1337
Eltayeb AA, Refaiy A (2020) Association of Hirschsprung’s disease with anorectal malformations: the early alarming signs for diagnosis and comorbidity related to this association. J Pediatr Surg 55(9):1981–1983
Bjørn N, Rasmussen L, Qvist N et al (2018) Full-thickness rectal biopsy in children suspicious for Hirschsprung’s disease is safe and yields a low number of insufficient biopsies. J Pediatr Surg 53(10):1942–1944
Holschneider A, Hutson J, Peña A et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
Kapur RP, Reed RC, Finn LS et al (2009) Calretinin immunohistochemistry versus acetylcholinesterase histochemistry in the evaluation of suction rectal biopsies for Hirschsprung disease. Pediatr Dev Pathol 12(1):6–15
Lukong CS, Mshelbwala PM, Anumah MA, Ameh EA, Nmadu PT (2012) Anorectal malformation coexisting with Hirschsprung’s disease: a report of two patients. Afr J Paediatr Surg 9:166–168
Vuille-Dit-Bille RN, de La Torre L, Hall J, Ketzer J et al (2021) Hirschsprung disease and anorectal malformations - an uncommon association. J Pediatr Surg 56(3):487–489. https://doi.org/10.1016/j.jpedsurg.2020.05.016
Holschneider AM, Ure BM, Pfrommer W et al (1996) Innervation patterns of the rectal pouch and fistula in anorectal malformations: a preliminary report. J Pediatr Surg 31(3):357–362
Pandey A, Pandey P, Singh SP et al (2018) Histology with immunohistochemistry of the fistula region in female anorectal malformation: can it be used for neo-anus reconstruction? J Paediatr Child Health 54(2):177–182
Raboei EH (2009) Patients with anorectal malformation and Hirschsprung’s disease. Eur J Pediatr Surg 19(5):325–327
Frenckner B, Husberg B (1991) Internal anal sphincter function after correction of imperforate anus. Pediatr Surg Int 6:202–206
Peña A, Levitt MA (2002) Colonic inertia disorders in pediatrics. Curr Probl Surg 39(7):666–730
Bischoff A, Levitt MA, Bauer C et al (2009) Treatment of fecal incontinence with a comprehensive bowel management program. J Pediatr Surg 44(6):1278–1284
Funding
The data that support the findings of this study are obtainable upon request from the corresponding author. The data are not publicly available due to ethical restrictions.
Author information
Authors and Affiliations
Contributions
EBCK and MOO designed the study, BGO and DSK performed histopathologic studies, EBCK and MOO collected and analyzed data, EBCK wrote the manuscript and GK provided technical support and conceptual advice. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cigsar Kuzu, E.B., Oztan, M.O., Ozamrak, B.G. et al. Rectal biopsy: is it really necessary in anorectal malformations?. Pediatr Surg Int 40, 22 (2024). https://doi.org/10.1007/s00383-023-05604-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05604-w