Abstract
Purpose
To describe the timing of chemotherapy initiation after surgery for Wilms tumor (WT) and neuroblastoma within a dedicated children’s cancer center.
Methods
A single-institution retrospective cohort study identified patients that underwent resection of unilateral WT or high-risk neuroblastoma and received adjuvant chemotherapy treatment. Adjuvant chemotherapy initiation and postoperative complications were recorded.
Results
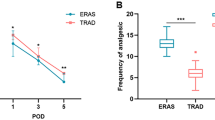
Among 47 WT patients, the median time to chemotherapy initiation was 11 days [interquartile range IQR 7–14]. 3 WT patients had post-operative complications, but all preceded chemotherapy. Among 83 patients treated for high-risk neuroblastoma, the median time to chemotherapy was 11 days [IQR 9–14]. High-risk neuroblastoma patients with 30-day postoperative complications had a significantly longer time to initiation of adjuvant chemotherapy (odds ratio 1.13; p = 0.008). Many of these complications preceded and delayed the initiation of post-operative chemotherapy. No complications occurred in the group of 12 (25%) WT patients or 16 (19.3%) neuroblastoma patients who started chemotherapy ≤ 7 days after surgery.
Conclusion
There is no association between early initiation of adjuvant chemotherapy and post-operative complications including wound healing. Early initiation of chemotherapy (≤ 7 days) is feasible in unilateral WT or high-risk neuroblastoma patients who are otherwise doing well without resulting in a preponderance of wound healing complications.




Similar content being viewed by others
References
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR (2016) SEER Cancer Statistics Review, 1975–2016. https://seer.cancer.gov/csr/1975_2016/
Deptula M et al (2019) Wound healing complications in oncological patients: perspectives for cellular therapy. Postepy Dermatol Alergol 36(2):139–146
Kalapurakal JA et al (2003) Influence of radiation therapy delay on abdominal tumor recurrence in patients with favorable histology Wilms’ tumor treated on NWTS-3 and NWTS-4: a report from the National Wilms’ Tumor Study Group. Int J Radiat Oncol Biol Phys 57(2):495–499
Phillips MR et al (2020) Implementation of a pediatric enhanced recovery pathway decreases opioid utilization and shortens time to full feeding. J Pediatr Surg 55(1):101–105
Rove KO et al (2020) Design and development of the Pediatric Urology Recovery After Surgery Endeavor (PURSUE) multicentre pilot and exploratory study. BMJ Open 10(11):039035
Ljungqvist O (2014) ERAS–enhanced recovery after surgery: moving evidence-based perioperative care to practice. JPEN J Parenter Enteral Nutr 38(5):559–566
Van Arendonk KJ, Chung DH (2019) Neuroblastoma: tumor biology and its implications for staging and treatment. Children (Basel) 6(1):12
Davidoff AM (2012) Wilms tumor. Adv Pediatr 59(1):247–267
Greenwood KL, Foster JH (2018) The safety of dinutuximab for the treatment of pediatric patients with high-risk neuroblastoma. Expert Opin Drug Saf 17(12):1257–1262
Smith V, Foster J (2018) High-risk neuroblastoma treatment review. Children (Basel) 5(9):114
Dome JS et al (2006) Treatment of anaplastic histology Wilms’ tumor: results from the fifth National Wilms’ Tumor Study. J Clin Oncol 24(15):2352–2358
Daw NC et al (2019) Treatment of stage I anaplastic Wilms’ tumour: a report from the Children’s Oncology Group AREN0321 study. Eur J Cancer 118:58–66
Franz MG, Steed DL, Robson MC (2007) Optimizing healing of the acute wound by minimizing complications. Curr Probl Surg 44(11):691–763
Guo S, Dipietro LA (2010) Factors affecting wound healing. J Dent Res 89(3):219–229
Payne WG et al (2008) Wound healing in patients with cancer. Eplasty 8:e9
Reyes-Habito CM, Roh EK (2014) Cutaneous reactions to chemotherapeutic drugs and targeted therapy for cancer: Part II. Targeted therapy. J Am Acad Dermatol 71(2):217.e1-217.e11
Brodeur GM et al (1993) Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol 11(8):1466–1477
Monclair T et al (2009) The International Neuroblastoma Risk Group (INRG) staging system: an INRG Task Force report. J Clin Oncol 27(2):298–303
Clavien PA et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Imran H et al (2009) Effect of time to resumption of chemotherapy after definitive surgery on prognosis for non-metastatic osteosarcoma. J Bone Joint Surg Am 91(3):604–612
Acknowledgements
This research was supported by The American Lebanese Syrian Associated Charities (ALSAC/St. Jude Children’s Research Hospital). This research was also supported by the Biostatistics Shared Resource of the St. Jude Comprehensive Cancer Center (NIH/NCI Comprehensive Cancer Center Support Grant# 5P30CA021765-41). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by AR, OG-Q, XW, ZL, LT, and AM. Writing—original draft preparation: AR, OG-Q, LT, and AM. Writing review and editing: AR, OG-Q, XW, ZL, HA, AD, LT, AM. Supervision: AD, LT, AM.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no conflicts of interest that are directly or indirectly related to the work to disclose. This study was declared exempt and deemed to be non-human subjects research by the St. Jude Children’s Research Hospital Institutional Review Board; waiver of informed consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ross, A., Gomez, O., Wang, X. et al. Timing of adjuvant chemotherapy after laparotomy for Wilms tumor and neuroblastoma. Pediatr Surg Int 37, 1585–1592 (2021). https://doi.org/10.1007/s00383-021-04968-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04968-1