Abstract
Purpose
To clarify the characteristics of gastroesophageal reflux (GER) in pediatric patients with neurological impairment (NI).
Methods
Twenty-six patients with NI, 1–17-year-old, fed via a nasogastric tube were categorized based on the absence (group I) or presence (group II) of abnormal GER, defined with multichannel intraluminal impedance-pH monitoring as %time with an esophageal pH <4.0 being ≥5.0% or number of liquid/mixed bolus reflux events(RE) >70 in 24 h.
Results
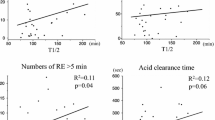
%Time and number of distal and proximal bolus REs were not significantly different between acid and nonacid REs. %Time of acid bolus RE and that of acid and total number of distal and proximal bolus REs were significantly higher in group II than in group I. Mean acid clearance time was significantly longer in group II. Median bolus clearance time was similar between the groups. No bolus RE parameters were significantly different between acid and nonacid REs in group I. Acid bolus RE was significantly higher than nonacid RE in terms of %time and number of proximal bolus RE in group II.
Conclusion
Acid REs significantly increased in pediatric patients with NI with abnormal GER. The number of acid and nonacid REs was comparable in patients without abnormal GER.





Similar content being viewed by others
References
Ravelli AM, Milla PJ (1998) Vomiting and gastroesophageal motor activity in children with disorders of the central nervous system. J Pediatr Gastroenterol Nutr 26:56–63
Penagini F, Mameli C, Fabiano V et al (2015) Dietary intakes and nutritional issues in neurologically impaired children. Nutrients 7:9400–9415
Del Buono R, Wenzl TG, Rawat D et al (2006) Acid and nonacid gastro-oesophageal reflux in neurologically impaired children: investigation with the multiple intraluminal impedance procedure. J Pediatr Gastroenterol Nutr 43:331–335
Fukahori S, Asagiri K, Ishii S et al (2013) Pre and post-operative evaluation of gastroesophageal reflux and esophageal motility in neurologically impaired children using combined pH-multichannel intraluminal impedance measurements. Pediatr Surg Int 29:545–551
Kawahara H, Tazuke Y, Soh H et al (2014) Does laparoscopy-aided gastrostomy placement improve or worsen gastroesophageal reflux in patients with neurological impairment? J Pediatr Surg 49:1742–1745
Pilic D, Fröhlich T, Nöh F et al (2011) Detection of gastroesophageal reflux in children using combined multichannel intraluminal impedance and pH measurement: data from the German Pediatric Impedance Group. J Pediatr 158:650–654
Lightdale JR, Gremse DA, Section on Gastroenterology, Hepatology, and Nutrition (2013) Gastroesophageal reflux: management guidance for the pediatrician. Pediatrics 131:e1684–e1695
Safe M, Cho J, Krishnan U (2016) Combined multichannel intraluminal impedance and pH measurement in detecting gastroesophageal reflux disease in children. J Pediatr Gastroenterol Nutr 63:e98–e106
Vicente Y, da Rocha C, Hernandez-Peredo G et al (2002) Esophageal acid clearance: more volume-dependent than motility-dependent in healthy piglets. J Pediatr Gastroenterol Nutr 35:173–179
Sifrim D (2005) Relevance of volume and proximal extent of reflux in gastro-oesophageal reflux disease. Gut 54:175–178
Kawahara H, Dent J, Davidson G (1997) Mechanisms responsible for gastroesophageal reflux in children. Gastroenterology 113:399–408
Herculano JR Jr, Troncon LE, Aprile LR et al (2004) Diminished retention of food in the proximal stomach correlates with increased acidic reflux in patients with gastroesophageal reflux disease and dyspeptic symptoms. Dig Dis Sci 49:750–756
Emerenziani S, Sifrim D (2005) Gastroesophageal reflux and gastric emptying, revisited. Curr Gastroenterol Rep 7:190–195
Acknowledgements
This study was supported by JSPS KAKENHI Grant Number 26462706 [Grant-in-Aid for Scientific Research (C)]. The authors would like to thank Enago (http://www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kawahara, H., Tazuke, Y., Soh, H. et al. Characteristics of gastroesophageal reflux in pediatric patients with neurological impairment. Pediatr Surg Int 33, 1073–1079 (2017). https://doi.org/10.1007/s00383-017-4139-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4139-7