Abstract
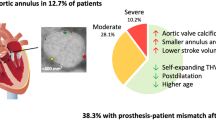
The objectives of the study were to evaluate the impact of aortic angulation (AA) on success of transcatheter aortic valve replacement (TAVR) with a new generation self-expandable prosthesis (Medtronic Evolut R®). Specific anatomical conditions, such as for example the presence of a horizontal aorta with elevated AA, have seemed to pose a significant challenge for the correct positioning and consequent functioning of self-expandable TAVR prostheses. We assessed 146 patients treated with Evolut R. AA was measured at computed tomography and two groups were identified using as cutoff the mean AA value. Acute outcomes were collected and compared. AA mean value was 49.6 ± 9.4° (AA ≥ 50°: 76 and AA < 50°: 70 patients). Risk profile (Logistic euroSCORE: AA ≥ 50°: 15.7; 75% IQR: 11.1–22.1 vs. AA < 50°: 14.7; 75% IQR: 10.7–24.0; p = 0.8) was equivalent. Perioperative results were similar: valve resheathing (AA ≥ 50°: 21.0% vs. AA < 50°: 24.2%; p = 0.6), recapturing (AA ≥ 50°: 19.7% vs. AA < 50°: 25.7%; p = 0.3), fluoroscopy time (AA ≥ 50°: 11.1 IQR: 8.6–17.0 min. vs. AA < 50°: 11.0 IQR: 8.0–15.7 min.; p = 0.9), and contrast agent use (AA ≥ 50°: 99.0 ± 41.8 ml. vs. AA < 50°: 104.2 ± 38.5 ml.; p = 0.4). At discharge, moderate paravalvular leak was present in 8/76 (10.5%) of the AA ≥ 50° and 6/70 (8.6%) of the AA < 50° (p = 0.7) patients. Severe paravalvular leak, implantation of a second valve, and/or conversion to surgery did not occur. Early safety (AA ≥ 50°: 7.8% vs. AA < 50°: 5.7%; p = 0.6) was similar in the two groups. AA did not affect procedural outcomes and valve performance of the Evolut R prosthesis.



Similar content being viewed by others
References
Sherif MA, Abdel-Wahab M, Stöcker B, Geist V, Richardt D, Tölg R, Richardt G (2010) Anatomic and procedural predictors of paravalvular aortic regurgitation after implantation of the Medtronic CoreValve bioprosthesis. J Am Coll Cardiol 56:1623–1629
Abramowitz Y, Maeno Y, Chakravarty T, Kazuno Y, Takahashi N, Kawamori H, Mangat G, Cheng W, Jilaihawi H, Makkar RR (2016) Aortic angulation attenuates procedural success following self-expandable but not balloon-expandable TAVR. JACC Cardiovasc Imaging 9:964–972
Manoharan G, Walton AS, Brecker SJ, Pasupati S, Blackman DJ, Qiao H, Meredith IT (2015) Treatment of symptomatic severe aortic stenosis with a novel resheathable supra-annular self-expanding transcatheter aortic valve system. JACC Cardiovasc Interv 8:1359–1367
Popma JJ, Reardon MJ, Khabbaz K, Harrison JK, Hughes GC, Kodali S, George I, Deeb GM, Chetcuti S, Kipperman R, Brown J, Qiao H, Slater J, Williams MR (2017) Early clinical outcomes after transcatheter aortic valve replacement using a novel self-expanding bioprosthesis in patients with severe aortic stenosis who are suboptimal for surgery: results of the Evolut R US Study. JACC Cardiovasc Interv 10:268–275
Willmann JK, Weishaupt D, Lachat M, Kobza R, Roos JE, Seifert B, Lüscher TF, Marincek B, Hilfiker PR (2002) Electrocardiographically gated multi-detector row CT for assessment of valvular morphology and calcification in aortic stenosis. Radiology 225:120–128
Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, Brott TG, Cohen DJ, Cutlip DE, van Es GA, Hahn RT, Kirtane AJ, Krucoff MW, Kodali S, Mack MJ, Mehran R, Rodés-Cabau J, Vranckx P, Webb JG, Windecker S, Serruys PW, Leon MB, Valve Academic Research Consortium-2 (2013) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document. J Thorac Cardiovasc Surg 145:6–23
Noble S, Roffi M (2014) Retrograde aortic valve crossing of the CoreValve prosthesis using the buddy balloon technique. Catheter Cardiovasc Interv 84:897–899
Sarkar K, Ussia GP, Tamburino C (2011) Trans catheter aortic valve implantation with core valve revalving system in uncoiled (horizontal) aorta. Overcoming anatomical and technical challenges for successful deployment. Catheter Cardiovasc Interv 78:964–969
Adams DH, Popma JJ, Reardon MJ, Yakubov SJ, Coselli JS, Deeb GM, Gleason TG, Buchbinder M, Hermiller J Jr, Kleiman NS, Chetcuti S, Heiser J, Merhi W, Zorn G, Tadros P, Robinson N, Petrossian G, Hughes GC, Harrison JK, Conte J, Maini B, Mumtaz M, Chenoweth S, Oh JK, US CoreValve Clinical Investigators (2014) Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med 370:1790–1798
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
D’Ancona, G., Kische, S., El-Mawardy, M. et al. Aortic annulus angulation does not attenuate procedural success of transcatheter aortic valve replacement using a novel self-expanding bioprosthesis. Heart Vessels 34, 1969–1975 (2019). https://doi.org/10.1007/s00380-019-01436-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01436-8