Abstract
Introduction
We evaluated the prognostic role of pre-salvage prostate-specific membrane antigen–radioguided surgery (PSMA-RGS) serum levels of alkaline phosphatase (AP), carcinoembryonic antigen (CEA), lactate dehydrogenase (LDH), and neuron-specific enolase (NSE).
Materials and methods
Patients who consecutively underwent PSMA-RGS for prostate cancer (PCa) oligorecurrence between January 2019 and January 2022 were selected. Biomarkers were assessed one day before surgery. Cox regression and logistic regression models tested the relationship between biochemical recurrence-free survival (BFS), 6- and 12-month biochemical recurrence (BCR), and several independent variables, including biomarkers.
Results
153 consecutive patients were analyzed. In the univariable Cox regression analysis, none of the biomarkers achieved predictor status (AP: hazard ratio [HR] = 1.03, 95% CI 0.99, 1.01; p = 0.19; CEA: HR = 1.73, 95% CI 0.94, 1.21; p = 0.34; LDH: HR = 1.01, 95% CI 1.00, 1.01; p = 0.05; NSE: HR = 1.02, 95% CI 0.98, 1.06; p = 0.39). The only independent predictor of BFS was the number of positive lesions on PSMA PET (HR = 1.17, 95% CI 1.02, 1.30; p = 0.03).
The number of positive lesions was confirmed as independent predictor for BCR within 6 and 12 months (BCR < 6 months: odds ratio [OR] = 1.1, 95% CI 1.0, 1.3; p = 0.04; BCR < 12 months: OR = 1.1, 95% CI 1.0, 1.3; p = 0.04).
Conclusion
The assessment of AP, CEA, LDH, and NSE before salvage PSMA-RGS showed no prognostic impact. Further studies are needed to identify possible predictors that will optimize patient selection for salvage PSMA-RGS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The widespread adoption of imaging techniques such as positron emission tomography (PET), using radiotracers targeting the prostate-specific membrane antigen (PSMA), has significantly improved the early detection of recurrent prostate cancer (PCa). This has proven to be particularly effective in identifying lesions in the pelvic region before systemic metastatic disease occurs, even at very low levels of prostate-specific antigen (PSA) [1,2,3].
Although the standard treatment for oligorecurrent hormone-sensitive prostate cancer (HSPC) usually consists of systemic combination treatment with androgen receptor-targeted agents (ARTA) and androgen deprivation therapy (ADT) [4,5,6], PSMA-radioguided surgery (RGS), which is still considered experimental, has been shown to be effective in removing PCa metastases and achieving consecutive PSA responses [7].
However, the greatest challenge lies in selecting the ideal candidate, as reliable biomarkers, nomograms or imaging techniques are not yet conclusive [8].
Recently, we attempted to evaluate the role of the European Association of Urology (EAU) risk groups for BCR and PSA kinetics (including PSA doubling time and PSA velocity) in the selection of patients for PSMA-RGS. According to their results, neither BCR risk groups nor PSA kinetics have an impact on the prediction of complete biochemical response, BCR-free and treatment-free survival in PSMA-RGS performed at low PSA values [8].
Thus, further guidance for patient selection by readily available biomarkers would be of great value. In the past, elevated serum levels of carcinoembryonic antigen (CEA), lactate dehydrogenase (LDH) and neuron-specific enolase (NSE) have already been described in the context of neuroendocrine dedifferentiation and aggressive-variant PCa [9]. According to the available literature, there is a possible correlation between elevated serum levels of NSE and prognosis in advanced PCa, particularly in the context of metastatic castration-resistant PCa (mCRPC) [10]. A recent meta-analysis found that elevated serum LDH levels are associated with an increased risk of mortality and progression in patients with “low volume” and “high volume” metastatic PCa [11]. The prognostic role of CEA is still controversial in PCa [12, 13]. Moreover, several clinical studies and a systematic review reported that alkaline phosphatase (AP) levels are associated with an increased risk of overall mortality and disease progression in patients with metastatic HSPC [14].
Thus, we aimed to assess the value of AP, CEA, LDH and NSE serum levels prior to PSMA-RGS in oligorecurrent PCa as potential tools for guiding treatment strategy and patient selection.
Materials and methods
Study cohort
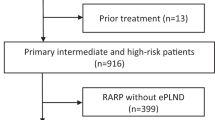
Patients who consecutively underwent PSMA-RGS for PCa pelvic, retroperitoneal or soft tissue oligorecurrence on PSMA PET between January 2019 and January 2022 were selected from our prospectively collected institutional review board-approved database (institutional review board (2019-PS-09; PV7316), Hamburg, Germany). Patients were selected for PSMA-RGS according to previously published criteria [7].
All patients had undergone radical prostatectomy (RP) as primary treatment, and subsequently were diagnosed with biochemical recurrence (BCR) with one or more positive soft tissue or lymph node lesions on PSMA PET. AP, CEA, LDH and NSE serum values were assessed one day prior to salvage surgery.
Patients were excluded from the analysis in case of ADT within six months prior to PSMA PET or involvement in a prospective clinical trial (n = 25). PSMA-RGS was performed as previously described [7, 15, 16].
Outcomes of interest
The rate of complete biochemical response (cBR, defined as PSA < 0.2 ng/ml) without any additional treatment was determined 2–16 weeks following PSMA-RGS. Furthermore, BCR-free survival (BFS) was assessed and calculated from the time of PSMA-RGS to the event (no cBR or PSA progression ≥ 0.2 ng/ml after cBR) or end of follow-up. Patients were censored on the date of last evidence of freedom from BCR or further treatment.
Statistical analysis
Descriptive statistics included frequencies and proportions for categorical variables. Means, medians, and ranges were reported for continuously coded variables.
To test if there are significant differences in the ordinal distributions of the level of biomarkers across the different levels of the location of positive lesions, the non-parametric Kruskal–Wallis test was performed.
Univariable and multivariable Cox regression models tested the relationship between BFS and several variables, namely, age at PSMA-RGS (continuously coded), Gleason grade group at RP (I–II vs III–V), pN stage at RP (N0/NX vs N1), radiation therapy (RT) after RP prior to PSMA-RGS (no vs yes), time between initial RP and PSMA-RGS (continuously coded), PSA prior PSMA-RGS (continuously coded), number of PSMA PET positive lesions prior to PSMA-RGS (continuously coded), levels of biomarkers before PSMA-RGS (AP, CEA, LDH, NSE, all continuously coded). Predictors were selected among potential factors previously published and associated with oncological outcomes after PSMA-RGS [7]. These were included in the multivariable models if significantly associated with the outcome in the univariable analysis.
Moreover, considering the potential clinical impact on patient selection, univariable logistic regression models were performed to test whether biomarkers above the normal range could predict early BCR (no vs yes) within 6 or 12 months [17].
For all statistical analyses, R software environment for statistical computing and graphics (version 4.1.2) was used. All tests were two sided, with a level of significance set at p < 0.05.
Results
Overall, 153 consecutive patients were analyzed.
Patients underwent PSMA-RGS at a median age of 66 years (IQR: 61, 70), and with a median PSA level of 0.6 ng/ml (IQR: 0.4, 1) (see Table 1; for initial patients’ characteristics see Supplementary Table 1).
The median values of AP, CEA, LDH, and NSE were 65 U/l (IQR: 56, 81), 0.8 µg/l (IQR: 0.5, 1.5), 197 U/l (IQR: 176, 213), and 14.3 µg/l (IQR: 12.1, 15.2), respectively (Table 1). Only in two (1.3%), ten (7%), eleven (7%) and 16 (10.4%) patients AP, CEA, LDH and NSE values were above the regular ranges. No significant correlation between the distribution of the biomarkers and the location of positive lesions was found (Supplementary Table 4).
Oncological outcomes
At 2–16 weeks after PSMA-RGS, 84 (55%) patients reached complete biochemical response. At a median follow-up of 13 months (IQR: 6, 24), 88 (57.5%) patients experienced BCR. The rate of BFS at 12 months was 43.3%. Within 6 and 12 months, 73 (48%) and 78 (51%) patients experienced BCR, respectively. The oncological outcomes of each patient according to the level of biomarkers assessed before PSMA-RGS are reported in Supplementary Fig. 1.
In the univariable Cox regression analysis, none of the biomarkers achieved predictor status, even coding the biomarkers as categorical variable with cut-off (AP: hazard ratio [HR] = 1.03, 95% confidence interval [CI]: 0.99, 1.01; p = 0.19; CEA: HR = 1.73, 95% CI 0.94, 1.21; p = 0.34; LDH: HR = 1.01, 95% CI 1.00, 1.01; p = 0.05; NSE: HR = 1.02, 95% CI 0.98, 1.06; p = 0.39) (Table 2). The only independent predictor of BFS was the number of positive lesions (HR = 1.17, 95% CI 1.02, 1.30; p = 0.03) (Table 2). PSA level performed prior to PSMA-RGS did not achieve predictor status (HR = 1.09, 95% CI 0.98, 1.21; p = 0.12) (Table 2). The number of positive lesions (HR = 1.19, 95% CI 1.04, 1.38; p = 0.01) was also confirmed as predictor of BFS in the multivariable model (Supplementary Table 5).
According to the univariable logistic regression analysis, none of the biomarkers above the normal range achieved the role of predicting BCR within 6 and 12 months (Supplementary Tables 2 and 3).
The number of positive lesions was confirmed as the only independent predictor for BCR within 6 and 12 months (BCR < 6 months: odds ratio [OR] = 1.1, 95% CI 1.0, 1.3; p = 0.04; BCR < 12 months: OR = 1.1, 95% CI 1.0, 1.3; p = 0.04) (Supplementary Table 2 and 3).
Discussion
In recent years, the widespread use of PSMA PET in both, staging and restaging, has sparked a strong interest in targeted imaging and individualized treatment strategies [1, 18]. This is particularly evident for open or robot-assisted PSMA-RGS as a patient-specific salvage treatment for PCa recurrence [19]. This technique has proven to be oncologically safe, as it effectively delays the start of systemic treatment in selected patients [7].
However, PSMA-RGS should still be considered experimental despite its encouraging results. One of the key requirements is the definition of clear criteria for patient selection. There is an unmet need to define the ideal candidates who would benefit most from salvage PSMA-RGS [7]. According to our previous analysis, patients with low PSA values at salvage surgery and a low number of PSMA-PET–avid lesions, ideally located in the pelvis, could derive the greatest benefit from PSMA RGS [7, 20].
In our analysis none of the tested serum biomarkers (AP, CEA, LDH and NSE) reached predictor status for BCR after PSMA-RGS on univariate analysis. The same results were reported in the additional analysis testing the role of biomarkers above the regular range in predicting BCR within 6 and 12 months. We hypothesize that the most important factor affecting the robustness of the models is the limited number of patients who had biomarkers beyond the regular range, and within this subgroup, those who experienced BCR.
In general, the literature exploring the role of biomarkers in oncologic outcomes of PCa is controversial. AP is one of the most widely studied markers which was found to be associated with OS and the risk of disease progression, but not with cancer-specific mortality in both, low and high volume metastatic HSPC [14, 19]. Nevertheless, Tsuzuki et al. developed a prognostic model including Gleason pattern 5, AP and LDH as predictors for a shorter time to CRPC and thus a poorer prognosis among patients with low-volume HSPC [21].
However, our results may not be directly comparable to the existing literature since we focused on patients with low metastatic burden, and we could hypothesize that biomarker values may increase in correlation with the extent of metastasis.
Most studies supporting the use of AP as a prognostic tool in the context of PCa treatment refer to metastatic CRPC [22, 23].
Similar considerations could be made for LDH, which is generally used as a marker of cancer burden in oncology. According to a recent systematic review and meta-analysis, LDH was associated with OS and PFS in patients with metastatic PCa [24]. However, most of the included studies were retrospective and had limited sample sizes, exclusion of patients with conditions that could affect LDH was not always specified, and LDH was categorized in the analysis with cutoff values that were not consistent within the original studies. Thus, caution should be taken when interpreting these results. Similar data were reported in the systematic review and meta-analysis by Mori et al. [11]. Nevertheless, only 14.3% of patients had HSPC, while the larger proportion was CRPC (85.7%).
Lastly, comparable thoughts should be given to NSE which could increase in CRPC compared to HSPC in the case of neuroendocrine transdifferentiation under androgen deprivation therapy [25]. Most of the studies reporting an association between increased NSE levels and poor prognosis are related to CRPC [10, 26]. Despite consistently incorporating CRPC, some studies did not confirm the prognostic role of NSE [25, 26].
Regarding CEA, the existing literature is limited to historical and small cohorts [27,28,29]. CEA was found to predict overall survival but not progression in patients with “anaplastic” small-cell prostate carcinoma during platinum-based chemotherapy [30]. Consistent with our findings, Nan et al. found that CEA levels provided prognostic information for breast cancer, gastric cancer and pancreatic cancer, but not for PCa [12].
However, taking all these aspects together and considering that this is the only study available in the literature on this topic, we believe that our results provide valuable insights into the tools that should or should not be considered in patient selection for PSMA-RGS.
In the current landscape, the most suitable candidates for salvage PSMA-RGS treatment are still patients with oligorecurrent disease, low PSA values and a limited number of positive lesions on PSMA-PET/CT, as shown in our previously published cohort.
Some limitations of our analysis should be mentioned. First, the study is constrained by a limited follow-up period. Due to limited follow-up in our cohort, it is not possible to have further insight on a stronger intermediate endpoint such as clinical progression. Moreover, the sample size is limited, and the number of events is low, thus the results of regression analysis should be interpreted with caution. Specifically, multivariable Cox regression models would have been prone to overfitting.
In conclusion, refining patient selection criteria is the crucial point to establishing the role of PSMA-RGS as a viable option for the treatment of recurrent PCa. In this context, while our results do not offer immediate or major clinical application, they do provide further insight into ongoing efforts to refine the ideal candidate. In the current scenario, we believe that all data, including negative data, has a valuable role to play in improving knowledge.
In the future evolving landscape, circulating tumour cells (CTCs) should be mentioned among the biomarkers that could play a prognostic role. In a pilot study, it was found that clinical and pathological outcomes are worse when CTCs can be detected in the blood preoperatively [31]. These results have laid the foundation for a prospective study (“BioPoP: Identification of Predictive Biomarkers” (NCT04324983)) investigating the predictive role of biomarkers in the selection of the ideal candidate for salvage PSMA-RGS.
Conclusion
The preoperative assessment of biomarkers, namely AP, CEA, LDH and NSE, before salvage PSMA-RGS for oligorecurrent PCa showed no prognostic significance. Further studies are needed to identify effective prognostic tools to optimize patient selection for salvage PSMA-RGS.
Data availability
Upon reasonable request raw data can be made available for research purposes in accordance with applicable data protection regulations.
Abbreviations
- ADT:
-
Androgen deprivation therapy
- AP:
-
Alkaline phosphatase
- ARTA:
-
Androgen receptor-targeted agents
- BCR:
-
Biochemical recurrence
- BFS:
-
Biochemical recurrence free survival
- cBR:
-
Complete biochemical response
- CEA:
-
Carcinoembryonic antigen
- CT:
-
Computed tomography
- HSPC:
-
Hormone-sensitive prostate cancer
- LDH:
-
Lactate dehydrogenase
- NSE:
-
Neuron specific enolase
- PCa:
-
Prostate cancer
- PET:
-
Positron emission tomography
- PSMA:
-
Prostate-specific membrane antigen
- RGS:
-
Radioguided surgery
- 99mTc:
-
99MTechnetium
- IQR:
-
Interquartile range
References
Berrens AC, Knipper S, Marra G, Van Leeuwen PJ, Van Der Mierden S, Donswijk ML et al (2023) State of the art in prostate-specific membrane antigen–targeted surgery—a systematic review. Eur Urol Open Sci 54:43–55
Maurer T, Eiber M, Schwaiger M, Gschwend JE (2016) Current use of PSMA–PET in prostate cancer management. Nat Rev Urol 13(4):226–235
Hofman MS, Lawrentschuk N, Francis RJ, Tang C, Vela I, Thomas P et al (2020) Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet Lond Engl 395(10231):1208–16
EAU EANM ESTRO ESUR ESUP SIOG Guidelines on Prostate Cancer 2022 (2022)
Armstrong AJ, Azad AA, Iguchi T, Szmulewitz RZ, Petrylak DP, Holzbeierlein J et al (2022) Improved survival with enzalutamide in patients with metastatic hormone-sensitive prostate cancer. J Clin Oncol Off J Am Soc Clin Oncol 40(15):1616–1622
Chi KN, Chowdhury S, Bjartell A, Chung BH, de PereiraSantana Gomes AJ, Santana, Gomes AJ, Given R et al (2021) Apalutamide in patients with metastatic castration-sensitive prostate cancer: final survival analysis of the randomized, double-blind, phase III TITAN study. J Clin Oncol Off J Am Soc Clin Oncol 39(20):2294–303
Knipper S, Mehdi Irai M, Simon R, Koehler D, Rauscher I, Eiber M et al (2023) Cohort study of oligorecurrent prostate cancer patients: oncological outcomes of patients treated with salvage lymph node dissection via prostate-specific membrane antigen-radioguided surgery. Eur Urol 83(1):62–69
Falkenbach F, Ambrosini F, Tennstedt P, Eiber M, Heck MM, Preisser F et al (2023) EAU biochemical recurrence risk classification and PSA kinetics have no value for patient selection in PSMA-radioguided surgery (PSMA-RGS) for oligorecurrent prostate cancer. Cancers 15(20):5008
Spetsieris N, Boukovala M, Patsakis G, Alafis I, Efstathiou E (2020) Neuroendocrine and aggressive-variant prostate cancer. Cancers 12(12):3792
Muoio B, Pascale M, Roggero E (2018) The role of serum neuron-specific enolase in patients with prostate cancer: a systematic review of the recent literature. Int J Biol Markers 33(1):10–21
Mori K, Kimura S, Parizi MK, Enikeev DV, Glybochko PV, Seebacher V et al (2019) Prognostic value of lactate dehydrogenase in metastatic prostate cancer: a systematic review and meta-analysis. Clin Genitourin Cancer 17(6):409–418
Nan J, Li J, Li X, Guo G, Wen X, Tian Y (2017) Preoperative serum carcinoembryonic antigen as a marker for predicting the outcome of three cancers. Biomark Cancer 9:1179299X1769014
Juang GD, Hwang TIS, Wang YH (2014) Metastatic prostate cancer with elevated serum levels of CEA and CA19-9. Urol Sci 25(1):28–30
Mori K, Janisch F, Parizi MK, Mostafaei H, Lysenko I, Enikeev DV et al (2020) Prognostic value of alkaline phosphatase in hormone-sensitive prostate cancer: a systematic review and meta-analysis. Int J Clin Oncol 25(2):247–257
Maurer T, Robu S, Schottelius M, Schwamborn K, Rauscher I, van den Berg NS et al (2019) 99mtechnetium-based prostate-specific membrane antigen-radioguided surgery in recurrent prostate cancer. Eur Urol 75(4):659–666
Robu S, Schottelius M, Eiber M, Maurer T, Gschwend J, Schwaiger M et al (2017) Preclinical evaluation and first patient application of 99m Tc-PSMA-I&S for SPECT imaging and radioguided surgery in prostate cancer. J Nucl Med 58(2):235–242
Wong NC, Lam C, Patterson L, Shayegan B (2019) Use of machine learning to predict early biochemical recurrence after robot-assisted prostatectomy. BJU Int 123(1):51–57
Roberts MJ, Chatfield MD, Hruby G, Nandurkar R, Roach P, Watts JA et al (2022) Event-free survival after radical prostatectomy according to prostate-specific membrane antigen-positron emission tomography and European Association of Urology biochemical recurrence risk groups. BJU Int 130(S3):32–39
Ambrosini F, Falkenbach F, Budäus L, Steuber T, Graefen M, Koehler D et al (2023) Comparative analysis of robot-assisted and open approach for PSMA-radioguided surgery in recurrent prostate cancer. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-023-06460-5
Roberts MJ, Maurer T, Perera M, Eiber M, Hope TA, Ost P et al (2023) Using PSMA imaging for prognostication in localized and advanced prostate cancer. Nat Rev Urol 20(1):23–47
Tsuzuki S, Kawano S, Fukuokaya W, Mori K, Nishikawa H, Tashiro K et al (2021) Prognostic model with alkaline phosphatase, lactate dehydrogenase and presence of Gleason pattern 5 for worse overall survival in low-risk metastatic hormone-sensitive prostate cancer. Jpn J Clin Oncol 51(11):1665–1671
Hammerich KH, Donahue TF, Rosner IL, Cullen J, Kuo HC, Hurwitz L et al (2017) Alkaline phosphatase velocity predicts overall survival and bone metastasis in patients with castration-resistant prostate cancer. Urol Oncol 35(7):460.e21-460.e28
Heinrich D, Bruland Ø, Guise TA, Suzuki H, Sartor O (2018) Alkaline phosphatase in metastatic castration-resistant prostate cancer: reassessment of an older biomarker. Future Oncol Lond Engl 14(24):2543–2556
Li F, Xiang H, Pang Z, Chen Z, Dai J, Chen S et al (2020) Association between lactate dehydrogenase levels and oncologic outcomes in metastatic prostate cancer: a meta-analysis. Cancer Med 9(19):7341–7351
Szarvas T, Csizmarik A, Fazekas T, Hüttl A, Nyirády P, Hadaschik B et al (2021) Comprehensive analysis of serum chromogranin A and neuron-specific enolase levels in localized and castration-resistant prostate cancer. BJU Int 127(1):44–55
Hvamstad T, Jordal A, Hekmat N, Paus E, Fosså SD (2003) Neuroendocrine serum tumour markers in hormone-resistant prostate cancer. Eur Urol 44(2):215–221
Ross RW, Beer TM, Jacobus S, Bubley GJ, Taplin M, Ryan CW et al (2008) A phase 2 study of carboplatin plus docetaxel in men with metastatic hormone-refractory prostate cancer who are refractory to docetaxel. Cancer 112(3):521–526
Loriot Y, Massard C, Gross-Goupil M, Di Palma M, Escudier B, Bossi A et al (2009) Combining carboplatin and etoposide in docetaxel-pretreated patients with castration-resistant prostate cancer: a prospective study evaluating also neuroendocrine features. Ann Oncol 20(4):703–708
Feuer JA, Lush RM, Venzon D, Duray P, Tompkins A, Sartor O et al (1998) Elevated carcinoembryonic antigen in patients with androgen-independent prostate cancer. J Investig Med Off Publ Am Fed Clin Res 46(2):66–72
Aparicio AM, Harzstark AL, Corn PG, Wen S, Araujo JC, Tu SM et al (2013) Platinum-based chemotherapy for variant castrate-resistant prostate cancer. Clin Cancer Res 19(13):3621–3630
Knipper S, Riethdorf S, Werner S, Tilki D, Graefen M, Pantel K et al (2021) Possible role of circulating tumour cells for prediction of salvage lymph node dissection outcome in patients with early prostate cancer recurrence. Eur Urol Open Sci 34:55–58
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Protocol/project development: Tobias Maurer, Gisa Mehring, Christina Steinbach. Data collection or management: Gisa Mehring, Christina Steinbach, Randi Pose. Data analysis: Francesca Ambrosini. Supervision: Tobias Maurer, Stefan Werner, Sabine Riethdorf, Gunhild von Amsberg, Daniel Koehler, Sophie Knipper. Manuscript writing/editing: Francesca Ambrosini, Tobias Maurer, Sophie Knipper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest relevant to the content of this manuscript. All authors directly participated in the planning, execution, or analysis of the study. This research received no specific grants from any funding agency in the public, commercial, or not-for-profit sector. The authors have no relevant financial interests to disclose.
Ethical approval
This study was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments and was approved by the local institutional review board.
Informed consent
All the patients included in the study provided written informed consent for the procedure and data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
345_2024_4948_MOESM4_ESM.jpg
Supplementary file4 Supplementary Figure 1: Scatter plot showing the oncological outcomes according to the levels of preoperative biomarkers in 153 consecutive patients who underwent salvage PSMA-radioguided surgery. The scatter plots depict the levels of the four biomarkers over time, with each point color-coded based on the presence or absence of BCR (JPG 100 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mehring, G., Steinbach, C., Pose, R. et al. Limited prognostic role of routine serum markers (AP, CEA, LDH and NSE) in oligorecurrent prostate cancer patients undergoing PSMA-radioguided surgery. World J Urol 42, 256 (2024). https://doi.org/10.1007/s00345-024-04948-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04948-9