Abstract
Purpose
Evaluate the percentage of patients with prostate cancer treated with luteinizing hormone-releasing hormone analogues (LHRHa) that develop castration resistance after a follow-up period of 3 years. The secondary objective is to evaluate the variables potentially related to the progression to castration resistant prostate cancer (CRPC).
Methods
A post-authorization, nation-wide, multicenter, prospective, observational, and longitudinal study that included 416 patients treated with LHRHa between 2012 and 2017 is presented. Patients were followed for 3 years or until development of CRPC, thus completing a per-protocol population of 350 patients. A Cox regression analysis was carried out to evaluate factors involved in progression to CRPC.
Results
After 3 years of treatment with LHRHa 18.2% of patients developed CRPC. In contrast, in the subgroup analysis, 39.6% of the metastatic patients developed CRPC, compared with 8.8% of the non-metastatic patients. The patients with the highest risk of developing CRPC were those with a nadir prostate-specific antigen (PSA) > 2 ng/ml (HR 21.6; 95% CI 11.7–39.8; p < 0.001) and those receiving concomitant medication, most commonly bicalutamide (HR 1.8; 95% CI 1–3.1, p = 0.0431).
Conclusions
The proportion of metastatic patients developing CRPC after 3 years of treatment with LHRHa is consistent with what has been previously described in the literature. In addition, this study provides new findings on CRPC in non-metastatic patients. Concomitant medication and nadir PSA are statistically significant predictive factors for the time to diagnosis of CRPC, the nadir PSA being the strongest predictor.
Similar content being viewed by others
Introduction
Prostate cancer (PC) is the second most common cancer, and the fifth most common cause of cancer-related mortality among male patients, worldwide. In Europe, the incidence of PC in men in 2020 exceeded that of lung cancer [1]. In developed countries, incidence is higher, possibly due to greater availability of prostate-specific antigen (PSA) testing [2, 3], and despite a significant mortality decrease (52% since 1993), PC remains the second cause of cancer-related death [2].
Androgen deprivation therapy (ADT) is the standard care for locally advanced and metastatic disease [4, 5]. PC cells require testosterone (T) and undergo apoptosis when lacking androgenic stimulation. T levels can be lowered with bilateral orchiectomy or administering LHRHa and antiandrogens. As bilateral orchiectomy has a potential psychological impact, drug therapy benefits outweigh the cost savings of surgery [5]. Complete androgen blockade (CAB) adds a non-steroidal antiandrogen (bicalutamide, flutamide, nilutamide) to therapy to inhibit adrenal androgens [6].
Although most PC patients respond to ADT, tumor cells may become androgen independent in 2–3 years [7, 8]. Multiple molecular mechanisms contribute to castration-resistant PC (CRPC), mostly involving the androgen receptor (AR) signaling pathway as an adaptative response to ADT [9]. In CRPC, PSA levels continue to rise in a low T level environment. Mortality of CRPC patients is high [10]. Despite several systemic therapies have demonstrated a survival advantage in metastatic castration resistant prostate cancer median overall survival based on real-world data may not exceed 2 years [10, 11]. Evidence shows that T levels < 20 ng/dL improve CRPC patient survival and delay disease progression [5, 9, 12]. Regular PSA and T level determinations predict treatment response and duration as well as disease progression, allowing for new strategies to be introduced [13,14,15].
Classical data revealed that only 7% of metastatic cancer patients treated with hormonal therapy were alive after 10 years with a mean response duration of 2.5 years [16]. Despite accumulating experience and knowledge of CRPC it is not well known how CRPC or median time to diagnosis of CRPC are influenced by epidemiological factors. The aim of this study is to evaluate the percentage of PC subjects in treatment with LHRH analogues who show castration-resistance state after a follow-up period of 3 years and to identify factors affecting poor prognosis.
Methods
Study design
ANARESISTANCE (Study number A-92-52014-204, Vall d’Hebron Hospital CEIm) was a post-authorization, prospective, observational, longitudinal study performed at 28 sites in Spain between 2012 and 2017. Prospective data were collected at four visits over 3 years: a baseline visit plus three visits 12 month apart. T and PSA levels were measured at each visit at local laboratories. We evaluated the percentage of LHRHa-treated PC patients developing CRPC, and identified factors related with CRPC development.
Patients
Eligibility criteria were age 18 years or older, histological confirmation of PC and suitability to ADT with any LHRHa according to the summary of product characteristics (SmPC) for at least 2 years or having initiated LHRHa within 1 year of inclusion. Exclusion criteria were participation in another clinical study, less than 3 years life expectancy and intention of intermittent ADT at inclusion or during the first 6 months. LHRHa selection and use followed routine clinical practice.
The study population included all patients who provided written informed consent and started LHRHa treatment. The per-protocol population included LHRHa-treated patients followed for 3 years after baseline with no major protocol deviations. Stratification based on metastatic status was performed at baseline. The indication for treatment with LHRHa in non-metastatic cases was adjuvant treatment to radiation therapy in high-risk patients and old symptomatic patients not-considered candidates or reluctant to local treatment.
Outcomes
The primary endpoint was the proportion of patients developing CRPC after 3 years of LHRHa. Secondary endpoints were median time to CRPC diagnosis and factors related to CRPC development. CRPC was defined as a serum T level < 50 ng/dl or < 1.7 nmol/L plus three consecutive increases of PSA, 1 week apart, resulting in two 50% increases over the nadir and PSA level > 2 ng/dl and anti-androgen withdrawal for at least 4 weeks (in the case of flutamide) and 6 weeks (in the case of bicalutamide) when used [17]. Furthermore, we aimed to estimate the median LHRHa treatment time until castration resistance. We evaluated whether age, race, PC personal and family history, stage (TNM classification), Gleason score, d’Amico risk classification, relapse, serum PSA level, serum T level and ECOG status influenced the time to castration-resistance.
The primary analysis was performed on the per-protocol population. Secondary analyses were conducted on the full study population.
Statistical analyses
We used SAS® software, version 9.4. The primary analysis was presented as absolute number and percentage of patients with an exact 95% confidence interval (CI). Time to CRPC was represented on Kaplan–Meier plots.
In the secondary analysis, a Cox regression model was used to identify factors potentially related to CRPC at 5% level. Predictive factors were identified by univariable and multivariable Cox regression analyses using a stepwise model with p = 0.2 entry and p = 0.05 stay criteria. PSA and T levels were analyzed by visit on the study population. Median T levels at visits 2, 3 and 4 were compared with median baseline T levels and among visits (visit 4 vs. visits 2 and 3) using the Wilcoxon Signed Rank test.
Results
Patient distribution is presented in Fig. 1. Patients who signed the informed consent and received at least one dose of an LHRHa composed the study population (n = 416). Forty-one patients were lost to follow-up (9.9%), and eight patients withdrew consent (1.9%). CRPC status was non assessable in 66 (15.9%) patients who were not included in the per-protocol population, defined as patients who received LHRHa for 36 months in whom development of CRPC was assessed (n = 350).
Characteristics of the study population
Mean ± SD age of the 416 patients in the study population, was 72.8 ± 8.18 years. The mean time between initial PC diagnosis and enrollment in the study was 15.6 ± 30.95 months. In 177 patients (42.5%) time since PC diagnosis to study enrollment was under 3 months. PC was diagnosed by screening in 274 patients (66%), the most frequent diagnosis method was PSA lab assay, (246; 89.8%). 38 (9.1%) patients had a family history of PC. Most patients had a good functional status (~ 60%, ECOG score = 0, ~ 25%, ECOG score = 1, at all visits). The most frequent comorbidities were cardiovascular in 191 patients (45.9%), metabolic in 118 (28.4%), renal in 65 (15.6%) and gastrointestinal in 43 (10.3%). During the study, 28 deaths were reported, none appeared related to the study drug.
Prostatectomy was performed in 61 patients (14.7%) and 83 (20%) received radiotherapy by baseline. In 199 patients (47.8%), LHRHa had been initiated before enrollment, and in 122 patients (30%) LHRHa was part of CAB. 379 patients (91.1%) received triptorelin 22.5 mg. Other LHRHa used were leuprolide in 32 (7.7%) and goserelin in 5 (1.2%). A total of 67 subjects (16.1%) received concomitant medication; the most commonly used was the antiandrogen bicalutamide (in 60 of 67 patients). Other concomitant medications included therapeutic radiopharmaceuticals (ten cases), abiraterone (three cases) and enzalutamide (three cases) and docetaxel (1 case). LHRHa was discontinued in 84 patients (20.2%) at a mean ± SD of 25.5 ± 10.6 months, never due to tolerability issues. LHRHa was discontinued due to exitus in 5 patients (6%), disease progression in 2 (2.4%), patient decision in 7 (8.3%), intermittent androgen blockade in 12 (14.3%), performance of radical prostatectomy) in 2 (2.4%), end of adjuvant radiation protocol in 52 (61.9%) and unknown cause in 4 (4.8%).
The baseline distribution of the study population according to TNM stage [18], Gleason score and T level is detailed in Table 1. Patients initiated on LHRHa at or after inclusion had higher T levels than those initiated before inclusion. Mean ± SD PSA level was 17.9 ± 36.69 ng/ml at screening visit (n = 400, 96.2%), and 23.2 ± 40.88 ng/ml before initiation of LHRHa (n = 286, 68.75%). Mean ± SD nadir PSA was 1.0 ± 5.71 ng/ml (n = 372, 89.4%): ≤ 2 ng/ml in 351 patients (94.4%) and > 2 ng/ml in 21 (5.6%). Mean ± SD time to the nadir PSA was 15.2 ± 9.64 months.
Evolution of PSA and testosterone levels
In the study population, mean PSA levels decreased for 24 months and remained stable at month 36 (Appendix B, Supplementary Material). Mean T level decreased at month 12 but increased at months 24 and 36. LHRHa-treated patients not reaching castration levels were 13.2%, 15% when castration level was set at 20 ng/dl.
Median ± interquartile range (IQR) T levels were lower at visits 2 (p < 0.0001), 3 (p < 0.0001) and 4 (p < 0.0001) than at screening, ranging from 120.5 ± 387 ng/dl at screening to 20.3 ± 57 ng/dl at visit 4. Notably, median ± IQR values were higher at visit 4 than at visits 2 and 3 (20.3 ± 57 ng/dl vs. 15.0 ± 26 (p < 0.0001) and 17 ± 19 ng/dl (p < 0.0001), respectively) (Appendix C, Supplementary Material).
Development of castration-resistance status
Since 64 (18.3%; 95% CI 14.38–22.74%) out of the 350 patients in the per-protocol population developed CRPC in 3 years, the median time to CRPC was non assessable. CRPC occurred in 36 of 90 metastatic patients (40%, 95% CI 29.81–50.87%) vs. 21 of 239 non-metastatic patients (8.8%, 95% CI 5.52–13.12%) (See in the Appendix A of the Supplementary Material a detailed distribution of CRPC status in the per protocol population at different times during follow-up and according to metastatic/non-metastatic and CAB status). Patients receiving CAB showed a trend to a higher rate of CRPC compared to patients not under CAB (21.6 vs 17.5%, 95% CI 14.04–30.81 and 12.91–22.91%). Of the 58 relapsing patients, 14 (24.1%, 95% CI 13.87–37.17%) developed CRPC, compared to 28 (18.9%, 95% CI 12.95–26.17%) of the 148 non-relapsing patients (relapse information was unavailable for 145 patients).
Although the median time to CRPC was non assessable, the 25th percentile of the time to CRPC diagnosis for the metastatic population was 28.5 (22.6–36.9) months (25th percentile non evaluable for non-metastatic patients). Figure 2 shows Kaplan–Meier curves for the time between LHRHa initiation and CRPC development.
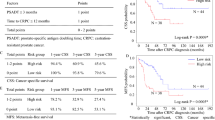
Factors potentially related to castration-resistance
Three factors were identified in the univariable Cox regression analysis: nadir PSA, total Gleason score, and any concomitant medication (Table 2). Of these, only the nadir PSA and any concomitant medication did not correlate with each other and were subsequently included in the multivariable analysis. In the multivariable analysis, patients with nadir PSA > 2 ng/ml had higher risk of CRPC than those with nadir PSA ≤ 2 ng/ml (HR 21.6, 95% CI 11.7–39.8; p < 0.001). Patients taking concomitant medication had higher risk of CRPC than those without concomitant medication (HR 1.8, 95% CI 1.0–3.1; p = 0.043).
Discussion
In this study, less than 10% of patients non-metastatic at ADT initiation developed CRPC after 3 years of continued treatment. In contrast, CRPC occurred in 40% of patients metastatic at diagnosis during the same time span. Based on previous reports, the percentage of CRPC patients in this study was lower than expected. At the time this study was designed, resistance to LHRHa in less than 3 years had been evaluated only in metastatic patients [19, 20].Our results are aligned with new studies that reported similar rates of CRPC after 3 years of ADT [21, 22]. The risk of CRPC increases in metastatic patients. Our results provide evidence of castration resistance in non-metastatic patients [23].
Differences in definitions of CRPC may mislead physicians to regard ADT as ineffective. Although some loss of effectiveness of ADT is to be expected given a high proportion of androgen-sensitive tumor cells, new combination therapies always include ADT to prevent repopulation of resistant cells [24, 25]. LHRHa have become the most widely used treatment of advanced/metastatic PC on account of their being better accepted than surgical castration, and having less cardiotoxicity than other hormonal treatments with comparable efficacy [17]. Nevertheless, some LHRHa may not reduce serum T below the castration level. A recent study concluded that triptorelin is a more potent agonist, than goserelin and leuprolide, and suggested that triptorelin may be most common in clinical practice in Spain, although the study site selection may not have been representative [26].
For a man with castration-resistant prostate cancer, there is a high probability that this will be the main cause contributing to his death. However, mortality varies in relation to tumor burden assessed as PSA doubling time and PSA at time of CRPC [10]. To date, there are no validated biomarkers of response or toxicity for CRPC other than models and prognostic factors [27, 28]. In our study, the nadir PSA and any concomitant medication were statistically significant predictors of time to CRPC. This is consistent with previous reports that validated concomitant medication as a predictive factor using phase III data [27]. Low molecular weight heparin and warfarin were associated with poorer survival whilst metformin and Cox2 inhibitors were associated with better outcomes [27]. Similarly, ≥ 1% PSA change after ADT was a strong predictor of shorter time to CRPC and overall survival in CRPC metastatic patients [28].
Limitations of this study should include few metastatic patients included (27%), and short follow-up of non-metastatic patients. Also, median time to CRPC was non assessable due to few patients reaching CRPC status. Finally, liquid chromatography with tandem mass spectrometry may not have been used in all local laboratories which may have caused heterogeneity. Another limitation of the study stands in that the influence of previous local treatment (prostatectomy and/or radiotherapy) has not been registered and therefore it could not be evaluated as a potential predictor for development of castration resistance. Finally, the influence of new therapeutic developments in the field of hormone sensitive metastatic PC, such as the use of enzalutamide or apalutamide [29, 30], have not been considered due to the time interval patients were recruited but could likely modify the perspective of CRPC development.
Conclusion
Despite efforts to develop new therapies, resistance to castration remains a challenge for advanced PC management. This study shows that after 3 years of ADT, nearly 20% of patients developed CRPC; nadir PSA and concomitant medication being predictive factors of the time to CRPC.
Data availability
Where patient data can be anonymized, Ipsen will share all individual participant data that underlie the results reported in this article with qualified researchers who provide a valid research question. Study documents, such as the study protocol and clinical study report, are not always available. Proposals should be submitted to DataSharing@Ipsen.com and will be assessed by a scientific review board. Data are available beginning 6 months and ending 5 years after publication; after this time, only raw data may be available.
References
Leith A, Kim J, Ribbands A, Clayton E, Yang L, Ghate SR (2022) Real-world treatment patterns in metastatic Castration-Resistant Prostate Cancer across Europe (France, Germany, Italy, Spain, and the United Kingdom) and Japan. Adv Ther 39:2236–2255. https://doi.org/10.1007/s12325-022-02073-w
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics, 2021. CA Cancer J Clin 71(1):7–33. https://doi.org/10.3322/caac.21654
Pernar CH, Ebot EM, Wilson KM, Mucci LA (2018) The epidemiology of prostate cancer. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a030361
Singer EA, Golijanin DJ, Miyamoto H, Messing EM (2008) Androgen deprivation therapy for prostate cancer. Expert Opin Pharmacother 9(2):211–228. https://doi.org/10.1517/14656566.9.2.211
Crawford ED, Heidenreich A, Lawrentschuk N, Tombal B, Pompeo ACL, Mendoza-Valdes A et al (2019) Androgen-targeted therapy in men with prostate cancer: evolving practice and future considerations. Prostate Cancer Prostatic Dis [Internet] 22(1):24–38. https://doi.org/10.1038/s41391-018-0079-0
Miller DR, Ingersoll MA, Teply BA, Lin MF (2021) Chapter 5. Combination treatment options for castration-resistant prostate cancer. In: Bott SRJ, Ng KL (eds) Prostate cancer [Internet]. Exon Publications, Brisbane. https://doi.org/10.36255/exonpublications.prostatecancer.combinationtreatment.2021
Arnold JT, Isaacs JT (2002) Mechanisms involved in the progression of androgen-independent prostate cancers: It is not only the cancer cell’s fault. Endocr Relat Cancer 9(1):61–73. https://doi.org/10.1677/erc.0.0090061
Harris WP, Mostaghel EA, Nelson PS, Montgomery B (2009) Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol 6(2):76–85. https://doi.org/10.1038/ncpuro1296 (Erratum in: Nat Clin Pract Urol. 2009 Mar;6(3):173)
Murray TBJ (2021) Chapter 3. The pathogenesis of prostate cancer. In: Bott SRJ, Ng KL (eds) Prostate cancer [Internet]. Exon Publications, Brisbane. https://doi.org/10.36255/exonpublications.prostatecancer.pathogenesis.2021
Aggarwal R, Ryan CJ (2011) Castration-resistant prostate cancer: targeted therapies and individualized treatment. Oncologist 16(3):264–275. https://doi.org/10.1634/theoncologist.2010-0216
Khoshkar Y, Westerberg M, Adolfsson J, Bill-Axelson A, Olsson H, Eklund M et al (2021) Mortality in men with castration-resistant prostate cancer-A long-term follow-up of a population-based real-world cohort. BJUI Compass 3(2):173–183. https://doi.org/10.1002/bco2.116
Anton A, Pillai S, Semira MC, Wong S, Shapiro J, Weickhardt A et al (2021) Real-world first-line systemic therapy patterns in metastatic castration-resistant prostate cancer. BJUI Compass 3(3):205–213. https://doi.org/10.1002/bco2.129
Tremblay S, Summers-Trasiewicz L, Pouliot F, Crook JM, Ding K, Klotz L, Toren P (2021) Interpreting testosterone and concomitant prostate specific antigen values during androgen deprivation therapy for recurrent prostate cancer. J Urol. https://doi.org/10.1097/JU.0000000000001946
Perachino M, Cavalli V, Bravi F (2010) Testosterone levels in patients with metastatic prostate cancer treated with luteinizing hormone-releasing hormone therapy: prognostic significance? BJU Int 105(5):648–651. https://doi.org/10.1111/j.1464-410X.2009.08814.x
Klotz L, O’Callaghan C, Ding K, Toren P, Dearnaley D, Higano CS et al (2015) Nadir testosterone within first year of androgen-deprivation therapy (ADT) predicts for time to castration-resistant progression: a secondary analysis of the PR-7 trial of intermittent versus continuous ADT. J Clin Oncol 33(10):1151–1156. https://doi.org/10.1200/JCO.2014.58.2973
Tangen CM, Faulkner JR, Crawford ED, Thompson IM, Hirano D, Eisenberger M et al (2003) Ten-year survival in patients with metastatic prostate cancer. Clin Genitourin Cancer 2(1):41–45. https://doi.org/10.3816/cgc.2003.n.011
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, Van Der Kwast T et al (2014) EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol [Internet] 65(2):467–479. https://doi.org/10.1016/j.eururo.2013.11.002
American Cancer Society. Prostate Cancer Early Detection , Diagnosis , and Staging. Am Cancer Soc [Internet]. 2017;1–25. Available from: https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging.html. Accessed 1 Sept 2022
Debruyne FM (1988) Results of a Dutch trial with the LHRH agonist buserelin in patients with metastatic prostatic cancer and results of EORTC studies in prostatic cancer. Am J Clin Oncol 11(Suppl 1):S33–S35
Oosterlinck W, Mattelaer J, Derde MP, Kaufman L (1995) Prognostic factors in advanced prostatic carcinoma treated with total androgen blockade. Flutamide with orchiectomy or with LHRH analogues. A Belgian multicentric study of 546 patients. Acta Urol Belg 63(3):1–9
de la Taille A, Martínez-Piñeiro L, Cabri P, Houchard A, Schalken J (2017) Factors predicting progression to castrate-resistant prostate cancer in patients with advanced prostate cancer receiving long-term androgen-deprivation therapy. BJU Int 119(1):74–81. https://doi.org/10.1111/bju.13455
Shore ND, Laliberté F, Ionescu-Ittu R, Yang L, Mahendran M, Lejeune D et al (2021) Real-world treatment patterns and overall survival of patients with metastatic castration-resistant prostate cancer in the US prior to PARP inhibitors. Adv Ther. https://doi.org/10.1007/s12325-021-01823-6
Sternberg CN, Baskin-Bey ES, Watson M, Worsfold A, Rider A, Tombal B (2013) Treatment patterns and characteristics of European patients with castration-resistant prostate cancer. BMC Urol. https://doi.org/10.1186/1471-2490-13-58
Shore ND, Morgans AK, Ryan CJ (2020) Resetting the bar of castration resistance—understanding androgen dynamics in therapy resistance and treatment choice in prostate cancer. Clin Genitourin Cancer [Internet] 19(3):199–207. https://doi.org/10.1016/j.clgc.2020.08.008
Rove KO, Crawford ED (2013) Androgen annihilation as a new therapeutic paradigm in advanced prostate cancer. Curr Opin Urol 23(3):208–213. https://doi.org/10.1097/MOU.0b013e32835fa889
Shim M, Bang WJ, Oh CY, Lee YS, Cho JS (2019) Effectiveness of three different luteinizing hormone-releasing hormone agonists in the chemical castration of patients with prostate cancer: goserelin versus triptorelin versus leuprolide. Investig Clin Urol 60(4):244–250. https://doi.org/10.4111/icu.2019.60.4.244
Pitcher B, Khoja L, Hamilton RJ, Abdallah K, Pintilie M, Joshua AM (2017) Assessment of a prognostic model, PSA metrics and toxicities in metastatic castrate resistant prostate cancer using data from project data sphere (PDS). PLoS ONE 12(2):1–12. https://doi.org/10.1371/journal.pone.0170544
Nakanishi S, Goya M, Tamaki M, Oshiro T, Saito S (2021) Three-month early change in prostate-specific antigen levels as a predictive marker for overall survival during hormonal therapy for metastatic hormone-sensitive prostate cancer. BMC Res Notes 14(1):4–9. https://doi.org/10.1186/s13104-021-05641-5
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S et al (2019) Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med 381(2):121–131. https://doi.org/10.1056/NEJMoa1903835
Chi KN, Chowdhury S, Bjartell A, Chung BH, de Santana P, Gomes AJ, Given R et al (2021) Apalutamide in patients with metastatic castration-sensitive prostate cancer: final survival analysis of the randomized, double-blind, phase III TITAN study. J Clin Oncol 39(20):2294–2303. https://doi.org/10.1200/JCO.20.03488
Acknowledgements
José Manuel Abascal (Hospital Central Universitario de Asturias, Oviedo); Víctor Barrondo (Hospital Universitario de Basurto, Bilbao); Antonio Benedicto (Hospital Universitario de la Ribera, Alzira); Ana Carballo (Hospital Clínico Universitario de Santiago, Santiago de Compostela); José Ramón Cortiñas (Hospital General de Valladolid); Manuel Fernández (Hospital Universitario del Henares, Coslada); Eduardo Ferrer (Hospital Clínico Universitario de Valencia); Pablo Luís Guzmán (Hospital General Universitario Los Arcos del Mar Menor, Murcia); Miguel Ángel López (Hospital Comarcal Santiago Apóstol, Miranda de Ebro); José Carlos Martínez (Hospital Universitario Nuestra Señora de Candelaria, Santa Cruz de Tenerife); Carlos Olivier (Hospital Universitario de la Princesa, Madrid); Paula Peleteiro (Hospital Clínico Universitario de Santiago, Santiago de Compostela); Pedro Julio Pérez (Hospital Virgen del Puerto, Plasencia); Daniel Pesqueira (Hospital de Povisa, Vigo); José Ponce (Hospital de A Coruña, A Coruña); Manuel Ruibal (Hospital Montecelo, Pontevedra); Josep Segarra (Hospital Universitario Joan XXIII, Tarragona); Eduardo Solsona (Instituto Valenciano de Oncología, Valencia); José Francisco Suárez (Hospital Universitario de Bellvitge, Hospitalet de Llobregat); José Rosa (Hospital Comarcal Santiago Apóstol, Miranda de Ebro); Ángel Tabernero (Hospital Universitario La Paz, Madrid); Félix Vesga (Hospital Universitario de Burgos); Almudena Zapatero (Hospital Universitario de la Princesa, Madrid).
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was funded by Ipsen Pharma S.A.U.
Author information
Authors and Affiliations
Consortia
Contributions
JCA, JPCS, JAG-L, JMGG, AG-C, JLGS, RPC, MPS, VP, JPM: protocol/project development. JCA, JPCS, JAG-L, JMGG, AG-C, JLGS, RC, JPM: data collection or management. MPS, VP, JPM: data analysis. JCA, JPCS, JAG-L, JMGG, AG-C, JLGS, RPC, MPS, VP, JPM: manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
Pérez Sampietro M. and Perrot V. are employees of Ipsen Pharma S.A.U. The other authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Before initiating the study, written and dated approval was obtained from all Independent Ethics Committee of the institutions involved.
Consent to participate
Informed consent was obtained from all individual participants before any study-specific assessment or procedure was performed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Angulo, J.C., Ciria Santos, J.P., Gómez-Caamaño, A. et al. Development of castration resistance in prostate cancer patients treated with luteinizing hormone-releasing hormone analogues (LHRHa): results of the ANARESISTANCE study. World J Urol 40, 2459–2466 (2022). https://doi.org/10.1007/s00345-022-04108-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04108-x