Abstract
Purpose
To ascertain renal cell carcinoma (RCC) financial toxicity on COVID-19 during the COVID-19 crisis as patients are struggling with therapeutic and financial implications.
Methods
An online survey was conducted from March 22 to March 25, 2020. It included baseline demographic, clinicopathologic, treatment-related information, anxiety levels related to COVID-19, questions related to financial concerns about COVID-19 as well as the validated 11-item COST measure.
Results
Five-hundred-and-thirty-nine patients (39%:58% male:female) from 14 countries responded. 23% of the patients did not feel in control of their financial situation but 8% reported being very satisfied with their finances. The median COST score was 21.5 (range 1–44). Metastatic patients who have not started systemic therapy had a COST score (19.8 range 2–41) versus patients on oral systemic therapy had a COST score (23.9 range 4–44). Patients in follow-up after surgery had a median COST score at 20.8 (range 1–40). A low COST scores correlated (p < 0.001) were female gender (r = 0.108), younger age (r = 0.210), urban living situation (r = 0.68), a lower educational level (r = 0.155), lower income (r = 0.165), higher anxiety about acquiring COVID-19 (r = 0.198), having metastatic disease (r = 0.073) and a higher distress score about cancer progression (r = 0.224).
Conclusion
Our data highlight severe financial impact of COVID-19. Acknowledging financial hardship and thorough counseling of cancer patients should be part of the conversation during the pandemic. Treatment and surveillance of RCC patients might have to be adjusted to contemplate financial and medical needs.
Similar content being viewed by others
Introduction
Much has been written about how the COVID-19 crisis is placing immense strain on healthcare systems worldwide. As a consequence, there has been a rush to develop guidelines around every element of cancer care, ranging from use of surgery, radiation, systemic therapy to supportive care modalities [1,2,3,4]. Practice changes have been implemented to reduce touchpoints for patients and to preserve hospital resources for COVID-19 patients. However, less research has focused on how the crisis is impacting individuals being treated for cancer, including adverse effects of financial toxicity.
Advances in care for patients with renal cell carcinoma have dramatically changed over the last decade, improving outcomes and increasing overall survival for patients. However, these advances have occurred during a time when insurance plans have also increased cost-sharing, shifting a greater proportion of treatment costs directly to the patient [5].
An estimated 2.7 billion people have been impacted by coronavirus lockdowns and according to the United Nations Conference on Trade and Development, the global economy could lose $2 trillion as a result of the crisis [6].
Advances in cancer care become meaningless if patients cannot afford them or if the patients’ prognoses continue to be determined by where they live or how good their insurance is [7].
We conducted an online survey to ascertain (a) patient anxiety level around COVID-19 and (b) implications on financial burden.
Materials and methods
Survey development and distribution
The survey was developed by the Kidney Cancer Research Alliance (KCCure), with multidisciplinary representation from two surgeons (MS, DP), medical oncologist (SKP), psychologist (CB) and patient advocate (DB). The survey included a total of 45 items (detailed subsequently) and was initially evaluated by a separate group of patient advocates for ease of interpretability. The open survey was then broadcast to the KCCure membership through a patient mailing list of n = 1532 subscribers maintained by the organization and was also distributed through online social media platforms (specifically, Facebook and Twitter). Multiple responses from the same patient were prohibited by the system via anonymized IP address tracking. IRB was not obtained as the survey was a patient organization’s effort. No personal data were collected in the de-personalized questionnaire and prior to taking the survey patients gave informed consent for data use and analysis.
Survey composition
The survey is included as Supplementary Appendix 1. Briefly, the survey included demographic features including age, gender, race, educational level and income level. Patients were queried regarding their perceived risk of COVID-19, and their anxiety level related to both COVID-19 and cancer progression was quantified using a Likert scale ranging from 0 to 10.
Further questions were based on disease status. Patients in surveillance were queried regarding their current plan for surveillance. Patients receiving systemic treatment were queried regarding the nature of systemic therapy they were receiving.
The survey contained items pertaining to distress level, financial hardship, medical and behavioral expectations that were quantified on a Likert scale ranging from 0 to 3. To assess financial burden, the validated comprehensive score for financial toxicity (COST) patient-reported outcome measure was included. The lower the score, the worse the financial toxicity [8].
Statistical analysis
Descriptive statistics with graphical outputs were used to characterize survey results.
Pearson’s correlation (r) and Kendal’s tau test were used to analyze the COST questionnaire, financial burden and hardship, as well as medical and behavioral expectations. Significance levels were two-tailed. All statistical analyses were carried out with SPSS Statistics Vers. 26 (IBM Analytics, Armonk, NY, USA).
Results
Patient characteristics
Responses were received via e-mail and social media. With a response rate of 35% and 539 total respondents, 280 patients (52%) had metastatic disease, 187 patients (35%) had prior surgery for localized disease and 23 patients (5%) had localized disease awaiting surgery (Table 1). Median age was 55 (range, 24–87) with 58% females and 39% males. Most patients had obtained a bachelor or graduate degree (44%) and live in the United States (87%). In addition, the majority of patients are receiving treatment at an academic center (37%), followed by regional centers (30%) and private practices (18%). Patients were predominantly white (88%) and well educated (58% had college or graduate degree. The majority had a household income that ranged between $50,000 and $99,999 (30%) or higher than $100,000 (38%). The majority of participants live in suburban areas (52%). Socioeconomic and clinical characteristics were statistically not significantly different between groups and are described in Table 1.
COVID-19 and expected hardships
The majority of patients expect the pandemic to induce medical, behavioral, psychological and financial hardship. Only 17% do not expect medical, 25% behavioral, 16% psychological and 13% financial hardship to occur as a result of COVID-19. Patients with an income of less than US $50,000 were significantly more anxious about financial hardship than people with a high income (> US $100,000) (93% vs 82%, p < 0.001).
Patients with a higher anxiety about acquiring COVID-19 were significantly (p < 0.001) more likely to expect medical (r = 0.212), behavioral (r = 0.178) and psychological hardship (r = 0.304).
Financial anxiety
The majority of patients (59%) were concerned that their money in savings or retirements assets would not cover the cost of their treatment. Only 8% were satisfied with their financial situation and 25% were financially stressed. More than a quarter of the patients (26%) were concerned about losing their job and income and 32% claim that their cancer treatment has reduced their satisfaction with their present financial situation. Half of the patients do not feel in control of their financial situation and only 8% were confident about their finances.
Educational and income level
Patients with a higher educational level or a higher income were significantly more often living in urban areas and were more likely to be treated at an academic center (p < 0.001). Compared to patients with a lower educational or income level, they did not have higher anxiety related to acquiring COVID-19 and had the same level of cancer distress.
COST score assessment
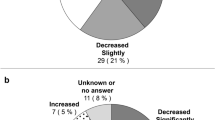
The median COST score of all patients was 21.5 (range 1–44). Detailed responses are shown in Table 2. Metastatic patients who have not started systemic therapy had the lowest median COST score (19.8 range 2–41) versus patients on systemic therapy with oral treatments had the highest median COST score (23.9 range 4–44). Interestingly, patients in follow-up after surgery also had a lower median COST score at 20.8 (range 1–40) (see Fig. 1).
Factors significantly (p < 0.001) contributing to a lower COST score were female gender (r = 0.108), younger age (r = 0.210), urban living situation (r = 0.68), a lower educational level (r = 0.155), lower income (r = 0.165), higher anxiety about acquiring COVID-19 (r = 0.198), having metastatic disease (r = 0.073) and a higher distress score about cancer progression (r = 0.224) (see Fig. 2).
Nationality and race were not correlated with financial distress in our dataset.
Discussion
Our study reveals that while patients experience heightened anxiety about increasing financial hardship related to COVID-19, they remain substantially concerned about cancer recurrence and progression. In the overall population, 71% felt they had a heightened risk for COVID-19 infection; however, only 27% of patients contacted their treating physicians to confirm this information. Patients with RCC seem unwilling to compromise planned surveillance for localized disease or planned systemic therapy for metastatic disease.
In our cohort, anxiety related to financial hardship is very high, mainly in patients with a moderate-to-high income and higher educational level.
The median COST score in our cohort of RCC patients is 21.5, which is somewhat lower than previously described cohorts of cancer patients in general, where it was at 23, indicating that pandemic might be increasing financial anxiety [8,9,10].
Although oral systemic therapy based on tyrosine-kinase inhibitors has one of the highest co-pays for patients [9], this was the subgroup of respondents that expected the lowest financial hardship with a COST score of 23.9. Patients prior to surgery had the one of the lowest scores at 20.0, which could be a reflection of the fear of future costs versus actual cost. The lower rates of financial concern for patients receiving oral therapy could be due to the fact that these drugs are more commonly used in later-line treatment, reflecting a patient population that has more experience with treatment resulting in lower anxiety levels related to cost. In line with previous findings, younger patients were more likely to be anxious about financial hardship and might need additional counseling and a specific plan to address this anxiety [9].
Interestingly, patients who have been diagnosed with cancer, but have not yet had treatment, expressed higher anxiety about financial toxicity versus patients already on therapy. This was true for both metastatic patients and patients with localized disease. It could be that uncertainty related to future costs is a larger driver of financial toxicity rather than the actual realized cost of treatments for patients. This might indicate a need for increased counseling for patients who are newly diagnosed and could be experiencing anxiety due to the uncertainty related to potential financial costs (Fig. 2).
This concern related to uncertainty of future costs is also evident in the responses related to the COST questionnaire. When asked about confidence in covering the cost of treatment, 41% indicate that they are not at all confident that they have enough money in their savings or retirement. Yet, when asked whether their out-of-pocket expenses were more than they thought they would be, only 12% said “very much”. Only 6% of patients said that they feel satisfied with their current situation, but when asked if they were able to meet their monthly expenses, only 8% indicated that they were not able to do so. When asked if they felt in control of their financial situation, less than 10% indicated that they were. But again, when asked if their cancer or treatment had reduced their satisfaction with their present financial situation, only 16% said very much.
Uncertainty in cancer is one of the most significant forms of distress in cancer patients [11]. It could be that the specter of future costs, fear related to inability to care for their family as their disease progresses, could be more important drivers to consider when measuring financial toxicity.
Research related to patient-reported outcomes, while rapidly advancing in cancer care, is still poorly understood in renal cell carcinoma. Despite demands from patient advocacy organizations, patient values concerning treatment decisions are yet to be defined and poorly described and understood [12]. Repeated assessment and analyses to differentiate trends from principles are needed. Nonetheless, the high rates of anxiety highlight the need to address financial toxicity as a standard part of care for kidney cancer patients.
Comparing these numbers needs to be done with caution as there has not been a COST analysis in RCC so far. As the COST score observed in our patient cohort is comparable to other disease areas, we are confident it reflects on the real situation. As there is uncertainty and the fear of losing jobs and access to medical care is settling in, we believe it reflects the actual changes in the medical situation rather than being caused by a selection bias. Notably, reported cohorts so far had comparable demographics and baseline characteristics, with the majority of respondents being female, having a higher educational level and income [9, 10].
Limitations of our study include the use of data supplied by patients. Using this approach, confirmation of medical data (e.g., histology, stage, treatment regimen) is not feasible. Furthermore, the questionnaire outside the COST data was not validated. There is also likely some selection bias among survey respondents—our population was predominantly female, highly educated and primarily US-based, and a relatively high proportion was treated at academic centers. But compared to previous surveys, in our patient cohort with more than 1500 responses, no differences in characteristics were seen (data submitted for publication). Perhaps most importantly, the data for COVID-19 are evolving extremely rapidly. The distribution of cases is changing, as is the approach to infection prevention, prophylaxis and treatment [1, 3, 13,14,15,16]. As such, it is possible that the perspective of patients and physicians will change as the situation progresses. To supplement this, we plan to continue to survey the RCC community to obtain the patient perspective on management.
Conclusion
Our data highlight severe financial impact of COVID-19 in patients with RCC. Acknowledging financial hardship and uncertainty related to future costs and providing thorough counseling of cancer patients should be part of the conversation during the pandemic. Younger patients, women and those with a lower income seem to be at highest need of financial advising. Treatment and surveillance of RCC patients might have to be adjusted to contemplate financial and medical needs.
References
Fauci AS, Lane HC, Redfield RR (2020) Covid-19 - navigating the uncharted. N Engl J Med 382:1268–1269
Pagano MB, Hess JR, Tsang HC et al (2020) Prepare to adapt: Blood supply and transfusion support during the first 2 weeks of the 2019 Novel Coronavirus (COVID-19) pandemic affecting Washington State. Transfusion 60:908–911
Ueda M, Martins R, Hendrie PC et al (2020) Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. https://doi.org/10.6004/jnccn.2020.7560
Yang G, Zhang H, Yang Y (2020) Challenges and countermeasures of integrative cancer therapy in the epidemic of COVID-19. Integr Cancer Ther 19:1534735420912811
Pisu M, Henrikson NB, Banegas MP, Yabroff KR (2018) Costs of cancer along the care continuum: what we can expect based on recent literature. Cancer 124:4181–4191
UNACD. The coronavirus shock: another story of a global crisis foretold and what policymaker should be doin about it. https://unctad.org/2020. Accessed 19 Apr 2020
Desai A, Gyawali B (2020) Financial toxicity of cancer treatment: moving the discussion from acknowledgement of the problem to identifying solutions. EClinicalMedicine 20:100269
de Souza JA, Yap BJ, Hlubocky FJ et al (2014) The development of a financial toxicity patient-reported outcome in cancer: the COST measure. Cancer 120:3245–3253
Zheng Z, Jemal A, Han X et al (2019) Medical financial hardship among cancer survivors in the United States. Cancer 125:1737–1747
de Souza JA, Yap BJ, Wroblewski K et al (2017) Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer 123:476–484
Bergerot CD, Battle D, Bergerot PG et al (2019) Sources of frustration among patients diagnosed with renal cell carcinoma. Front Oncol 9:11
Addario BJ, Fadich A, Fox J et al (2018) Patient value: perspectives from the advocacy community. Health Expect 21:57–63
Cao B, Wang Y, Wen D et al (2020) A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med 382:1787–1799
Parmet WE, Sinha MS (2020) Covid-19 - the law and limits of quarantine. N Engl J Med 382:e28
Choy KT, Wong AY, Kaewpreedee P et al (2020) Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral Res 178:104786
Costanzo M, De Giglio MAR, Roviello GN (2020) SARS CoV-2: Recent Reports on Antiviral Therapies Based on Lopinavir/Ritonavir, Darunavir/Umifenovir, Hydroxychloroquine, Remdesivir, Favipiravir and Other Drugs for the Treatment of the New Coronavirus. Curr Med Chem 27:4536–4541
Acknowledgements
The authors would like to thank all patients and their caregivers for their significant contributions in sharing their own experience over the cancer journey.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MDS, DJB, SKP, DFP: protocol/project development. MDS, DJB: data collection or management. MDS, CDB, SKP, DFP: data analysis. MDS, CDB, SKP, CDB, DFP: manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Ethics board approval was not obtained as these data were not obtained via an institution, but by a patient organization (KCCure).
Informed consent
All patients gave informed consent and voluntarily entered their data by themselves in the database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Staehler, M.D., Battle, D.J., Bergerot, C.D. et al. COVID-19 and financial toxicity in patients with renal cell carcinoma. World J Urol 39, 2559–2565 (2021). https://doi.org/10.1007/s00345-020-03476-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03476-6