Abstract
Backgrounds
Patient-reported outcome measurements are important for urinary incontinence. We analyze self-assessed patient satisfaction and define the clinical profile of patient with highest satisfaction with the adjustable transobturator male system (ATOMS).
Methods
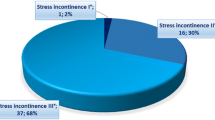
Patient perception of results was evaluated in a series of 181 patients after ATOMS adjustment. Baseline incontinence severity was defined in pads-per-day (PPD) as mild (2), moderate (3–5) or severe (≥ 6), and dryness as use of none or one security PPD. Post-operative pain at discharge was evaluated by 0–10 visual analogue scale and complications by Clavien–Dindo classification. Multivariate analysis was performed to anticipate “very much better” than baseline perception on patient global impression of improvement and a predictive nomogram was developed.
Results
Dryness was achieved in 80.7% (94.9% mild, 80.8% moderate and 65.8% severe groups). Mean pad-test and pad-count decrease with respect to baseline was 458 ± 330 ml and 3.2 ± 1.9 PPD, respectively (both p < .0001). Complications presented in 25 (13.8%). The proportion of patients that self-declared satisfied with the procedure was 87.1%; 90.6% perceived their situation “better” and 48.1% “very much better” than before. Multivariate analysis revealed best perception is defined by dryness after adjustment (p < .0001), baseline severity of incontinence (p = .007), low post-operative pain at discharge (p = .0018) and lack of complications (p = .007).
Conclusions
Self-assessed satisfaction with ATOMS is very high. Factors that predict best perception of improvement include dryness, baseline SUI severity, presence of complications and pain level during admission. Radiotherapy and device generation were not independent predictors. A nomogram to predict patients that are completely satisfied with ATOMS after adjustment is proposed.





Similar content being viewed by others
References
Radadia KD, Farber NJ, Shinder B, Polotti CF, Milas LJ, Tunuguntla HSGR (2018) Management of postradical prostatectomy urinary incontinence: a review. Urology 113:13–19
Nitti VW, Mourtzinos A, Brucker BM, SUFU Pad Test Study Group (2014) Correlation of patient perception of pad use with objective degree of incontinence measured by pad test in men with post-prostatectomy incontinence: the SUFU Pad Test Study. J Urol 192:836–842
Poon SA, Silberstein JL, Savage C, Maschino AC, Lowrance WT, Sandhu JS (2012) Surgical practice patterns for male urinary incontinence: analysis of case logs from certifying American urologists. J Urol 188:205–210
VanderAa F, Drake MJ, Kasyan GR, Petrolekas A, Cornu JN, Young Academic Urologists Functional Urology Group (2013) The artificial urinary sphincter after a quarter of a century: a critical systematic review of its use in male non-neurogenic incontinence. Eur Urol 63:681–689
Comiter CV, Dobberfuhl AD (2016) The artificial urinary sphincter and male sling for postprostatectomy incontinence: Which patient should get which procedure? Investig Clin Urol 57:3–13
Sahai A, Abrams P, Dmochowski R, Anding R (2017) The role of male slings in post prostatectomy incontinence: ICI-RS 2015. Neurourol Urodyn 36:927–934
Seweryn J, Bauer W, Ponholzer A, Schramek P (2012) Initial experience and results with a new adjustable transobturator male system for the treatment of stress urinary incontinence. J Urol 187:956–961
Mühlstädt S, Friedl A, Mohammed N, Schumann A, Weigand K, Kawan F, Göllert C, Kahlert C, Theil G, Fischer K, Fornara P (2017) Five-year experience with the adjustable transobturator male system for the treatment of male stress urinary incontinence: a single-center evaluation. World J Urol 35:145–151
Angulo JC, Arance I, Esquinas C, Dorado JF, Marcelino JP, Martins FE (2017) Outcome measures of adjustable transobturator male system with pre-attached scrotal port for male stress urinary incontinence after radical prostatectomy: a prospective study. Adv Ther 34:1173–1183
Angulo JC, Cruz F, Esquinas C, Arance I, Manso M, Rodríguez A, Pereira J, Ojea A, Carballo M, Rabassa M, Teyrouz A, Escribano G, Rodríguez E, Teba F, Celada G, Madurga B, Álvarez-Ossorio JL, Marcelino JP, Martins FE (2018) Treatment of male stress urinary incontinence with the adjustable transobturator male system: outcomes of a multi-center Iberian study. Neurourol Urodyn 37:1458–1466
Hoda MR, Primus G, Fischereder K, Von Heyden B, Mohammed N, Schmid N, Moll V, Hamza A, Karsch JJ, Brössner C, Fornara P, Bauer W (2013) Early results of a European multicentre experience with a new self-anchoring adjustable transobturator system for treatment of stress urinary incontinence in men. BJU Int 111:296–303
Herschorn S (2008) The artificial urinary sphincter is the treatment of choice for post-radical prostatectomy incontinence. Can Urol Assoc J 2:536–539
Kahlon B, Baverstock RJ, Carlson KV (2011) Quality of life and patient satisfaction after artificial urinary sphincter. Can Urol Assoc J 5:268–272
Fischer MC, Huckabay C, Nitti VW (2007) The male perineal sling: assessment and prediction of outcome. J Urol 177:1414–1418
Viers BR, Linder BJ, Rivera ME, Rangel LJ, Ziegelmann MJ, Elliott DS (2016) Long-term quality of life and functional outcomes among primary and secondary artificial urinary sphincter implantations in men with stress urinary incontinence. J Urol 196:838–843
Slevin ML, Plant H, Lynch D, Drinkwater J, Gregory WM (1988) Who should measure quality of life, the doctor or the patient? Br J Cancer 57:109–112
Corcos J, Beaulieu S, Donovan J, Naughton M, Gotoh M, Symptom Quality of Life Assesment Committee of the First International Consultation on Incontinence (2002) Quality of life assessment in men and women with urinary incontinence. J Urol 168:896–905
Twiss CO, Fischer MC, Nitti VW (2007) Comparison between reduction in 24-h pad weight, International Consultation on Incontinence-Short Form (ICIQ-SF) score, International Prostate Symptom Score (IPSS), and Post-Operative Patient Global Impression of Improvement (PGI-I) score in patient evaluation after male perineal sling. Neurourol Urodyn 26:8–13
Krause J, Tietze S, Behrendt W, Nast J, Hamza A (2014) Reconstructive surgery for male stress urinary incontinence: Experiences using the ATOMS(®) system at a single center. GMS Interdiscip Plast Reconstr Surg DGPW. https://doi.org/10.3205/iprs000056.eCollection
González SP, Cansino JR, Portilla MA, Rodriguez SC, Hidalgo L, De la Peña J (2014) First experience with the ATOMS(®) implant, a new treatment option for male urinary incontinence. Cent Eur J Urol 67:387–391
Friedl A, Mühlstädt S, Rom M, Kivaranovic D, Mohammed N, Fornara P, Brössner C (2016) Risk factors for treatment failure with the adjustable transobturator male system incontinence device: Who will succeed, who will fail? Results of a multicenter study. Urology 90:189–194
Friedl A, Mühlstädt S, Zachoval R, Giammò A, Kivaranovic D, Rom M, Fornara P, Brössner C (2017) Long-term outcome of the adjustable transobturator male system (ATOMS): results of a European multicentre study. BJU Int 119:785–792
Mühlstädt S, Friedl A, Zachoval R, Mohammed N, Schumann A, Theil G, Fornara P (2018) An overview of the ATOMS generations: port types, functionality and risk factors. World J Urol. https://doi.org/10.1007/s00345-018-2548-4
Chertack N, Gill BC, Angermeier KW, Montague DK, Wood HM (2017) Predicting success after artificial urinary sphincter: Which preoperative factors drive patient satisfaction postoperatively? Transl Androl Urol 6:1138–1143
Litwiller SE, Kim KB, Fone PD, White RW, Stone AR (1996) Post-prostatectomy incontinence and the artificial urinary sphincter: a long-term study of patient satisfaction and criteria for success. J Urol 156:1975–1980
Haab F, Trockman BA, Zimmern PE, Leach GE (1997) Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of followup. J Urol 158:435–439
Gousse AE, Madjar S, Lambert MM, Fishman IJ (2001) Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol 166:1755–1758
Montague DK, Angermeier KW, Paolone DR (2001) Long-term continence and patient satisfaction after artificial sphincter implantation for urinary incontinence after prostatectomy. J Urol 166:547–549
Roth CC, Winters JC (2006) Insertion of artificial urinary sphincter with preservation of bulbospongiosus muscle in patients at risk for sphincter erosion: an assessment of patient satisfaction. Ochsner J 6:54–58
Angulo JC, Esquinas C, Arance I, Rodríguez A, Pereira J, Rabassa M, Teyrouz A, Teba F, Celada G, Marcelino JP, Martins FE, Manso M, Cruz F (2018) Adjustable transobturator male system after failed surgical devices for male stress urinary incontinence: a feasibility study. Urol Int 101:106–113
Esquinas C, Angulo JC (2018) Effectiveness of adjustable transobturator male system (ATOMS) to treat male stress incontinence: a systematic review and meta-analysis. Adv Ther. https://doi.org/10.1007/s12325-018-0852-4
Acknowledgements
The authors acknowledge Mr. Juan Dorado (PerTICA S.L.) for statistical analysis.
Author information
Authors and Affiliations
Contributions
The contribution to each author is as follows: protocol/project development: JCA. Data collection or management: JCA, IA, AO, MC, AR, JP, MR, AT, GE, FT, BM, FEM, FC. Data analysis: JCA, IA, AO, MC, AR, JP, MR, AT, GE, FT, BM, FEM, FC. Manuscript writing/editing: JCA, FC.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest or specific disclosure regarding the publication of this article.
Ethical standards
The protocol was approved by local ethics committee in Hospital Universitario de Getafe (A08/17). All subject received informed consent to undergo surgery and all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Angulo, J.C., Arance, I., Ojea, A. et al. Patient satisfaction with adjustable transobturator male system in the Iberian multicenter study. World J Urol 37, 2189–2197 (2019). https://doi.org/10.1007/s00345-019-02639-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02639-4