Abstract
Objectives
To evaluate the role of shear-wave dispersion slope for predicting renal allograft dysfunction.
Methods
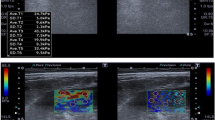
We retrospectively reviewed 128 kidney transplant recipients (median age, 55 years [interquartile range, 43–62 years]; male, 68) who underwent biopsy for allograft evaluation from November 2022 to February 2023. Cortex and renal sinus fat stiffness and shear-wave dispersion slope were obtained at shear-wave elastography (SWE). Cortex-to-sinus stiffness ratio (SR) and dispersion slope ratio (DSR)–related clinical and pathologic factors were evaluated using multivariable linear regression analysis. We conducted univariate and multivariate analyses for multiparametric ultrasound (US) parameters for identifying acute rejection and calculated the area under the receiver operating curve (AUC) values.
Results
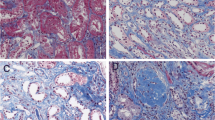
Of 128 patients, 31 (24.2%) demonstrated acute rejection. The SR value did not differ between patient groups (1.21 vs. 1.20, p = 0.47). Patients with acute rejection demonstrated a higher DSR than those without rejection (1.4 vs. 1.21, p < 0.01). Interstitial fibrosis and tubular atrophy grade (IFTA; coefficient, 0.11/grade; p = 0.04) and renal transplant and biopsy interval (coefficient, 0.00007/day; p = 0.03) were SR determinant factors, whereas only IFTA grade (coefficient, 0.10/grade; p = 0.01) for DSR. Multivariate analysis revealed mean resistive index (odds ratio [OR] 1.08, 95% confidence interval [CI] 1.02–1.14, p = 0.01) and DSR value (OR 16.0, 95% CI 3.0–85.8, p = 0.001) as independent factors for predicting acute rejection. An AUC of 0.74 for detecting acute rejection was achieved by combining the resistive index and DSR value.
Conclusion
Shear-wave dispersion slope obtained at SWE may help identify renal allograft dysfunction.
Clinical relevance statement
Acute rejection in renal allografts is a major cause of allograft failure, but noninvasive diagnosis is a challenge. Shear-wave dispersion slope can identify acute rejection non-invasively.
Key Points
• The interstitial fibrosis and tubular atrophy grade was a determinant factor for stiffness ratio and shear-wave dispersion slope ratio between cortex and renal sinus fat.
• Shear-wave dispersion slope ratio between cortex and renal sinus fat could identify acute rejection in renal allografts.
• A shear-wave dispersion slope has a potential to reduce unnecessary renal biopsy for evaluating renal allografts.




Similar content being viewed by others
Abbreviations
- ARFI:
-
Acoustic radiation force impulse
- AUC:
-
Area under the receiver operating characteristic curve
- DSR:
-
Cortex-to-renal sinus fat dispersion slope ratio
- IFTA:
-
Interstitial fibrosis and tubular atrophy
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RI:
-
Resistive index
- ROI:
-
Region of interest
- SR:
-
Cortex-to-renal sinus fat stiffness ratios
- SWE:
-
Shear-wave elastography
References
Sellarés J, de Freitas DG, Mengel M et al (2012) Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant 12:388–399. https://doi.org/10.1111/j.1600-6143.2011.03840.x
Yoo MG, Jung DC, Oh YT et al (2017) Usefulness of multiparametric ultrasound for evaluating structural abnormality of transplanted kidney: can we predict histologic abnormality on renal biopsy in advance? AJR Am J Roentgenol 209:W139–W144. https://doi.org/10.2214/AJR.16.17397
Schwarz A, Gwinner W, Hiss M et al (2005) Safety and adequacy of renal transplant protocol biopsies. Am J Transplant 5:1992–1996. https://doi.org/10.1111/j.1600-6143.2005.00988.x
Chen S, Urban MW, Pislaru C, et al (2009) Liver elasticity and viscosity quantification using shearwave dispersion ultrasound vibrometry (SDUV). In: 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society. pp 2252–2255
Sugimoto K, Moriyasu F, Oshiro H et al (2018) Viscoelasticity measurement in rat livers using shear-wave US elastography. Ultrasound Med Biol 44:2018–2024. https://doi.org/10.1016/j.ultrasmedbio.2018.05.008
Sugimoto K, Moriyasu F, Oshiro H, et al (2020) Clinical utilization of shear wave dispersion imaging in diffuse liver disease. Ultrasonography 39:3–10. https://doi.org/10.14366/usg.19031
Lee DH, Lee JY, Bae JS et al (2019) Shear-wave dispersion slope from US shear-wave elastography: detection of allograft damage after liver transplantation. Radiology 293:327–333. https://doi.org/10.1148/radiol.2019190064
Jeong HJ (2020) Diagnosis of renal transplant rejection: Banff classification and beyond. Kidney Res Clin Pract 39:17–31. https://doi.org/10.23876/j.krcp.20.003
Barr RG, Wilson SR, Rubens D et al (2020) Update to the Society of Radiologists in Ultrasound Liver elastography consensus statement. Radiology 296:263–274. https://doi.org/10.1148/radiol.2020192437
Gennisson J-L, Grenier N, Combe C, Tanter M (2012) Supersonic shear wave elastography of in vivo pig kidney: influence of blood pressure, urinary pressure and tissue anisotropy. Ultrasound Med Biol 38:1559–1567. https://doi.org/10.1016/j.ultrasmedbio.2012.04.013
Shiina T, Nightingale KR, Palmeri ML et al (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: part 1: basic principles and terminology. Ultrasound Med Biol 41:1126–1147. https://doi.org/10.1016/j.ultrasmedbio.2015.03.009
Dietrich CF, Bamber J, Berzigotti A et al (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (long version). Ultraschall Med 38:e16–e47. https://doi.org/10.1055/s-0043-103952
Tublin ME, Bude RO, Platt JF (2003) The resistive index in renal Doppler sonography: where do we stand? AJR Am J Roentgenol 180:885–892. https://doi.org/10.2214/ajr.180.4.1800885
Syversveen T, Brabrand K, Midtvedt K et al (2011) Assessment of renal allograft fibrosis by acoustic radiation force impulse quantification – a pilot study. Transpl Int 24:100–105. https://doi.org/10.1111/j.1432-2277.2010.01165.x
Iyama T, Sugihara T, Takata T, Isomoto H (2021) Renal ultrasound elastography: a review of the previous reports on chronic kidney diseases. Appl Sci 11:9677. https://doi.org/10.3390/app11209677
Amador C, Urban MW, Chen S, Greenleaf JF (2011) Shearwave dispersion ultrasound vibrometry (SDUV) on swine kidney. IEEE Trans Ultrason Ferroelectr Freq Control 58:2608–2619. https://doi.org/10.1109/TUFFC.2011.2124
Selzo MR, Moore CJ, Hossain MdM et al (2016) On the quantitative potential of viscoelastic response (VisR) ultrasound using the one-dimensional mass-spring-damper model. IEEE Trans Ultrason Ferroelectr Freq Control 63:1276–1287. https://doi.org/10.1109/TUFFC.2016.2539323
Zhao X, Pelegri AA (2014) Modeling dynamic responses of viscoelastic heterogeneous soft tissues to step acoustic radiation force. In: Proceedings of the ASME 2013 International Mechanical Engineering Congress and Exposition, vol 3B: Biomedical and Biotechnology Engineering. V03BT03A061. https://doi.org/10.1115/IMECE2013-66109
Hossain MM, Selzo MR, Hinson RM et al (2018) Evaluating renal transplant status using viscoelastic response (VisR) ultrasound. Ultrasound Med Biol 44:1573–1584. https://doi.org/10.1016/j.ultrasmedbio.2018.03.016
Lee ES, Lee JB, Park HR et al (2017) Shear wave liver elastography with a propagation map: diagnostic performance and inter-observer correlation for hepatic fibrosis in chronic hepatitis. Ultrasound Med Biol 43:1355–1363. https://doi.org/10.1016/j.ultrasmedbio.2017.02.010
Roufosse C, Simmonds N, Clahsen-van Groningen M et al (2018) A 2018 reference guide to the Banff classification of renal allograft pathology. Transplantation 102:1795. https://doi.org/10.1097/TP.0000000000002366
Hwang J, Kim HW, Kim PH et al (2021) Technical performance of acoustic radiation force impulse imaging for measuring renal parenchymal stiffness: a systematic review and meta-analysis. J Ultrasound Med 40:2639–2653. https://doi.org/10.1002/jum.15654
Maralescu F-M, Chiodan M, Sircuta A et al (2022) Are the currently available elastography methods useful in the assessment of chronic kidney disease? A systematic review and a meta-analysis. Appl Sci 12:2359. https://doi.org/10.3390/app12052359
Stock KF, Klein BS, Vo Cong MT et al (2010) ARFI-based tissue elasticity quantification in comparison to histology for the diagnosis of renal transplant fibrosis. Clin Hemorheol Microcirc 46:139–148. https://doi.org/10.3233/CH-2010-1340
Makita A, Nagao T, Miyoshi K-I et al (2021) The association between renal elasticity evaluated by real-time tissue elastography and renal fibrosis. Clin Exp Nephrol 25:981–987. https://doi.org/10.1007/s10157-021-02063-2
Wang L, Xia P, Lv K et al (2014) Assessment of renal tissue elasticity by acoustic radiation force impulse quantification with histopathological correlation: preliminary experience in chronic kidney disease. Eur Radiol 24:1694–1699. https://doi.org/10.1007/s00330-014-3162-5
Ries M, Jones RA, Basseau F et al (2001) Diffusion tensor MRI of the human kidney. J Magn Reson Imaging 14:42–49. https://doi.org/10.1002/jmri.1149
Ghonge NP, Mohan M, Kashyap V, Jasuja S (2018) Renal allograft dysfunction: evaluation with shear-wave sonoelastography. Radiology 288:146–152. https://doi.org/10.1148/radiol.2018170577
Maralescu F-M, Bende F, Sporea I et al (2022) Assessment of renal allograft stiffness and viscosity using 2D SWE PLUS and Vi PLUS measures—a pilot study. J Clin Med 11:4370. https://doi.org/10.3390/jcm11154370
Grenier N, Poulain S, Lepreux S et al (2012) Quantitative elastography of renal transplants using supersonic shear imaging: a pilot study. Eur Radiol 22:2138–2146. https://doi.org/10.1007/s00330-012-2471-9
Boor P, Floege J (2015) Renal allograft fibrosis: biology and therapeutic targets. Am J Transplant 15:863–886. https://doi.org/10.1111/ajt.13180
Asano K, Ogata A, Tanaka K et al (2014) Acoustic radiation force impulse elastography of the kidneys. J Ultrasound Med 33:793–801. https://doi.org/10.7863/ultra.33.5.793
Bob F, Bota S, Sporea I et al (2015) Relationship between the estimated glomerular filtration rate and kidney shear wave speed values assessed by acoustic radiation force impulse elastography. J Ultrasound Med 34:649–654. https://doi.org/10.7863/ultra.34.4.649
Maralescu F-M, Vaduva A, Schiller A et al (2023) Relationship between novel elastography techniques and renal fibrosis—preliminary experience in patients with chronic glomerulonephritis. Biomedicines 11:365. https://doi.org/10.3390/biomedicines11020365
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sang Youn Kim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB no. 2306-218-1446).
Study subjects or cohorts overlap
None.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Taek Min Kim and Hyungwoo Ahn contributed equally as first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, T.M., Ahn, H., Cho, J.Y. et al. Prediction of acute rejection in renal allografts using shear-wave dispersion slope. Eur Radiol (2023). https://doi.org/10.1007/s00330-023-10492-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-023-10492-8