Abstract
Objectives
The common practice is to remove symptomatic common bile duct (CBD) stones in patients. This study aimed to investigate the factors affecting the percutaneous transhepatic removal of CBD stones.
Methods
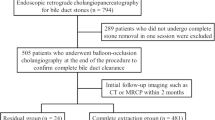
We retrospectively analyzed the data of 100 patients (66 men and 34 women; age: 25–105 years, mean 79.1 years) with symptomatic CBD stones who underwent percutaneous transhepatic stone removal (PTSR) from January 2010 through October 2019. After balloon dilation of the ampulla of Vater or bilioenteric anastomosis, the stones were pushed out of the CBD into the small bowel with a balloon catheter. If failed, basket lithotripsy was performed. Technical success was defined as complete clearance of the bile ducts on a cholangiogram.
Results
The technical success rate was 83%, and achieved 90.2% in patients with altered gastroduodenal/pancreatobiliary anatomy. Multivariable analysis revealed that CBD diameter (odds ratio [OR]: 506.460, p = 0.015), failed ERCP (OR: 16.509, p = 0.004), Tokyo guidelines TG18/TG13 severity (grade III; OR: 60.467, p = 0.006), and left-sided transhepatic approach (OR: 21.621, p = 0.012) were risk factors for technical failure. The appropriate cutoff CBD size was 15.5 mm (area under the curve: 0.91). CBD stone size, radiopacity of stones, and CBD angle between retroduodenal and pancreatic portion did not influence technical success.
Conclusions
PTSR is effective for CBD stone removal in older adults and individuals with altered gastrointestinal tract anatomy. The aforementioned risk factors for technical failure should be considered in preoperative evaluation before PTSR to improve the success rate.
Key Points
• PTSR is effective in symptomatic CBD stone management among older adults and individuals with altered anatomy. Investigating clinical /anatomic factors can guide radiologists toward a more comprehensive preoperative evaluation to maximize the success rate.
• Our data indicate that dilated CBD (diameter ≥ 15.5 mm) and left-sided PTBDs reduce the technical success rate by 506-fold and 22-fold, respectively.
• Clinical factors such as previous failed ERCP for stone removal and higher severity of acute cholangitis lessen the technical success rate.




Similar content being viewed by others
Abbreviations
- aCBD:
-
CBD angulation between retroduodenal and pancreatic portion
- ALKP:
-
Alkaline phosphatase
- AUC:
-
Area under the curve
- CBD:
-
Common bile duct
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- ESCP:
-
Endosonography-guided cholangiopancreatography
- ESWL:
-
Extracorporeal shock-wave lithotripsy
- fERCP:
-
Previous ERCP failure for stone removal
- HU:
-
Hounsfield unit
- IHD:
-
Intrahepatic bile duct
- MRCP:
-
Magnetic resonance cholangiopancreatography
- OR:
-
Odds ratio
- PAD:
-
Periampullary diverticulum
- PTBD:
-
Percutaneous transhepatic biliary drainage
- PTSR:
-
Percutaneous transhepatic biliary stone removal
- T.bil:
-
Total bilirubin
- TG18/TG 13:
-
Tokyo guideline 2018/2013 for acute cholangitis severity
References
Shah KN, Clary BM (2017) Chapter 36A - stones in the bile duct: clinical features and open surgical approaches and techniques. In: Jarnagin WR (ed) Blumgart’s Surgery of the Liver, Biliary Tract and Pancreas, 2-Volume Set, 6th edn. Elsevier, Philadelphia, pp 585-603.e3
Manes G, Paspatis G, Aabakken L et al (2019) Endoscopic management of common bile duct stones. Eur Soc Gastrointest Endosc (ESGE) Guide Endosc 51(5):472–491
Li G, Pang Q, Zhai H et al (2021) SpyGlass-guided laser lithotripsy versus laparoscopic common bile duct exploration for large common bile duct stones: a non-inferiority trial. Surg Endosc 35(7):3723–3731
Costi R, Gnocchi A, Di Mario F, Sarli L (2014) Diagnosis and management of choledocholithiasis in the golden age of imaging, endoscopy and laparoscopy. World J Gastroenterol 20(37):13382–401
Morrell D, Pauli E, Juza R (2019) Endoscopy in surgically altered anatomy. Annals Laparosc Endoscopic Surg 4(41)
Ali MF, Modayil R, Gurram KC, Brathwaite CEM, Friedel D, Stavropoulos SN (2018) Spiral enteroscopy-assisted ERCP in bariatric-length Roux-en-Y anatomy: a large single-center series and review of the literature (with video). Gastrointest Endosc 87(5):1241–1247
Committee AT, Chauhan SS, Manfredi MA et al (2015) Enterosc Gastrointest Endosc 82(6):975–990
Jirapinyo P, Lee LS (2016) Endoscopic ultrasound-guided pancreatobiliary endoscopy in surgically altered anatomy. Clin Endosc 49(6):515–529
Martin A, Kistler CA, Wrobel P, Yang JF, Siddiqui AA (2016) Endoscopic ultrasound-guided pancreaticobiliary intervention in patients with surgically altered anatomy and inaccessible papillae: a review of current literature Endosc. Ultrasound 5(3):149–156
Koggel LM, Wahab PJ, Robijn RJ et al (2021) Efficacy and safety of 100 laparoscopy-assisted transgastric endoscopic retrograde cholangiopancreatography procedures in patients with Roux-en-Y gastric bypass. Obes Surg 31(3):987–993
Saleem A, Levy MJ, Petersen BT, Que FG, Baron TH (2012) Laparoscopic assisted ERCP in Roux-en-Y gastric bypass (RYGB) surgery patients. J Gastrointest Surg 16(1):203–8
Lopes TL, Clements RH, Wilcox CM (2009) Laparoscopy-assisted ERCP: experience of a high-volume bariatric surgery center (with video). Gastrointest Endosc 70(6):1254–9
Lezoche E, Paganini AM (2000) Technical considerations and laparoscopic bile duct exploration: transcystic and choledochotomy. Semin Laparosc Surg 7(4):262–278
Shojaiefard A, Esmaeilzadeh M, Ghafouri A, Mehrabi A (2009) Various techniques for the surgical treatment of common bile duct stones: a meta review. Gastroenterol Res Pract 2009:840208
Sharma A, Dahiya P, Khullar R, Soni V, Baijal M, Chowbey PK (2012) Management of common bile duct stones in the laparoscopic era. Indian J Surg 74(3):264–269
Hongjun H, Yong J, Baoqiang W (2015) Laparoscopic common bile duct exploration: choledochotomy versus transcystic approach? Surg Laparosc Endosc Percutan Tech 25(3):218–222
Perez MR, Oleaga JA, Freiman DB, McLean GL, Ring EJ (1979) Removal of a distal common bile duct stone through percutaneous transhepatic catheterization. Arch Surg 114(1):107–109
Clouse ME (1983) Dormia basket modification for percutaneous transhepatic common bile duct stone removal. AJR Am J Roentgenol 140(2):395–397
Clouse ME, Falchuk KR (1983) Percutaneous transhepatic removal of common duct stones: report of ten patients. Gastroenterology 85(4):815–819
Centola CA, Jander HP, Stauffer A, Russinovich NA (1981) Balloon dilatation of the papilla of Vater to allow biliary stone passage. AJR Am J Roentgenol 136(3):613–614
Ozcan N, Kahriman G, Mavili E (2012) Percutaneous transhepatic removal of bile duct stones: results of 261 patients. Cardiovasc Intervent Radiol 35(3):621–7
Liu B, Ma J, Li S, et al (2021) Percutaneous transhepatic papillary balloon dilation versus endoscopic retrograde cholangiopancreatography for common bile duct stones: a multicenter prospective study. Radiology 300(2):470–478
Muglia R, Lanza E, Poretti D et al (2020) Percutaneous transhepatic endoscopic lithotripsy of biliary stones with holmium laser for the treatment of recurrent cholangitis. Abdom Radiol (NY) 45(8):2561–2568
Tripathi N, Mardini H, Koirala N, Raissi D, Emhmed Ali SM, Frandah WM (2020) Assessing the utility, findings, and outcomes of percutaneous transhepatic cholangioscopy with spyglass(TM) direct visualization system: a case series. Transl Gastroenterol Hepatol 5:12
Zhuo H, Chen Z, Lin R, et al (2020) Percutaneous transhepatic choledochoscopic lithotomy (PTCSL) is effective for the treatment of intrahepatic and extrahepatic choledocholithiasis. Surg Laparosc Endosc Percutan Tech 31(3):326–330
Wang P, Tao H, Liu C et al (2021) One-step percutaneous transhepatic cholangioscopic lithotripsy in patients with choledocholithiasis. Clin Res Hepatol Gastroenterol 45(2):101477
Jung GS, Kim YJ, Yun JH et al (2019) Percutaneous transcholecystic removal of common bile duct stones: case series in 114 patients. Radiology 290(1):238–243
Deal AK, Murthy S, Wason S, Vingan H, Fabrizio M (2016) Percutaneous transhepatic holmium laser lithotripsy of a large common bile duct stone. Radiol Case Rep 11(4):361–364
Herr A, Collins D, White M et al (2019) Percutaneous biliary endoscopy for stones. Tech Vasc Interv Radiol 22(3):127–134
Lamanna A, Maingard J, Bates D, Ranatunga D, Goodwin M (2019) Percutaneous transhepatic laser lithotripsy for intrahepatic cholelithiasis: a technical report. J Med Imaging Radiat Oncol 63(6):758–764
Tao H, Wang P, Sun B, Li K, Zhu C (2020) One-step multichannel percutaneous transhepatic cholangioscopic lithotripsy applied in bilateral hepatolithiasis. World J Surg 44(5):1586–1594
Gerges C, Vazquez AG, Tringali A, et al (2021) Percutaneous transhepatic cholangioscopy using a single-operator cholangioscope (pSOC), a retrospective, observational, multicenter study. Surg Endosc 35(12):6724–6730
Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS (1993) Endoscopic extraction of bile duct stones: management related to stone size. Gut 34(12):1718–1721
Kiriyama S, Kozaka K, Takada T et al (2018) Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci 25(1):17–30
Skandalakis JE, Gray SW, Rowe JS (1983) Anatomical complications in general surgery 1st ed., McGraw-Hill. Book company. New York paris 130
Patel IJ, Rahim S, Davidson JC et al (2019) Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part II: Recommendations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol 30(8):1168-1184 e1
Cotton PB, Eisen GM, Aabakken L et al (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Banks PA, Bollen TL, Dervenis C et al (2013) Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 62(1):102–11
Kim CW, Chang JH, Lim YS, Kim TH, Lee IS, Han SW (2013) Common bile duct stones on multidetector computed tomography: attenuation patterns and detectability. World J Gastroenterol 19(11):1788–1796
Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y (1974) Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc 20(4):148–151
Hallerback B, Enochsson L (2020) A prospective nationwide study on the impact of the level of sedation on cannulation success and complications of endoscopic retrograde cholangiopancreatography. Ann Gastroenterol 33(3):299–304
Simsek O, Simsek A, Ergun S, Velidedeoglu M, Saribeyoglu K, Pekmezci S (2017) Managing endoscopic retrograde cholangiopancreatography-related complications in patients referred to the surgical emergency unit. Ulus Travma Acil Cerrahi Derg 23(5):395–399
Neoptolemos JP, Carr-Locke DL, Fraser I, Fossard DP (1984) The management of common bile duct calculi by endoscopic sphincterotomy in patients with gallbladders in situ. Br J Surg 71(1):69–71
Dumonceau JM, Kapral C, Aabakken L et al (2020) ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 52(2):127–149
Plewka M, Rysz J, Kujawski K (2017) Complications of endoscopic retrograde cholangiopancreatography. Pol Merkur Lekarski 43(258):272–275
Karaahmet F, Kekilli M (2018) The presence of periampullary diverticulum increased the complications of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol 30(9):1009–1012
Grimes KL, Maciel VH, Mata W, Arevalo G, Singh K, Arregui ME (2015) Complications of laparoscopic transgastric ERCP in patients with Roux-en-Y gastric bypass. Surg Endosc 29(7):1753–1759
Hu Y, Kou DQ, Guo SB (2020) The influence of periampullary diverticula on ERCP for treatment of common bile duct stones. Sci Rep 10(1):11477
Kim HJ, Choi HS, Park JH et al (2007) Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc 66(6):1154–1160
Acknowledgements
Kan Ling contributed to the figure illustration (Fig. 4).
Funding
This study has received funding by Wong Vung-Hau Radiology Foundation (WVH). The WVH Foundation had no role in the design, analysis or interpretation of the results in this study, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Chien-An Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• prognostic study/observational
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chiu, HC., Liu, CA., Tseng, HS. et al. Predictors of technical success of percutaneous transhepatic common bile duct stone removal: is it only a matter of stone size?. Eur Radiol 33, 6872–6882 (2023). https://doi.org/10.1007/s00330-023-09631-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09631-y