Abstract
Objectives
We explored the prevalence of health complaints subjectively associated with static magnetic field (SMF) and acoustic noise exposure among MR radiographers in Sweden, using CT radiographers as a control group. Additionally, we explored radiographers’ use of strategies to mitigate adverse health effects.
Methods
A cross-sectional survey was sent to all hospitals with MR units in Sweden. MR and/or CT personnel reported prevalence and attribution of symptoms (vertigo/dizziness, nausea, metallic taste, illusion of movement, ringing sensations/tinnitus, headache, unusual drowsiness/tiredness, forgetfulness, difficulties concentrating, and difficulties sleeping) within the last year. We used logistic regression to test associations between sex, age, stress, SMF strength, working hours, and symptom prevalence. Data regarding hearing function, work-environmental noise, and strategies to mitigate adverse symptoms were also analysed.
Results
In total, 529 out of 546 respondents from 86 hospitals were eligible for participation. A ≥ 20 working hours/week/modality cut-off rendered 342 participants grouped into CT (n = 75), MR (n = 121), or mixed personnel (n = 146). No significant differences in symptom prevalence were seen between groups. Working at ≥ 3T increased SMF-associated symptoms as compared with working at ≤ 1.5T (OR: 2.03, CI95: 1.05–3.93). Stress was a significant confounder. Work-related noise was rated as more troublesome by CT than MR personnel (p < 0.01). MR personnel tended to use more strategies to mitigate adverse symptoms.
Conclusion
No significant differences in symptom prevalence were seen between MR and CT radiographers. However, working at 3T increased the risk of SMF symptoms, and stress increased adverse health effects. Noise nuisance was considered more problematic by CT than MR personnel.
Key Points
• No significant differences in symptom prevalence were seen between MR and CT radiographers.
• Working at ≥ 3 T doubled the odds of experiencing SMF symptoms (vertigo/dizziness, nausea, metallic taste, and/or illusion of movement) as compared to working exclusively at ≤ 1.5 T.
• Work-related acoustic noise was less well mitigated and was rated as more troublesome by CT personnel than by MR personnel.
Similar content being viewed by others
Introduction
Working with MRI entails static magnetic field (SMF) exposures that are thousands of times stronger than the Earth’s magnetic field. The exposure is expressed as magnetic flux density measured in Tesla (T), and clinical field strengths commonly range from 1 to 7 T [1, 2]. Any physical movement inside the SMF creates motion-induced time-varying magnetic fields in the body, which induce electrical currents that can stimulate sensory organs [3, 4]. MR personnel, e.g., radiographers, move inside the SMF as an integrated part of their work: setting up equipment, assisting and positioning patients, and cleaning between exams. In some instances, MR personnel might be needed inside the room during scanning for patient support. Furthermore, switched gradient magnetic fields are applied during scanning which produce acoustic noise between 80 and 130 decibels (dB) [5, 6]—sound pressure levels that can cause discomfort and hearing injuries (≥ 85 dB) [5, 7].
Exposure to any one of the above sources is a potential health hazard. MR personnel report transient symptoms such as vertigo, tiredness, metallic taste, headache, nystagmus, head ringing, and nausea [3, 8, 9]. Some workers also experience visual light flashes (magnetophosphenes) and have difficulties concentrating [10,11,12]. Many of the transient symptoms are linked to SMF exposure [13], particularly during movement of the head. Recent evidence suggests that the magnetic fields induce electric fields, which affect the vestibular system and initiate vertigo [14, 15], especially at stronger SMFs, e.g., 7 T [16, 17].
To mitigate adverse health effects from SMF exposure, occupational exposure limits are set by the International Commission on Non-Ionizing Radiation Protection (ICNIRP) [18]. These limits form a basis for national legislation—for instance, AFS 2016:3 [19] in Sweden. Moreover, personnel are recommended to use hearing protection inside the MR room during scanning [7, 20], and to move slowly close to the MR bore to limit motion-induced symptoms [11, 21].
The discussion about safety in MR environments intensified after the first draft of the EU directive 2013/35/EU [22] was published in 2009. At the same time, a Swedish pilot study among MR personnel found that 47% reported symptoms such as dizziness, illusion of movement, and headaches regularly, and 15% experienced symptoms in connection to their routine work close to the scanner [8]. However, a limitation in that and similar studies [13, 23] was the lack of control groups to account for environmental confounders. To limit adverse health effects, we must better understand the factors in the working environment that contribute to causing harm [4]. We propose to adjust for work-related confounders by comparing health effects among MR personnel with a similar group working without exposure to strong SMFs—i.e., CT personnel. Incidentally, established work environmental risk exposures among CT personnel outside of ionizing radiation are limited; however, stress and burnout appear to be increasing among CT radiographers due to increased workload [24].
Our primary aim was to explore the prevalence of health complaints subjectively associated with static magnetic field and acoustic noise exposure among MR radiographers in Sweden, using CT radiographers as a control group. Our main hypothesis was that MR radiographers reported more symptoms in general compared to CT radiographers. Additionally, we explored the attribution of symptoms in relation to modalities and whether personnel use strategies to mitigate adverse health effects.
Material and methods
Data to assess health complaints were extracted from a cross-sectional national survey with 202 items that had been sent electronically to the 92 known hospitals with MR units in Sweden. At each hospital, a contact person responsible for MRI and/or CT was asked to inform their colleagues and distribute a link to the web-based questionnaire. Data from the same questionnaire, focusing on MR incidents, have earlier been published and we refer to this publication for further information on data collection procedures [25]. In summary, all personnel working to any degree with MRI and/or CT scanning—thus, primarily targeting radiographers—were considered eligible for participation. At the time, the number of personnel working with human scanning within the 92 hospitals was estimated to be 620 for MR and approximately 1300 for CT [25]. Data were collected between September 2015 and April 2016, during which time three survey reminders were sent to increase the response rate.
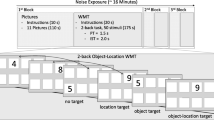
The included items were based on similar validated questionnaires concerning work environmental health, e.g., the widely used MM-questionnaires, and The Occupational Stress Questionnaire [26, 27]. Specifically, participants were asked to rate the prevalence of symptoms subjectively associated with SMF and acoustic noise exposure: vertigo/dizziness, nausea, metallic taste, illusion of movement, ringing sensation or sound (tinnitus), headache, unusual drowsiness or tiredness, forgetfulness, difficulties concentrating, and difficulties sleeping. We asked for symptom prevalence in general during the last year, e.g., without taking their work with MR or CT into account. Prevalence ranged on a five-point Likert scale from “never” to “more than four times a week”. This was followed by questions about whether symptoms occurred or intensified when being in the MR and/or CT scanner room, and if so, in relation to where in the room and doing what type of movements, if any. These items had previously been tested among MR nurses in a pilot study [8]. Besides demographic data, participants were also asked about work-environmental noise, self-rated hearing function, and if they used any strategies to mitigate adverse health effects in their work.
First, we included all eligible participants and used their amount of weekly MR working hours as an independent variable to predict symptom prevalence. Second, we categorized participants into three separate groups: MR personnel, CT personnel, and mixed (both MR and CT) personnel. To meet group inclusion, we added a cut-off value a priori of 20 work hours/week (h/w), i.e., ≥ 50% of full-time work in Sweden, within the respective image modalities. Personnel who worked ≥ 20 h/w with MR, and did not work with CT at all, were categorized into the MR group. Personnel who worked ≥ 20 h/w with CT, and not with MR at all, were categorized into the CT group. The mixed group consisted of participants who worked both with CT and MR for at least 20 h/w combined. Third, we divided all MR users from MR personnel and mixed personnel into those whose work included MR systems > 1.5 T and those working only at ≤ 1.5 T.
All symptom prevalence variables were a priori dichotomized into never/seldom (< 1 time/week) or often (≥ 1 time(s)/week), as previously done by Wilén and de Vocht [8]. The symptoms were also categorized into three groups in relation to SMF (vertigo/dizziness, illusion of movement, metallic taste, and nausea), general work environment (difficulties concentrating, difficulties sleeping, forgetfulness, headache, and unusual drowsiness or tiredness), and acoustic noise (ringing sensations or sound/tinnitus). The variable “are you experiencing acoustic noise in your work in general as troublesome?” was dichotomized into little (“not at all” or “somewhat”) or a great deal. Additionally, the following variables were dichotomized: sex; established hearing loss (yes/no), and self-rated hearing function (normal/impaired).
We used descriptive statistics to survey symptom prevalence and display participant characteristics. When appropriate, we used the Chi-square tests to compare categorical data between the three groups. Logistic regression was used to test the association between MR work exposure (h/w) and symptom prevalence, which included all eligible participants. Moreover, we tested the association between symptom prevalence and MR, CT, and mixed personnel. Symptoms were both tested individually and within the three symptom groups as dependent variables in separate logistic regression models. Lastly, MR users within the MR and mixed personnel were analyzed to evaluate whether SMF strength affected the prevalence of the three symptom groups. In all logistic regression models, adjustment variables were age, sex, and stress level. Each independent variable was initially tested using univariate logistic regression. Any variable with a p value < 0.2 was included in a multivariate regression model to adjust for confounders. Missing data in any of the logistic regression variables were excluded from that model.
All data analyses were carried out in SPSS version 26 (IBM Corp.). In all tests, a p value ≤ 0.05 was considered statistically significant.
Results
Participants
Our survey was answered by 546 participants from 86 hospitals. After we excluded incomplete submissions and subjects who neither worked with MR, CT, nor human scanning, 529 participants were eligible, among which 345 worked with MR, and 392 worked with CT. Adding the cut-off value of 20 work h/w within the image modalities rendered 342 participants for group inclusion. Among these, 121 participants worked ≥ 50% with MR but not CT (78% female; mean age ± SD: 52 ± 8.9 years, range 30–66), 75 participants worked ≥ 50% with CT but not MR (84 % female; mean age ± SD: 43 ± 13 years, range 23–65), and 146 participants worked ≥ 50% with both MR and CT combined (71% female; mean age ± SD 42 ± 12 years, range 24–65). Except for two biomedical scientists, one registered nurse, and one physicist, all participants were radiographers. Demographic data are presented in Table 1. Altogether, 267 (121 + 146) MR personnel were included in the cut-off stratification.
Health complaints
Reported symptom prevalence (n = 342 participants) did not differ significantly between the MR, CT, and mixed groups (all p > 0.05) (Table 2). Among participants in the MR and mixed group (n = 267), however, working with ≥ 3 T doubled the odds of experiencing SMF symptoms ≥ 1 time(s)/week (odds ratio, OR: 2.03; CI95: 1.05–3.93, p = 0.04).
The CT group showed 2.6 times greater odds of experiencing acoustic noise at work in general as troublesome to “a great deal” than the MR group (p < 0.01) (Fig. 1). Occasional ringing sounds were reported to occur when inside the CT room or standing next to the gantry (Tables 3 and 4). However, no differences were seen in self-rated hearing function (p = 0.54) or established hearing loss (p = 0.79) between CT, MR, or mixed personnel (Table 5).
Odds ratios of experiencing acoustic noise at work in general as troublesome to “a great deal” (n = 342). We dichotomized the outcome of “are you experiencing acoustic noise at work in general as troublesome?” into 0 = “not at all” or “somewhat”, and 1 = “a great deal”, and performed logistic regression adjusted for sex, age, and stress (ascending order). To simplify the model, we excluded all variables with a p value > 0.2. Female sex, and group (MR), were the reference categories. Plots denote the odds ratio, OR, and the black whiskers mark the 95% confidence interval (CI)
The amount of weekly MR working hours (n = 529 participants) had no significant association with symptom prevalence among the SMF, general work environment, or acoustic noise symptom groups (all p > 0.05, data not shown). Instead, stress was revealed as a significant confounder to all symptom variables individually (all p < 0.05) except for metallic taste (p = 0.18), and within the three larger symptom groups (SMF, p < 0.001; general work environment, p < 0.001; and acoustic noise, p < 0.001). Additionally, for each year of age, the odds of experiencing ringing sensations or sound (tinnitus) one or more times a week increased by 3% (OR: 1.03; CI95: 1.00–1.06, p = 0.03). For unusual drowsiness, each year of life decreased the odds by 2.8% (OR: 0.97; CI95: 0.95–0.99, p = 0.01). Female sex increased the odds of headache 3.5-fold (OR: 3.47; CI95: 1.32–9.08, p = 0.01), while each year of life decreased odds of headache by 3.7% (OR 0.96; CI95: 0.94–0.99, p < 0.01). For sleeping difficulties, each year of life increased the odds by 3.1% (OR 1.03; CI95: 1.01–1.05, p < 0.01).
When looking exploratory at symptom occurrence (Table 3) and attribution (Table 4) in relation to being in the MR or CT room, vertigo was reported to occur “sometimes” by 49% in the MR group, and movement close to the MR gantry was the largest trigger (Table 3). In comparison, 16% of the CT group reported vertigo “sometimes” inside the CT room, most commonly when making sudden movements. Furthermore, MR personnel reported nausea, illusion of movement, and metallic taste to mostly occur when being close to, or leaning towards, the MR gantry (Table 4). Difficulties concentrating were reported to occur “sometimes” by 25% of CT personnel as compared to 14% by MR personnel (Table 3). However, we found no significant differences in general work environment symptoms between the MR, CT, and mixed groups (all p > 0.05) (Table 2).
Considering the use of strategies to mitigate adverse symptoms during work (Fig. 2), 54% and 45% among MR and CT personnel, respectively, reported no use of strategies. However, personnel in the MR group and the mixed group reported that they slowed down their movements in the MR scanner room (4.8–7.4%) and avoided working within proximity to the scanner gantry (16–18%), compared to the CT working personnel (0–2.7%). Regarding the use of hearing protection, 66–68% of the MR group and mixed group always used it inside the MR room during scanning, whereas 69–84% of the mixed group and CT group never used hearing protection inside the CT room during scanning (Table 5). Incidentally, two CT radiographers stated in an open question that they often closed the scanner room door to suppress acoustic noise even if no patient was examined.
Discussion
The prevalence of reported adverse symptoms subjectively associated with SMF and acoustic noise exposure did not significantly differ between MR and CT radiographers. However, exposure to higher SMFs (3 T) increased MR radiographers’ odds of experiencing SMF related symptoms. Further, stress appears to have stronger associations with symptom prevalence than working with MRI.
Although this study partly corroborates previous literature [3, 8, 13, 23, 28,29,30], our data show no significant association between SMF symptoms and the amount of weekly MR working hours. In contrast, de Vocht et al [13] did see a positive association between weekly MR working hours and increased reporting of SMF symptoms; however, their data failed to associate subjective symptoms with magnetic field exposure or magnetic field strength (1.5 T and 3 T). In comparison, Schaap et al [3] found a positive association between increased SMF symptoms and increased field strength in closed-bore MR systems. Unlike their study, however, our material had a nearly complete absence of 7 T personnel. Although not significant, we found tendencies towards increased SMF symptom occurrence and attribution among MR personnel considering reported vertigo, nausea, metallic taste, and illusion of movement compared to CT personnel. These symptoms were mainly reported when participants worked close to the scanner bore and during movement, i.e. during exposure to strong SMFs and increased motion-induced time-varying magnetic fields. Given that the demand for stronger field MR systems keeps growing, we might encounter higher symptom prevalence in the future [31]. Considering the inconsistent results, radiology departments need to establish education and protective measures to minimize the risk of SMF-related adverse health effects for MR personnel.
Another key finding in our study was the influence of stress on reported symptoms, regardless of image modality. As our study did not delve any deeper into organizational structures or work culture, nor aimed to evaluate environmental stressors, we cannot establish any causality or pinpoint specific stress-related objectives to be addressed for decreasing symptom occurrence. However, other studies have also found stress to be an important contributing factor in reported health effects by MR personnel [13, 30]. Working shifts, working in larger departments, and/or having 6–15 years of work experience were the greatest stressors among Finnish radiographers [32]. Conversely, stress was not seen to impact the symptom prevalence in general among MR personnel in a previous Swedish study [8]. In that study, however, no control group was included and the number of participants was limited (n = 59).
Head ringing/tinnitus has been reported during SMF exposure [3, 29, 33]. We chose to look at head ringing separately from all other symptoms because it also can be triggered by acoustic noise [34]. Accordingly, CT personnel reported head ringing when being inside the CT room. Moreover, CT personnel revealed a greater risk of experiencing acoustic noise in their work environment as troublesome. While we lack data on sound pressure levels and on noise characteristics that were perceived as troublesome, we hypothesize from clinical experience that fans and X-ray tube rotations contribute to noise nuisance. Increased patient and personnel turnover during CT shifts might also aggravate noise exposure. On the other hand, awareness of acoustic noise and sound pressure levels from MR scanners, at least in Sweden, has led to site building revisions regarding acoustics in MR workspaces—but not to the same extent regarding CT environments.
One explanation for the MR radiographers’ mildly reported health complaints in our study might be due to adaptation to the work environment. The adaptation theory is supported by comparing the symptom outcome among MR personnel with less than one year of experience, as done by Zanotti et al [23, 35]. There, participants reported symptoms more frequently during their first two months at MR, but the prevalence declined thereafter. Incidentally, the mean work experience with MR was rather high in our study cohort (14 years). Experienced MR personnel have likely developed habits to mitigate adverse effects from both SMF and acoustic noise exposure, such as moving slowly within the SMF vicinity and wearing hearing protection during scanning. Additionally, the so-called healthy worker effect [36] cannot be ruled out as a bias among MR personnel in our study, since the strong magnetic fields make it problematic for certain personnel to enter the scanning room, i.e., persons with active implants, or those who experience severe symptoms in general. However, our outcome might also reflect a successful result of the 2013 implemented EU guidelines [22]—which acknowledge MR as an occupational risk environment and states both exposure limits and strategies to minimize adverse health effects. The CT environment outside of radiation safety may have been foreshadowed in that regard.
Limitations
Any subjectively reported hearing function should be interpreted with caution as participant-perceived ratings may lack correlation with audiometric data, and hearing impairment is often underreported [37]. Audiometric testing would, however, not have been feasible given our study design. Participants’ experience of work environmental noise and adaptation to mitigation strategies thereof still highlighted acoustic noise as an issue in MR and CT work environments.
Our way of distributing the questionnaires left us no possibility to control how many workers had been asked to partake in the study. A brief overview of the MR personnel in Sweden, however, gives us an approximate response rate of 60% [25]. Moreover, as our primary aim was to explore symptom reports from MR users, we wanted our controls (CT) to work within the same hospitals. Therefore, we chose not to send out the questionnaire to hospitals that did not have access to MRI. As such, our CT controls are less numerically representative compared to the MR cohort with regards to national demographics, which might induce a bias. Many of our participants were also working with other imaging modalities in addition to MR and/or CT, e.g., conventional radiography, which admittedly reflects normal working conditions for MR and CT personnel in Sweden. Still, such work environmental factors or organizational biases cannot be excluded as confounders, and might, conversely, be an explanation as to why adverse symptoms are not more prevalent in our study.
Conclusion
Comparing MR personnel to a CT control group suggests that adverse symptoms cannot solely be explained by SMF exposure and acoustic noise exposure, and our hypothesis that MR radiographers report more symptoms in general than CT radiographers was rejected. Stress was an important confounder for symptom onset. However, SMF symptoms were significantly more prevalent among MR radiographers whose work included 3-T systems compared to those only working at ≤ 1.5 T. MR personnel also tended to use more mitigation strategies when working close to the scanner than did CT personnel. Acoustic noise was generally mitigated by MR personnel, whereas CT personnel experienced work environmental noise as more troublesome. This finding might imply that reducing noise nuisance within CT environments is needed and ought to be further looked into.
Abbreviations
- dB:
-
Decibel
- ICNIRP:
-
International Commission on Non-Ionizing Radiation Protection
- OR:
-
Odds ratio
- SMF:
-
Static magnetic field
- T:
-
Tesla
References
Ladd ME, Bachert P, Meyerspeer M et al (2018) Pros and cons of ultra-high-field MRI/MRS for human application. Prog Nucl Magn Reson Spectrosc 109:1–50
McRobbie WD (2020) Essentials of MRI Safety, 1st edn. Wiley-Blackwell, Hoboken
Schaap K, Christopher-de Vries Y, Mason CK, de Vocht F, Portengen L, Kromhout H (2014) Occupational exposure of healthcare and research staff to static magnetic stray fields from 1.5-7 Tesla MRI scanners is associated with reporting of transient symptoms. Occup Environ Med 71:423–429
Hartwig V, Romeo S, Zeni O (2018) Occupational exposure to electromagnetic fields in magnetic resonance environment: basic aspects and review of exposure assessment approaches. Med Biol Eng Comput 56:531–545
Price DL, De Wilde JP, Papadaki AM, Curran JS, Kitney RI (2001) Investigation of acoustic noise on 15 MRI scanners from 0.2 T to 3 T. J Magn Reson Imaging 13:288–293
Moelker A, Maas RA, Vogel MW, Ouhlous M, Pattynama PM (2005) Importance of bone-conducted sound transmission on patient hearing in the MR scanner. J Magn Reson Imaging 22:163–169
Coskun O (2011) Magnetic resonance imaging and safety aspects. Toxicol Ind Health 27:307–313
Wilén J, de Vocht F (2011) Health complaints among nurses working near MRI scanners--a descriptive pilot study. Eur J Radiol 80:510–513
Schaap K, Portengen L, Kromhout H (2016) Exposure to MRI-related magnetic fields and vertigo in MRI workers. Occup Environ Med 73:161–166
van Nierop LE, Slottje P, van Zandvoort MJ, de Vocht F, Kromhout H (2012) Effects of magnetic stray fields from a 7 Tesla MRI scanner on neurocognition: a double-blind randomised crossover study. Occup Environ Med 69:759–766
International Commission on Non-Ionizing Radiation Protection (ICNIRP) (2014) Guidelines for limiting exposure to electric fields induced by movement of the human body in a static magnetic field and by time-varying magnetic fields below 1 Hz. Health Phys 106:418–425
Schenck JF, Dumoulin CL, Redington RW, Kressel HY, Elliott RT, McDougall IL (1992) Human exposure to 4.0-Tesla magnetic fields in a whole-body scanner. Med Phys 19:1089–1098
de Vocht F, Batistatou E, Mölter A et al (2015) Transient health symptoms of MRI staff working with 1.5 and 3.0 Tesla scanners in the UK. Eur Radiol 25:2718–2726
Glover PM, Cavin I, Qian W, Bowtell R, Gowland PA (2007) Magnetic-field-induced vertigo: a theoretical and experimental investigation. Bioelectromagnetics 28:349–361
Roberts DC, Marcelli V, Gillen JS, Carey JP, Della Santina CC, Zee DS (2011) MRI magnetic field stimulates rotational sensors of the brain. Curr Biol 21:1635–1640
Heilmaier C, Theysohn JM, Maderwald S, Kraff O, Ladd ME, Ladd SC (2011) A large-scale study on subjective perception of discomfort during 7 and 1.5 T MRI examinations. Bioelectromagnetics 32:610–619
Hansson B, Markenroth Bloch K, Owman T et al (2020) Subjectively reported effects experienced in an actively shielded 7T MRI: a large-scale study. J Magn Reson Imaging 52:1265–1276
International Commission on Non-Ionizing Radiation Protection (ICNIRP) (2009) Guidelines on limits of exposure to static magnetic fields. Health Phys 96:504–514
The Swedish Work Environment Authority (2016) Elektromagnetiska fält. Arbetsmiljöverkets föreskrifter om elektromagnetiska fält och allmänna råd om tillämpningen av föreskrifterna. In: Arbetsmiljöverket. Available via https://www.av.se/arbetsmiljoarbete-och-inspektioner/publikationer/foreskrifter/elektromagnetiska-falt-afs-20163-foreskrifter/. Accessed 6 Dec 2021.
Bongers S, Slottje P, Kromhout H (2017) Hearing loss associated with repeated MRI acquisition procedure-related acoustic noise exposure: an occupational cohort study. Occup Environ Med 74:776–784
Heinrich A, Szostek A, Nees F, Meyer P, Semmler W, Flor H (2011) Effects of static magnetic fields on cognition, vital signs, and sensory perception: a meta-analysis. J Magn Reson Imaging 34:758–763
European Union (2013) Directive 2013/35/EU of the European Parliament and of the Council of 26 June 2013 on the minimum health and safety requirements regarding the exposure of workers to the risks arising from physical agents (electromagnetic fields) (20th individual Directive within the meaning of Article 16(1) of Directive 89/391/EEC) and repealing Directive 2004/40/EC. Available via https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32013L0035. Accessed 6 dec 2021.
Zanotti G, Ligabue G, Gobba F (2015) Subjective symptoms and their evolution in a small group of magnetic resonance imaging (MRI) operators recently engaged. Electromagn Biol Med 34:262–264
Mohammed S, Rosenkrantz AB, Recht MP (2020) Preventing burnout in the face of growing patient volumes in a busy outpatient CT suite: a technologist perspective. Curr Probl Diagn Radiol 49:70–73
Hansson B, Olsrud J, Wilén J, Owman T, Höglund P, Björkman-Burtscher IM (2020) Swedish national survey on MR safety compared with CT: a false sense of security? Eur Radiol 30:1918–1926
Elo AL, Leppänen A, Jahkola A (2003) Validity of a single-item measure of stress symptoms. Scand J Work Environ Health 29:444–451
Anderson K, Stridh G, Fagerlund I, Larsson B (1993) The MM-questionnaire – a tool when solving lndoor climate problems. Örebro, Sweden, Department of Occupational and Environmental Medicine. Available via http://www.inomhusklimatproblem.se/publikations/2_publ_bas.html. Accessed 10 March 2022.
Ghadimi-Moghadam A, Mortazavi SMJ, Hosseini-Moghadam A et al (2018) Does exposure to static magnetic fields generated by magnetic resonance imaging scanners raise safety problems for personnel? J Biomed Phys Eng 8:333–336
de Vocht F, van Drooge H, Engels H, Kromhout H (2006) Exposure, health complaints and cognitive performance among employees of an MRI scanners manufacturing department. J Magn Reson Imaging 23:197–204
Bravo G, Modenese A, Arcangeli G et al (2021) Subjective symptoms in magnetic resonance imaging personnel: a multi-center study in Italy. Front Public Health. https://doi.org/10.3389/fpubh.2021.699675
Schaap K, Christopher-De Vries Y, Crozier S, De Vocht F, Kromhout H (2014) Exposure to static and time-varying magnetic fields from working in the static magnetic stray fields of MRI scanners: a comprehensive survey in the Netherlands. Ann Occup Hyg 58:1094–1110
Lohikoski K, Roos M, Suominen T (2019) Workplace culture assessed by radiographers in Finland. Radiography (Lond) 25:e113–e118
Heinrich A, Szostek A, Meyer P et al (2013) Cognition and sensation in very high static magnetic fields: a randomized case-crossover study with different field strengths. Radiology 266:236–245
Levine RA, Oron Y (2015) Chapter 23 - Tinnitus. In: Aminoff MJ, Boller F, Swaab DF (eds) Handbook of Clinical Neurology. Elsevier, pp 409–431
Zanotti G, Ligabue G, Korpinen L, Gobba F (2016) Subjective symptoms in Magnetic Resonance Imaging operators: prevalence, short-term evolution and possible related factors. Med Lav 107:263–270
Chowdhury R, Shah D, Payal AR (2017) Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods - A Review. Indian J Occup Environ Med 21:2–8
Tsimpida D, Kontopantelis E, Ashcroft D, Panagioti M (2020) Comparison of self-reported measures of hearing with an objective audiometric measure in adults in the english longitudinal study of ageing. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2020.15009
Funding
Open access funding provided by Umea University. This study has received funding from the Skåne University Hospital foundations and donations and the Academy of Care Science, Skåne University Hospital, Lund, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Isabella M. Björkman-Burtscher (Department of Radiology, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; Department of Radiology, Sahlgrenska University Hospital, Västra Götalands Region, Gothenburg, Sweden).
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the appropriate ethical reviews committee. Study participation was voluntary and all data were collected anonymously.
Ethical approval
Institutional Review Board approval was obtained by the Swedish Ethical Review Authority—formerly called the local ethical review committee (DNR 2014/867).
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in: Hansson B, Olsrud J, Wilén J, Owman T, Höglund P, Björkman-Burtscher IM (2020) Swedish national survey on MR safety compared with CT: a false sense of security? Eur Radiol 30:1918-1926.
Methodology
• prospective
• cross-sectional study
• single-center study with a national study cohort recruitment
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Glans, A., Wilén, J., Lindgren, L. et al. Health effects related to exposure of static magnetic fields and acoustic noise—comparison between MR and CT radiographers. Eur Radiol 32, 7896–7909 (2022). https://doi.org/10.1007/s00330-022-08843-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08843-y