Abstract
Objectives
This study aimed to compare the accuracy of PET/CT parameters with CT parameters for directing bone biopsies.
Methods
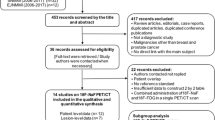
The study was an IRB-approved retrospective study of 388 patients who underwent both 2-[18F] FDG PET/CT and CT within 6 weeks before a bone biopsy. Age, sex, cancer type, lesion length, SUVmax, tumor to liver (T/L) ratio, CT attenuation, difference in CT attenuation between the lesion and normal bone (delta CT attenuation), and the absolute delta CT attenuation were used as predictors. T tests and chi-squared tests were used to compare variables. DeLong’s test was used to compare receiver operator characteristic (ROC) curves.
Results
We reviewed the data from 388 patients. Of these, 295 patients had bone lesion biopsies, and 93 patients had bone marrow aspirations/biopsies. Biopsies of larger bone lesions (p = 0.033) and bone lesions with higher SUVmax (p = 0.005) were more likely to show malignancy. For bone lesions, the ROC curve for the SUVmax (AUC = 0.6827) was better than the ROC curves for delta CT attenuation (AUC = 0.5766, p = 0.032) and absolute delta CT attenuation (AUC = 0.5491, p = 0.006), but not significantly better than the ROC curves for CT attenuation (AUC = 0.5894, p = 0.061) and T/L ratio (AUC = 0.6778, p = 0.774). A threshold SUVmax of 5.25 had an accuracy of 0.713, sensitivity of 0.766, and specificity of 0.549 to predict malignancy in bone lesion biopsies. None of these variables predicted malignancy in bone marrow biopsies (p > 0.05 for all).
Conclusions
Metabolic 2-[18F]FDG PET/CT parameters have more clinical impact for planning bone biopsies as compared to CT parameters.
Key Points
• The 2-[ 18 F]FDG PET/CT measurement (SUVmax) has more clinical impact for planning bone biopsies as compared to CT measurements.
• Neither the change in CT attenuation of the lesion relative to normal bone nor the absolute value of this change was a significant predictor of malignancy.
• 2-[ 18 F]FDG PET/CT may have clinical benefit and an additional role in directing bone biopsies.





Similar content being viewed by others
Abbreviations
- 2-[18F]FDG:
-
2-deoxy-2-[ 18F]fluoro-D-glucose
- ABP:
-
American Board of Pathology
- ABR:
-
American Board of Radiology
- Absolute delta CT attenuation:
-
Absolute value of the Delta CT attenuation
- AUC:
-
Area under the curve
- CONSORT :
-
Consolidated Standards of Reporting Trials
- CT :
-
Computed tomography
- Delta CT attenuation:
-
CT attenuation of the lesion–CT attenuation of normal bone
- EANM:
-
European Association of Nuclear Medicine
- EMR:
-
Electronic medical record
- HNSCC:
-
Head and neck squamous cell carcinoma
- HU:
-
Hounsfield units
- IRB:
-
Institutional review board
- MDP:
-
Tc-99 m methylene diphosphonate
- MRI:
-
Magnetic resonance imaging
- PET/CT:
-
Positron emission tomography/computed tomography
- ROC:
-
Receiver operator characteristic
- SD:
-
Standard deviation
- SUVmax :
-
Maximum standardized uptake value
- T/L ratio:
-
Ratio of SUVmax of the lesion to the liver SUVmax
References
https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed 10 Apr 2020
SebroR Mari-Aparici C, Hernandez-Pampaloni M (2013) Value of true whole-body FDG-PET/CT scanning protocol in oncology: optimization of its use based on primary diagnosis. Acta Radiol 54(5):534–9. https://doi.org/10.1177/0284185113476021
Schwartz L, Supuran CT, Alfarouk KO (2017) The Warburg effect and the hallmarks of cancer. Anticancer Agents Med Chem 17(2):164–170
Shen B, Huang T, Sun Y, Jin Z, Li XF (2017) Revisit 18F-fluorodeoxyglucose oncology positron emission tomography: “systems molecular imaging” of glucose metabolism. Oncotarget. 8(26):43536–43542
Skovgaard D, Kjaer M, El-Ali H, Kjaer A (2009) 18F-fluorodeoxyglucose and PET/CT for noninvasive study of exercise-induced glucose uptake in rat skeletal muscle and tendon. Eur J Nucl Med Mol Imaging 36(5):859–868
Avril N (2004) GLUT1 expression in tissue and (18)F-FDG uptake. J Nucl Med 45(6):930–932
Macedo F, Ladeira K, Pinho F et al (2017) Bone metastases: an overview. Oncol Rev 11(1):321
Yang HL, Liu T, Wang XM et al (2011) Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol 21:2604–2617
Boellaard R, O'Doherty MJ, Weber WA et al (2010) FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nucl Med Mol Imaging 37(1):181–200
Huang J, Huang L, Zhou J et al (2017) Elevated tumor-to-liver uptake ratio (TLR) from 18F-FDG-PET/CT predicts poor prognosis in stage IIA colorectal cancer following curative resection. Eur J Nucl Med Mol Imaging 44(12):1958–1968
Wang C, Zhao K, Hu S et al (2020) The PET-derived tumor-to-liver standard uptake ratio (SUVTLR) is superior to tumor SUVmax in predicting tumor response and survival after chemoradiotherapy in patients with locally advanced esophageal cancer. Front Oncol 10:1630
Hofheinz F, Bütof R, Apostolova I et al (2016) An investigation of the relation between tumor-to-liver ratio (TLR) and tumor-to-blood standard uptake ratio (SUR) in oncological FDG PET. EJNMMI Res 6:19
de Mestier L, Armani M, Cros J et al (2019) Lesion-by-lesion correlation between uptake at FDG PET and the Ki67 proliferation index in resected pancreatic neuroendocrine tumors. Dig Liver Dis 51(12):1720–1724
Ulano A, Bredella MA, Burke P et al (2016) Distinguishing untreated osteoblastic metastases from enostoses using CT attenuation measurements. AJR Am J Roentgenol 207(2):362–368
Lee HT, Pukenas BA, Sebro R (2020) Change in bone CT attenuation and C-Reactive protein are predictors of bone biopsy culture positivity in patients with vertebral discitis/osteomyelitis. Spine (Phila Pa1976) 45(17):1208–1214
Nakahara T, Owaki Y, Shindou T, Nakajima K, Jinzaki M (2019) Bone SPECT-based segmented attenuation correction for quantitative analysis of bone metastasis (B-SAC): comparison with CT-based attenuation correction. EJNMMI Res 9(1):27
Cicchetti DV (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 6(4):284–290
Costelloe CM, Chuang HH, Chasen BA et al (2013) (2013) Bone windows for distinguishing malignant from benign primary bone tumors on FDG PET/CT. J Cancer 4(7):524–530
Thie JA (2004) Understanding the standardized uptake value, its methods, and implications for usage. J Nucl Med 45(9):1431–1434
Schwab JH, Healey JH (2007) FDG-PET lacks sufficient sensitivity to detect myxoid liposarcoma spinal metastases detected by MRI. Sarcoma. 2007:36785
Erly WK, Oh ES, Outwater EK (2006) The utility of in-phase/opposed-phase imaging in differentiating malignancy from acute benign compression fractures of the spine. AJNR Am J Neuroradiol 27(6):1183–1188
Perry MT, Sebro R (2018) Accuracy of opposed-phase magnetic resonance imaging for the evaluation of treated and untreated spinal metastases. Acad Radiol 25(7):877–882
Schmidt GP, Schoenberg SO, Schmid R et al (2006) Screening for bone metastases: whole-body MRI using a 32-channel system versus dual-modality PET-CT. Eur Radiol 17(4):939–949
Li J, Weissberg Z, Bevilacqua TA, Yu G, Weber K, Sebro R (2018) Concordance between fine-needle aspiration and core biopsies for osseous lesions by lesion imaging appearance and CT attenuation. Radiol Med 123(4):254–259
Jelinek JS, Murphey MD, Welker JA et al (2002) Diagnosis of primary bone tumors with image-guided percutaneous biopsy: experience with 110 tumors. Radiology 223:731–737
Leffler SG, Chew FS (1999) CT-guided percutaneous biopsy of sclerotic bone lesions: diagnostic yield and accuracy. AJR Am J Roentgenol 172:1389–1392
Spritzer CE, Afonso PD, Vinson EN et al (2013) Bone marrow biopsy: RNA isolation with expression profiling in men with metastatic castration-resistant prostate cancer--factors affecting diagnostic success. Radiology. 269:816–823
Loudini N, Glaudemans AWJM, Jutte PC et al (2020) The value of prebiopsy FDG-PET/CT in discriminating malignant from benign vertebral bone lesions in a predominantly oncologic population. Skeletal Radiol 49:1387–1395
Kumar R, Mittal BR, Bhattacharya A et al (2019) 18F-FDG PET/CT-guided real-time automated robotic arm-assisted needle navigation for percutaneous biopsy of hypermetabolic bone lesions: diagnostic performance and clinical impact. AJR Am J Roentgenol 212(1):W10–W18
Acknowledgements
RS was supported by R21 NIH/NIMH MH093415.
Funding
This study has received funding from the National Institutes of Health (NIH) Grant # R21 NIH/NIMH MH093415.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ronnie Sebro, MD, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (PhD in Biostatistics).
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• observational
• multihospital study performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 31 kb)
Rights and permissions
About this article
Cite this article
Sebro, R., Ashok, S.S. The utility of 2-[18F]FDG-PET/CT maximum SUV versus CT attenuation for directing bone biopsies. Eur Radiol 31, 6780–6792 (2021). https://doi.org/10.1007/s00330-021-07770-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07770-8