Abstract
Objectives
This study aimed to assess the diagnostic accuracy of computed tomography (CT) and time-resolved magnetic resonance angiography (TR-MRA) for patency after coil embolization of pulmonary arteriovenous malformations (PAVMs) and identify factors affecting patency.
Methods
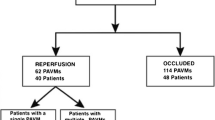
Data from the records of 205 patients with 378 untreated PAVMs were retrospectively analyzed. Differences in proportional reduction of the sac or draining vein on CT between occluded and patent PAVMs were examined, and receiver operating characteristic analysis was performed to assess the accuracy of CT using digital subtraction angiography (DSA) as the definitive diagnostic modality. The accuracy of TR-MRA was also assessed in comparison to DSA. Potential factors affecting patency, including sex, age, number of PAVMs, location of PAVMs, type of PAVM, and location of embolization, were evaluated.
Results
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of CT were 82%, 81%, 77%, 85%, and 82%, respectively, when the reduction rate threshold was set to 55%, which led to the highest diagnostic accuracy. The sensitivity, specificity, PPV, NPV, and accuracy of TR-MRA were 89%, 95%, 89%, 95%, and 93%, respectively. On both univariable and multivariable analyses, embolization of the distal position to the last normal branch of the pulmonary artery was a factor that significantly affected the prevention of patency.
Conclusions
TR-MRA appears to be an appropriate method for follow-up examinations due to its high accuracy for the diagnosis of patency after coil embolization of PAVMs. The location of embolization is a factor affecting patency.
Key Points
• Diagnosis of patency after coil embolization for pulmonary arteriovenous malformations (PAVMs) is important because a patent PAVM can lead to neurologic complications.
• The diagnostic accuracies of CT with a cutoff value of 55% and TR-MRA were 82% and 93%, respectively.
• The positioning of the coils relative to the sac and the last normal branch of the artery was significant for preventing PAVM patency.





Similar content being viewed by others
Abbreviations
- AVP:
-
AMPLATZER Vascular Plug
- CT:
-
Computed tomography
- DSA:
-
Digital subtraction angiography
- HHT:
-
Hereditary hemorrhagic telangiectasia
- MVP:
-
MVP Micro Vascular Plug
- NPV:
-
Negative predictive value
- PAVM:
-
Pulmonary arteriovenous malformation
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- TR-MRA:
-
Time-resolved magnetic resonance angiography
References
White RI Jr, Pollak JS, Wirth JA (1996) Pulmonary arteriovenous malformations: diagnosis and transcatheter embolotherapy. J Vasc Interv Radiol 7:787–804
Gossage JR, Kanj G (1998) Pulmonary arteriovenous malformations: a state of the art review. Am J Respir Crit Care Med 158:643–661
Etievant J, Si-Mohamed S, Vinurel N et al (2018) Pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia: correlations between computed tomography findings and cerebral complications. Eur Radiol 28:1338–1344
Woodward CS, Pyeritz RE, Chittams JL, Trerotola SO (2013) Treated pulmonary arteriovenous malformations: patterns of persistence and associated retreatment success. Radiology 269:919–926
Lee DW, White RI Jr, Egglin TK et al (1997) Embolotherapy of large pulmonary arteriovenous malformations: long-term results. Ann Thorac Surg 64:930–940
Prasad V, Chan RP, Faughnan ME (2004) Embolotherapy of pulmonary arteriovenous malformations: efficacy of platinum versus stainless steel coils. J Vasc Interv Radiol 15:153–160
Remy-Jardin M, Dumont P, Brillet PY, Dupuis P, Duhamel A, Remy J (2006) Pulmonary arteriovenous malformations treated with embolotherapy: helical CT evaluation of long-term effectiveness after 2-21-year follow-up. Radiology 239:576–585
Milic A, Chan RP, Cohen JH, Faughnan ME (2005) Reperfusion of pulmonary arteriovenous malformations after embolotherapy. J Vasc Interv Radiol 16:1675–1683
Hayashi S, Baba Y, Senokuchi T, Nakajo M (2012) Efficacy of venous sac embolization for pulmonary arteriovenous malformations: comparison with feeding artery embolization. J Vasc Interv Radiol 23:1566–1577
Letourneau-Guillon L, Faughnan ME, Soulez G et al (2010) Embolization of pulmonary arteriovenous malformations with amplatzer vascular plugs: safety and midterm effectiveness. J Vasc Interv Radiol 21:649–656
Kajiwara K, Urashima M, Yamagami T et al (2014) Venous sac embolization of pulmonary arteriovenous malformation: safety and effectiveness at mid-term follow-up. Acta Radiol 55:1093–1098
Gamondès D, Si-Mohamed S, Cottin V et al (2016) Vein diameter on unenhanced multidetector CT predicts reperfusion of pulmonary arteriovenous malformation after embolotherapy. Eur Radiol 26:2723–2739
Goyen M, Ruehm SG, Jagenburg A, Barkhausen J, Kröger K, Debatin JF (2001) Pulmonary arteriovenous malformation: characterization with time-resolved ultrafast 3D MR angiography. J Magn Reson Imaging 13:458–460
Fink C, Eichhorn J, Bock M (2002) Pulmonary arteriovenous malformation and aortopulmonary collateral imaged by time resolved contrast enhanced magnetic resonance angiography. Heart 88:292
Boussel L, Cernicanu A, Geerts L et al (2010) 4D time-resolved magnetic resonance angiography for noninvasive assessment of pulmonary arteriovenous malformations patency. J Magn Reson Imaging 32:1110–1116
Kawai T, Shimohira M, Kan H et al (2014) Feasibility of time-resolved MR angiography for detecting recanalization of pulmonary arteriovenous malformations treated with embolization with platinum coils. J Vasc Interv Radiol 25:1339–1347
Shimohira M, Kawai T, Hashizume T et al (2015) Reperfusion rates of pulmonary arteriovenous malformations after coil embolization: evaluation with time-resolved MR angiography or pulmonary angiography. J Vasc Interv Radiol 26:856–864.e1
Shovlin CL, Guttmacher AE, Buscarini E et al (2000) Diagnostic criteria for hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome). Am J Med Genet 91:66–67
Kawai T, Shimohira M, Ohta K et al (2016) The role of time-resolved MRA for post-treatment assessment of pulmonary arteriovenous malformations: a pictorial essay. Cardiovasc Intervent Radiol 39:965–672
Zhang J, Ding S, Zhao H et al (2020) Evaluation of chronic carotid artery occlusion by non-contrast 3D-MERGE MR vessel wall imaging: comparison with 3D-TOF-MRA, contrast-enhanced MRA, and DSA. Eur Radiol 30(11):5805–5814
Zhang X, Cao YZ, Mu XH et al (2020) Highly accelerated compressed sensing time-of-flight magnetic resonance angiography may be reliable for diagnosing head and neck arterial steno-occlusive disease: a comparative study with digital subtraction angiography. Eur Radiol 30:3059–3065
Schneider G, Uder M, Koehler M et al (2008) MR angiography for detection of pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. AJR Am J Roentgenol 190:892–901
Meaney JF, Weg JG, Chenevert TL, Stafford-Johnson D, Hamilton BH, Prince MR (1994) Diagnosis of pulmonary embolism with magnetic resonance angiography. N Engl J Med 336:1422–1427
Togao O, Obara M, Helle M et al (2020) Vessel-selective 4D-MR angiography using super-selective pseudo-continuous arterial spin labeling may be a useful tool for assessing brain AVM hemodynamics. Eur Radiol 30(12):6452–6463
Anzalone N, Righi C, Simionato F et al (2000) Three-dimensional time-of-flight MR angiography in the evaluation of intracranial aneurysms treated with Guglielmi detachable coils. AJNR Am J Neuroradiol 21:746–752
Hennemeyer CT, Wicklow K, Feinberg DA, Derdeyn CP (2001) In vitro evaluation of platinum Guglielmi detachable coils at 3 T with a porcine model: safety issues and artifacts. Radiology 219:732–737
D’Orazio F, Splendiani A, Gallucci M (2014) 320-Row detector dynamic 4D-CTA for the assessment of brain and spinal cord vascular shunting malformations. A technical note. Neuroradiol J 27:710–717
Hadizadeh DR, Marx C, Gieseke J, Schild HH, Willinek WA (2014) High temporal and high spatial resolution MR angiography (4D-MRA). Rofo 186:847–859
Tamada D, Kromrey ML, Ichikawa S, Onishi H, Motosugi U (2020) Motion artifact reduction using a convolutional neural network for dynamic contrast enhanced MR imaging of the liver. Magn Reson Med Sci 19:64–76
Hamamoto K, Matsuura K, Chiba E, Okochi T, Tanno K, Tanaka O (2016) Feasibility of non-contrast-enhanced MR angiography using the time-SLIP technique for the assessment of pulmonary arteriovenous malformation. Magn Reson Med Sci 15:253–265
Sagara K, Miyazono N, Inoue H, Ueno K, Nishida H, Nakajo M (1998) Recanalization after coil embolotherapy of pulmonary arteriovenous malformations: study of long-term outcome and mechanism for recanalization. AJR Am J Roentgenol 170:727–730
Saouti N, Westerhof N, Postmus PE, Vonk-Noordegraaf A (2010) The arterial load in pulmonary hypertension. Eur Respir Rev 19:197–203
Rosenhek R, Korschineck I, Gharehbaghi-Schnell E et al (2003) Fibrinolytic balance of the arterial wall: pulmonary artery displays increased fibrinolytic potential compared with aorta. Lab Invest 83:871–876
Dinkel HP, Triller J (2002) Pulmonary arteriovenous malformations: embolotherapy with superselective coaxial catheter placement and filling of venous sac with Guglielmi detachable coils. Radiology 223:709–714
Shimohira M, Kawai T, Hashizume T, Muto M, Kitase M, Shibamoto Y (2018) Usefulness of hydrogel-coated coils in embolization of pulmonary arteriovenous malformations. Cardiovasc Intervent Radiol 41:848–855
Maruno M, Kiyosue H, Tanoue S et al (2016) Renal arteriovenous shunts: clinical features, imaging appearance, and transcatheter embolization based on angioarchitecture. Radiographics 36:580–595
Kim DJ, Willinsky RA, Krings T, Agid R, Terbrugge K (2011) Intracranial dural arteriovenous shunts: transarterial glue embolization--experience in 115 consecutive patients. Radiology 258:554–561
Jacobowitz GR, Rosen RJ, Rockman CB et al (2001) Transcatheter embolization of complex pelvic vascular malformations: results and long-term follow-up. J Vasc Surg 33:51–55
Maruno M, Kiyosue H, Hongo N, Matsumoto S, Mori H (2018) Where is the origin of the last normal branch from feeding artery of pulmonary arteriovenous malformations? Cardiovasc Intervent Radiol 41:1849–1856
Stein EJ, Chittams JL, Miller M, Trerotola SO (2017) Persistence in coil-embolized pulmonary arteriovenous malformations with feeding artery diameters of 3 mm or less: a retrospective single-center observational study. J Vasc Interv Radiol 28:442–449
Tapping CR, Ettles DF, Robinson GJ (2011) Long-term follow-up of treatment of pulmonary arteriovenous malformations with AMPLATZER vascular plug and AMPLATZER vascular plug II devices. J Vasc Interv Radiol 22:1740–1746
Kucukay F, Özdemir M, Şenol E, Okten S, Ereren M, Karan A (2014) Large pulmonary arteriovenous malformations: long-term results of embolization with AMPLATZER vascular plugs. J Vasc Interv Radiol 25:1327–1332
Ratnani R, Sutphin PD, Koshti V et al (2019) Retrospective comparison of pulmonary arteriovenous malformation embolization with the polytetrafluoroethylene-covered nitinol microvascular plug, AMPLATZER plug, and coils in patients with hereditary hemorrhagic telangiectasia. J Vasc Interv Radiol 30:1089–1097
Bailey CR, Arun A, Towsley M et al (2019) MVP™ micro vascular plug systems for the treatment of pulmonary arteriovenous malformations. Cardiovasc Intervent Radiol 42:389–395
Acknowledgments
We would like to express our deep appreciation to Masaki Komiyama, Tatsuya Kawai and the members of HHT JAPAN.
Funding
This study has received funding by the Clinical Research Group of the Japanese Society for Transcatheter Hepatic Arterial Embolization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Masashi Shimohira.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
The requirement to obtain informed consent was waived because of the retrospective design.
Ethical approval
Institutional Review Board approval was obtained in each institution.
Approval number was as follows:
Nagoya City University Graduate School of Medical60160070
Oita University1061
Osaka University Graduate School of Medicine16362
Okayama University Medical Schoolken1611-009
Saitama Medical Center, Jichi Medical UniversityS16-090
Osaka City General Hospital1708047
Kobe University Graduate School of Medicine180012
Kurume University School of Medicine16194
Aichi Medical University2016-H272
Hyogo College of Medicine2522
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in following articles.
Makimoto S, Hiraki T, Gobara H, et al (2014) Association between reperfusion and shrinkage percentage of the aneurysmal sac after embolization of pulmonary arteriovenous malformation: evaluation based on contrast-enhanced thin-section CT images. Jpn J Radiol 32:266–273
Osuga K, Kishimoto K, Tanaka K, et al (2014) Initial experience with use of hydrogel microcoils in embolization of pulmonary arteriovenous malformations. Springerplus 17;3:609
Hamamoto K, Matsuura K, Chiba E, et al (2016) Feasibility of non-contrast-enhanced MR angiography using the time-SLIP technique for the assessment of pulmonary arteriovenous malformation. Magn Reson Med Sci 15:253–265
Maruno M, Kiyosue H, Hongo N, et al (2018) Where is the origin of the last normal branch from feeding artery of pulmonary arteriovenous malformations? Cardiovasc Intervent Radiol 41:1849–1856
Shimohira M, Kawai T, Hashizume T, et al (2015) Reperfusion rates of pulmonary arteriovenous malformations after coil embolization: evaluation with time-resolved MR angiography or pulmonary angiography. J Vasc Interv Radiol 26:856–864.e1
Shimohira M, Kawai T, Hashizume T, Muto M, Kitase M, Shibamoto Y (2018) Usefulness of hydrogel-coated coils in embolization of pulmonary arteriovenous malformations. Cardiovasc Intervent Radiol 41:848–855
Methodology
• retrospective
• diagnostic or prognostic study
• multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shimohira, M., Kiyosue, H., Osuga, K. et al. Location of embolization affects patency after coil embolization for pulmonary arteriovenous malformations: importance of time-resolved magnetic resonance angiography for diagnosis of patency. Eur Radiol 31, 5409–5420 (2021). https://doi.org/10.1007/s00330-020-07669-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07669-w