Abstract
Patients with Sjögren's syndrome are at a higher risk to develop oral candidiasis than the general population. As antifungals have many side-effects, new approaches are needed to address this problem. This randomized controlled study aimed to evaluate the short-term efficacy of probiotics in the reduction of oral candidal growth in patients with SS. Thirty-two Sjogren’s syndrome patients were randomly allocated in two groups receiving either Probiotics or placebo capsules twice a day for 5 weeks. The strains included in the probiotic capsule were Lactobacillus acidophilus, Lactobacillus bulgaricus, Streptococcus thermophilus and Bifidobacteriumbifidum. Oral rinse solution samples were collected and candidal levels were determined (CFU/mL) at baseline and after the 5-week experimental period. Pain, erythema and angular cheilitis were also assessed at baseline and after 2, 4 and 5-week. In the probiotic group, there was a statistically significant reduction of the candidal load from baseline to the 5th week respectively. However, the change in candidal load at the same time in the placebo group was not statistically significant. The tested probiotic product may represent an unconventional method to reduce candidal colonization, to prevent oral candidosis in patients with Sjogren’s syndrome.
Clinical trials registration ID NCT03840538 (https://clinicaltrials.gov/show/NCT03840538).


Similar content being viewed by others
Reference
Ramos-Casals M, Brito-Zerón P, Sisó-Almirall A, Bosch X (2012) Primary Sjogren syndrome. BMJ 345:e6280. https://doi.org/10.1136/bmj.e6280
Yan Z, Young AL, Hua H, Xu Y (2011) Multiple oral Candida infections in patients with Sjögren’s syndrome—prevalence and clinical and drug susceptibility profiles. J Rheumatol 38(11):2428–2431. https://doi.org/10.3899/jrheum.100819
Turner MD, Ship JA (2007) Dry mouth and its effects on the oral health of elderly people. J Am Dent Assoc 138(9):S15–S20. https://doi.org/10.14219/jada.archive.2007.0358
Radfar L, Shea Y, Fischer SH et al (2003) Fungal load and candidiasis in Sjögren’s syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 96(3):283–287. https://doi.org/10.1016/S1079-2104(03)00224-5
Mavragani CP, Moutsopoulos NM, Moutsopoulos HM (2006) The management of Sjogren’s syndrome. Nat Clin Pract Rheumatol 2(5):252–261. https://doi.org/10.1038/ncprheum0165
Oliver RJ, Dhaliwal HS, Theaker ED, Pemberton MN (2004) Patterns of antifungal prescribing in general dental practice. Br Dent J. https://doi.org/10.1038/sj.bdj.4811354
Sardi JCO, Almeida AMF, Mendes Giannini MJS (2011) New antimicrobial therapies used against fungi present in subgingival sites—a brief review. Arch Oral Biol 56(10):951–959. https://doi.org/10.1016/j.archoralbio.2011.03.007
Sardi JCO, Scorzoni L, Bernardi T, Fusco-Almeida AM, Mendes Giannini MJS (2013) Candida species: current epidemiology, pathogenicity, biofilm formation, natural antifungal products and new therapeutic options. J Med Microbiol 62(PART1):10–24. https://doi.org/10.1099/jmm.0.045054-0
González S, Sung H, Sepúlveda D, González MJ, Molina C (2014) Oral manifestations and their treatment in Sjögren’s syndrome. Oral Dis 20(2):153–161. https://doi.org/10.1111/odi.1210
Puupponen-Pimiä R, Aura A-M, Oksman-Caldentey K-M et al (2002) Development of functional ingredients for gut health. Trends Food Sci Technol 13:3–11. https://doi.org/10.1016/S0924-2244(02)00020-1
Kohler GA, Assefa S, Reid G (2012) Probiotic interference of lactobacillus rhamnosus GR-1 and lactobacillus reuteri RC-14 with the opportunistic fungal pathogen candida albicans. Infect Dis Obstet Gynecol. https://doi.org/10.1155/2012/636474
Elahi S, Pang G, Ashma R, Clancy R (2005) Enhanced clearance of Candida albicans from the oral cavities of mice following oral administration of Lactobacillus acidophilus. Clin Exp Immunol 141:29–36. https://doi.org/10.1111/j.1365-2249.2005.02811.x
Vitali C, Bombardieri S, Jonsson R et al (2002) Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis 61(6):554–558. https://doi.org/10.1136/ard.61.6.554
Li D, Li Q, Liu C et al (2014) Efficacy and safety of probiotics in the treatment of Candida-associated stomatitis. Mycoses 57(3):141–146. https://doi.org/10.1111/myc.12116
Byadarahally Raju S, Rajappa S (2011) Isolation and identification of Candida from the oral cavity. ISRN Dent 2011:1–7. https://doi.org/10.5402/2011/487921
Odds FC (1994) Candida albicans, the life and times of a pathogenic yeast. J Med Vet Mycol 32(Suppl 1):1–8. https://doi.org/10.1080/02681219480000681
Breivik H, Borchgrevink PC, Allen SM et al (2008) Assessment of pain. Br J Anaesth 101(1):17–24. https://doi.org/10.1093/bja/aen103
Ship JA, Vissinik A, Challacombes J (2007) Use of prophylactic antifungals in the immunocompromised host. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:1–14. https://doi.org/10.1016/j.tripleo.2006.11.003
Leung K, Leung W, Mcmillan A (2007) Supra-gingival microbiota in Sjögren’s syndrome. Clin Oral Investig 11:415–423. https://doi.org/10.1007/s00784-007-0132-1
Ishikawa KH, Mayer MPA, Miyazima TY et al (2015) A multispecies probiotic reduces oral candida colonization in denture wearers. J Prosthodont 24(3):194–199. https://doi.org/10.1111/jopr.12198
Hatakka K, Ahola AJ, Yli-Knuuttila H et al (2007) Probiotics reduce the prevalence of oral Candida in the elderly a randomized controlled trial. J Dent Res 86(2):125–130. https://doi.org/10.1177/154405910708600204
Miyazima TY, Ishikawa KH, Mayer MPA, Saad SMI, Nakamae AEM (2017) Cheese supplemented with probiotics reduced the Candida levels in denture wearers—RCT. Oral Dis 23(7):919–925. https://doi.org/10.1111/odi.12669
Mendonça FHBP, dos Santos SSF, Faria IDSD, Gonçalves e Silva CR, Jorge AOC, Leão MVP (2012) Effects of probiotic bacteria on Candida presence and IgA anti-Candida in the oral cavity of elderly. Braz Dent J 23(5):534–538. https://doi.org/10.1590/S0103-64402012000500011
Hu H, Merenstein DJ, Wang C et al (2013) Impact of eating probiotic yogurt on colonization by candida species of the oral and vaginal mucosa in HIV-infected and HIV-uninfected women. Mycopathologia 176(3–4):175–181. https://doi.org/10.1007/s11046-013-9678-4
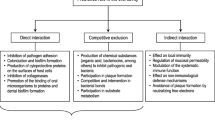
Boirivant M, Strober W (2007) The mechanism of action of probiotics. Curr Opin Gastroenterol 23:679–692. https://doi.org/10.1097/MOG.0b013e3282f0cffc
Acknowledgements
We would like to thank all participants in this study and the Faculty of Pharmacy, Cairo University, for supplying us with the placebo capsules used in the study.
Funding
This study is self-funded and no funding was received by any of the authors.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the design of the study, interpretation of the data, manuscript preparation and critical revisions of the manuscript. All authors have approved the final version submitted for publication and agreed to be held accountable for all aspects of the study. Design of the study: YK, BE, MK, ME and RY. Patient recruitment: ME. Data collection: YK, BE and ME. Random sequence generation: BE. Administration of the treatment: YK., Candidal culture: RY &YK. Assessment of the treatment: YK, MK. Statistical analysis and data interpretation: BE, YK. Manuscript preparation: YK, BE, and MK. Manuscript revision: YK, BE, MK, ME, and RY. All co-authors approve the final manuscript for publication and take full responsibility for the integrity of all parts.
Corresponding author
Ethics declarations
Conflict of interest
Yasmine Kamal, Mahmoud Kandil, Mervat Eissa, Reham Yousef and Basma ElSaadany declare that they have no competing conflicts of interest. All the authors declare that they have no relationship with the drug company.
Informed consent
A written informed consent was obtained from all the participants included in this study and no identifying information of any participant was included in this paper.
Ethical statement
The protocol for this clinical trial was approved by the Ethics Committee of the Faculty of Dentistry, Cairo University, under the ethical committee number: 15 10 12. All participants have provided written informed consent before the research was initiated. All shared data is in line with ICMJE recommendations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamal, Y., Kandil, M., Eissa, M. et al. Probiotics as a prophylaxis to prevent oral candidiasis in patients with Sjogren's syndrome: a double-blinded, placebo-controlled, randomized trial. Rheumatol Int 40, 873–879 (2020). https://doi.org/10.1007/s00296-020-04558-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04558-9