Abstract
Cervical spine involvement may lead to severe complications in rheumatoid arthritis (RA). In the era of modern therapies, atlantoaxial subluxation (AAS) may be rare; however, it may still be detected in asymptomatic patients. The onset of myelopathy can occur at any time. Altogether 49 female RA patients were included. Among them, 15 were methotrexate treated, biologic free, while 34 patients received biologics. The patients had no cervical pain or any neurological symptoms. We assessed the first (C1) and second (C2) cervical vertebrae by 3 T magnetic resonance imaging (MRI). In addition to AAS, we also determined odontoid erosion or periodontal soft tissue thickening. We associated our MRI findings with clinical, laboratory parameters, and hand radiography. We detected anterior AAS and soft tissue thickening in one-quarter, while odontoid erosions in eight (16%) of RA patients. There were no significant differences among the therapeutic subgroups. No posterior or vertical AAS was seen. Anterior AAS was associated with higher degree of inflammation, soft tissue thickening was seen at younger age, while odontoid erosions were associated with van der Heijde–Sharp scores of the hand. None of the patients had any lesions requiring surgery. The presence of cervical involvement in RA patients with 10–11 years of disease duration is still an important and frequent phenomenon. Higher disease activity and erosive disease are associated with atlantoaxial involvement. 3 T MRI is a sensitive method to assess AAS, as well as soft tissue lesions and odontoid erosions.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory rheumatic disease often involving the small joints of the hands and feet, the wrists, elbows, ankles, and knees [1]. RA may also involve the cervical spine in 20–70% of patients [1,2,3,4] and may start early during the disease course [5]. The atlantooccipital and atlantoaxial joints are the only vertebral segments without intervertebral disk. They comprise exclusively synovial joints. Therefore, these sections of the cervical spine are mostly affected by RA [6].
Chronic inflammation associated with RA may cause chronic synovitis, erosive pannus leading to odontoid erosion, laxity of ligaments, spinal instability, and subluxation in the atlantoaxial joint (AAS) [2, 4]. AAS can be anterior, posterior or vertical. Anterior AAS is the most common form and results from the laxity of ligaments. Posterior and vertical AAS are less frequently observed. Posterior AAS is mainly due to erosion of the dens and it is associated with a higher risk of cord compression compared to anterior AAS. Vertical AAS is the consequence of vertebral destruction and may even cause cranial settling with basal invagination [2,3,4, 7].
During the course of RA, the involvement of the cervical spine has no clinical symptoms for a long time due to the adaptability of neurological structures [5, 8]. Neurological signs may not be present up to 10 mm of AAS [8]. Suboccipital pain may be the first symptom of AAS [9]; however, it may be absent in more than half of patients with known instability [10]. Dizziness, tinnitus, and dysphagia may also occur [8, 10].
Functional cervical spine X-rays or MRI screening may detect asymptomatic abnormalities that may become symptomatic even after a sudden movement, trauma or retroposition of the head during anesthesia [2, 3, 6, 7, 11]. Moreover, surgical anesthesia relaxes the defensive muscles further increasing the risk of cord compression. Therefore, assessment of cervical spine involvement in RA patients should be part of preoperative workup [6, 12].
Spinal cord involvement is the most serious complication. Myelopathy could result in severe pain, irreversible neurologic deficits, respiratory dysfunction, and consequent death [6, 13]. Therefore, early diagnosis and proper treatment take priority. Surgical indications are therapy-resistant pain and neurologic deficits [6, 13].
According to the current European League Against Rheumatism (EULAR) recommendations, cervical spine involvement should primarily be detected by neutral position and functional X-rays of the cervical spine [11]. MRI scanning is more sensitive than conventional radiographs, showing early structural damage of the joints, as well as soft tissue involvement including periodontal synovitis, fibrous pannus, and odontoid erosions. MRI provides not only lateral, but also sagittal and coronal views and give explicit information of the soft tissue, as well as lesions of the neuraxis and epidural tissues. MRI should be performed if the patient has neurologic deficit or if there is indication of surgery [6, 11, 14].
With the introduction of effective treatments including targeted therapies and the treat-to-target strategy, cervical spine involvement in RA has become rare [6, 15]. Early initiation of therapy may prevent further cartilage destruction and ligamentous laxity [6]. However, it still remains an issue to select patients with an increased risk of cervical spine involvement to initiate therapeutic intervention before neurologic deterioration occurs [6, 15]. We found only very few reports on the association of biological therapy and cervical spine pathology in RA [15,16,17]. Thus, in the present cross-sectional study we wished to assess cervical spine involvement in Hungarian RA patients undergoing biologic versus methotrexate (MTX) therapy. In addition, as more powerful MRI instruments have recently become available, we wished to test the value of 3 T MRI imaging in the detection of cervical spine abnormalities.
Patients and methods
Forty-nine RA patients undergoing regular follow-ups at the Borsod County Teaching Hospital, Miskolc were recruited for the study. Patients with RA were in stable remission or with low disease activity. None of them had any cervical pain or neurological symptoms.
The major characteristics of these 49 patients are shown in Table 1. All patients were females, their median age was 60 (range 43–78) years. Their median disease duration was 9 (range 0.5–36) years. Altogether 71% were IgM rheumatoid factor (RF) positive, and 67% were ACPA (anti-CCP2) positive. Among these patients, 15 were biologic free. They had been receiving MTX for a median 6 (range 0.5–15) years in an average dose of 15 (range 7.5–20) mg/week. Altogether 34 patients had been receiving biologics [17 infliximab (IFX) as first-line biologic treatment and 17 tocilizumab (TCZ) as second-line biologic treatment after a failure of anti-TNF therapy], in combination with MTX. The median duration of biologic therapy was 5 (1–10) years, the median duration of MTX in the biologic-treated group was 5.5 (0.5–12) years in an average dose of 15 (7.5–25) mg/week. All patients underwent regular follow-ups every 3 months in the last 3 years.
Ethical approval (1046-63/2015) was obtained from the University of Miskolc Regional/Institutional Review Board. All patients signed informed consent forms. The study was performed according to the Declaration of Helsinki.
The study design is included in Fig. 1.
Cervical spine MRI investigations
All 49 RA patients underwent cervical MRI imaging in neutral position. We assessed the atlas and the axis to explore the inflammatory cervical spine involvement of RA patients. For this purpose, a Siemens Magnetom Verio 3 T (3 T) MRI instrument (Siemens, Munich, Germany) was used. All MRI scans were performed by a single radiologist (L. K.) and also read by a neurosurgeon/neuroradiologist (C. O.). The presence or absence of AAS, odontoid erosion, and periodontal soft tissue thickening were noted. AAS is defined by an increase in the atlantodental interval (ADI), the distance between the anterior surface of the dens and the posterior surface of C1, of > 3 mm. ADI > 3.5 mm means instability and ADI > 10 mm is an indication for surgery. None of the patients underwent plain radiography as we intended to detect early lesions. Therefore, all patients directly went for MRI.
Laboratory assessments
Serum IgM RF and high sensitivity CRP (hsCRP) were assessed by quantitative nephelometry (Cobas Mira Plus, Roche), using RF and CRP reagents, respectively (both Dialab, Vienna, Austria). RF levels > 50 IU/ml indicated seropositivity and hsCRP levels > 5 mg/l were considered elevated. Anti-CCP autoantibodies were detected in serum samples using the second generation Immunoscan-RA CCP2 ELISA test (Euro Diagnostica, Arnhem, The Netherlands). The assay was performed according to the instructions of the manufacturer. A concentration > 25 IU/ml indicated seropositivity.
We also calculated the mean ESR (mESR), CRP (mCRP) and DAS28 (mDAS28) values based on three monthly assessments within the past 3 years (up to 12 assessments) (Table 1). We applied the EULAR DAS28 remission and low disease activity criteria: DAS28 remission: < 2.6, low disease activity < 3.2.
Hand X-ray analysis
All RA patients underwent hand X-rays at the time of the cervical spine MRI study. Radiographs of the hand are used to determine the degree of disease progression. Erosions were scored according to the modified van der Heijde–Sharp method [18]. Each joint was graded on a score of 0 (normal) to 5 (maximal destruction).
Each radiograph was scaled by the same radiologist (L. K.) and then by a single rheumatologist (Z. K.), and the results were averaged.
Statistical analysis
The statistical analysis was processed using the IBM SPSS 25 software. Data are expressed as median and range. The distribution of continuous variables was examined by Kolmogorov–Smirnov test. Differences were evaluated by independent two-tailed t test or Mann–Whitney test as appropriate. Nominal variables were compared between groups using the Chi-squared or Fisher’s exact test, as appropriate. p values < 0.05 were considered significant.
We perfomed sample size power calculations. This indicated with respect to the three most important findings (Table 3, see later), the power percentages were 82%, 93%, and 83%. Usually, power > 80% is acceptable, so our study was well powered.
Results
Comparative description of RA patient subsets
With respect to clinical and disease activity markers, the total RA cohort, the MTX- and biologic-treated RA subsets did not differ from each other in most respects (Table 1). However, MTX-treated patients had significantly higher mDAS28 [3.23 (1.86–4.34) vs 2.59 (0.75–3.69); p = 0.036] than biologic-treated patients (Table 1). Moreover, TCZ-treated patients had significantly lower mDAS28 [2.2 (0.75–3.29) vs 2.78 (1.8–3.69); p < 0.001], mESR [9.56 (2.62–24) mm/h vs 22.38 (9.62–50.86) mm/h; p < 0.001] and higher modified van der Heijde–Sharp scores (vdHSS) [26 (3–70) vs 15 (0–146); p = 0.040), compared to IFX-treated individuals (Table 1).
Cervical spine MRI investigations
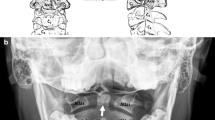
Anterior AAS developed in 26.5% of all RA patients, 20.0% of the MTX- and 29.4% of the biologic-treated subset. Within the biologic-treated subset, 23.5% of IFX- and 35.3% of TCZ-treated patients had anterior AAS (Table 2). Soft tissue thickening was observed in 24.5%, 33.3%, 20.6%, 35.3%, and 5.8% of all MTX-, any biologic-, IFX-, and TCZ-treated RA patients, respectively (Table 2). Finally, odontoid erosion was seen in 16.3% of all RA patients, 20.0% in MTX- and 14.7% of any biologic-treated, as well as in 11.8% of IFX- and 17.7% of TCZ-treated patients (Fig. 2; Table 2). There were no significant differences between MTX- and biologic-treated patients with respect to any MRI finding. Moreover, within the biologic-treated subset, there were no differences between the IFX- and TCZ-treated subsets (Table 2). No posterior or vertical AAS was detected in any patient.
Associations of cervical spine MRI pathologies with clinical, laboratory and hand X-ray parameters
Patients with anterior AAS had significantly higher mCRP compared to those without AAS [10.17 (2.16–21.8) vs 4.6 (0.16–26.32) mg/l; p = 0.019) (Table 3). Patients with AAS also had a tendency of higher mDAS28 and MTX dose, but these differences were not statistically significant (Table 3) (power: 82%). Patients with soft tissue thickening on MRI were significantly younger compared to those without this feature [54.5 (45–63) vs 61 (43–78) years; p = 0.013] (Table 3) (power: 93%). There was also a non-significant tendency of higher mDAS28 and mESR in patients with soft tissue thickening (Table 3). Finally, patients with odontoid erosion had significantly higher vdHSS compared to those without odontoid erosion [38 (21–86) vs 16 (0–146); p = 0.007) (Table 3) (power: 83%). With respect to other parameters, such as disease duration, seropositivity, MTX dose and duration, biologic treatment and its duration, TCZ versus IFX treatment, there were no differences between the three patient subsets (Table 3).
Discussion
Cervical spine involvement, a serious complication of RA, can be observed even in recent times, in the era of modern therapies. AAS, soft tissue thickening, or odontoid erosion may be identified even in asymptomatic patients. Isolated, mostly anterior AAS may develop early in the disease course and it can later be complicated with soft tissue involvement and odontoid erosions. Myelopathy may occur at any time initially leading to headache and neck pain, followed by more advanced neurological symptoms [8,9,10,11, 14]. As 3 T MRI instruments have only recently become available, we wished to try this technique to assess cervical spine pathology in RA. Moreover, there have been only very few reports with respect to cervical spine involvement in biologic-treated RA patients [15,16,17]. Our cohort included 49 RA patients with no cervical spine and neurological symptoms.
In RA, the most common cervical spine involvement is anterior AAS. We found this lesion in about quarter of our RA patients. Carotti et al. [14] described cervical involvement in 24% of early RA patients (disease duration < 12 months). In our cohort, anterior AAS was associated with higher mCRP and there was also a tendency of association with higher mDAS28 and MTX dose. In other studies, seropositivity, early onset of RA, high disease activity scores, erosive disease at baseline, and use of corticosteroids were predictors of AAS [7, 14]. Hand X-ray findings may also potentially predict AAS in RA [19]. In our hands, AAS was not associated with vdHSS. Importantly, the progressive damage of peripheral joints with indication of prosthetic implantation was also associated with cervical spine involvement. In RA, patients scheduled for hip or knee replacement surgery, 44–65% demonstrated AAS on pre-surgical radiographs [10].
MRI may be very useful when assessing cervical spine pathologies in RA as this technique, in comparison to conventional radiography, may also detect soft tissue thickening and odontoid erosions. We assessed our patients, in addition to AAS, for signs of synovitis and fibrotic pannus in the joints of C1 and C2 vertebrae, as well as for erosive lesions of the dens. Again, approximately quarter of our patients had soft tissue thickening and 16% had dens erosions. Interestingly, soft tissue thickening occurred at younger age, while odontoid erosions were associated with higher vdHSS indicating more pronounced peripheral joint destruction. As discussed above, in other studies, structural damage of small joints of the hand was rather associated with AAS [19].
As there have been few reports on the association of biologic therapy with cervical spine involvement in RA [15,16,17], we also tried to compare MTX- versus biologic-treated, as well as, within the biologic-treated subset, also IFX- versus TCZ-treated RA patient subsets. In our cross-sectional study, MTX- and biologic-treated patients had similar clinical features. Only mDAS28 was higher in the MTX-treated group. On the other hand, TCZ-treated patients had lower mDAS28 and mESR and somewhat lower mCRP compared to IFX-treated patients indicating that IFX and TCZ may have different effects on inflammatory activity. However, TCZ-treated patients had higher vdHSS suggesting that this subset may reflect a more severe group of patients. Despite these clinical and radiological differences between the RA subsets, no significant differences were found between any two patient subset with respect to AAS, soft tissue thickening or odontoid erosions. In 2019, Sandstrom et al. [15] published very recent data from the NEORACo early arthritis cohort. In this study, 99 treatment-naïve RA patients received conventional DMARD and corticosteroid and then they were randomized to receive IFX or placebo. After 10 years, 4.7% of the analyzed patients had cervical spine involvement. There were only two cases with AAS, both treated with IFX [15]. Thus, in early RA patients managed according to the treat-to-target strategy, AAS is relatively rare compared to our patients with 10–11 years of disease duration. Salli et al. [16] reported successful IFX treatment of periodontoid pannus in one RA patient. We have not found any other reports on the possible effects of biologics on cervical spine pathologies in RA. Kanayama et al. [17], who conducted a prospective study on 47 RA patients and received IFX for at least 1 year. IFX was able to suppress the progression of cervical lesions in 83% of patients showing good clinical response to IFX [17]. We did not find any reports with respect to TCZ treatment.
Our study has strengths and limitations. The major strength is its novelty studying cervical spine involvement in RA in the era of modern therapies, as well as the use of new 3 T MRI technology. Possible limitations include the relatively small number of patients, especially in the therapeutic subsets and the cross-sectional nature of our study. In addition, our cohort includes patients with longer disease duration; therefore, cervical spine pathologies are relatively more common than in early arthritis cohorts.
In conclusion, 3 T MRI may assess soft tissue involvement and odontoid erosions in addition to AAS. Despite of biologic therapy, 15–30% of RA patients still have preclinical cervical spine abnormalities that may be associated with higher degree of systemic inflammation and structural hand joint changes. MRI is a sensitive method to assess cervical spine involvement in RA patients with otherwise no neurological symptoms.
Change history
04 April 2020
In the original article, the first author’s given name and family name were interchanged as provided by the authors in the original manuscript.
References
Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS et al (2018) Rheumatoid arthritis. Nat Rev Dis Primers 4:18001
Neva MH, Kaarela K, Kauppi M (2000) Prevalence of radiological changes in the cervical spine—a cross sectional study after 20 years from presentation of rheumatoid arthritis. J Rheumatol 27:90–93
Zikou AK, Alamanos Y, Argyropoulou MI, Tsifetaki N, Tsampoulas C, Voulgari PV et al (2005) Radiological cervical spine involvement in patients with rheumatoid arthritis: a cross sectional study. J Rheumatol 32:801–806
Naranjo A, Carmona L, Gavrila D, Balsa A, Belmonte MA, Tena X et al (2004) Prevalence and associated factors of anterior atlantoaxial luxation in a nation-wide sample of rheumatoid arthritis patients. Clin Exp Rheumatol 22:427–432
Paimela L, Laasonen L, Kankaanpaa E, Leirisalo-Repo M (1997) Progression of cervical spine changes in patients with early rheumatoid arthritis. J Rheumatol 24:1280–1284
Wasserman BR, Moskovich R, Razi AE (2011) Rheumatoid arthritis of the cervical spine–clinical considerations. Bull NYU Hosp Jt Dis 69:136–148
Joaquim AF, Appenzeller S (2014) Cervical spine involvement in rheumatoid arthritis—a systematic review. Autoimmun Rev 13:1195–1202
Kramer J, Jolesz F, Kleefield J (1991) Rheumatoid arthritis of the cervical spine. Rheum Dis Clin N Am 17:757–772
Ferrante A, Ciccia F, Giammalva GR, Iacopino DG, Visocchi M, Macaluso F et al (2019) The craniovertebral junction in rheumatoid arthritis: state of the art. Acta Neurochir Suppl 2019 125:79–86
Imagama S, Oishi Y, Miura Y, Kanayama Y, Ito Z, Wakao N et al (2010) Predictors of aggravation of cervical spine instability in rheumatoid arthritis patients: the large joint index. J Orthop Sci 15:540–546
Colebatch AN, Edwards CJ, Ostergaard M, van der Heijde D, Balint PV, D'Agostino MA et al (2013) Eular recommendations for the use of imaging of the joints in the clinical management of rheumatoid arthritis. Ann Rheum Dis 72:804–814
Arawwawala D, Morgan P (2007) Preoperative cervical spine X-rays for patients with rheumatoid arthritis. Br J Hosp Med (Lond) 68:56
Casey AT, Crockard HA, Bland JM, Stevens J, Moskovich R, Ransford AO (1996) Surgery on the rheumatoid cervical spine for the non-ambulant myelopathic patient-too much, too late? Lancet 347:1004–1007
Carotti M, Salaffi F, Di Carlo M, Sessa F, Giovagnoni A (2019) Magnetic resonance imaging of the craniovertebral junction in early rheumatoid arthritis. Skelet Radiol 48:553–561
Sandstrom T, Rantalaiho V, Yli-Kerttula T, Kautiainen H, Malmi T, Karjalainen A et al (2019) Cervical spine involvement is very rare in patients with rheumatoid arthritis treated actively with treat to target strategy. Ten-year results of the NEORACo study. J Rheumatol. https://doi.org/10.3899/jrheum.190139
Salli A, Sahin N, Paksoy Y, Kucuksarac S, Ugurlu H (2009) Treatment of periodontoid pannus with infliximab in a patient with rheumatoid arthritis. J Clin Rheumatol 15:250–251
Kanayama Y, Kojima T, Hirano Y, Shioura T, Hayashi M, Funahashi K et al (2010) Radiographic progression of cervical lesions in patients with rheumatoid arthritis receiving infliximab treatment. Mod Rheumatol 20:273–279
van der Heijde D (2000) How to read radiographs according to the sharp/van der heijde method. J Rheumatol 27:261–263
Chung J, Bak KH, Yi HJ, Chun HJ, Ryu JI, Han MH (2019) Upper cervical subluxation and cervicomedullary junction compression in patients with rheumatoid arthritis. J Korean Neurosurg Soc 62:661–670
Acknowledgements
Open access funding provided by University of Debrecen (DE). This research was supported by the European Union and the State of Hungary and co-financed by the European Social Fund in the framework of TAMOP-4.2.4.A/2-11/1-2012-0001 ‘National Excellence Program’ (Z. S.); and by the European Union Grants GINOP-2.3.2-15-2016-00015 and GINOP-2.3.2-15-2016-00050 (Z. S.).
Author information
Authors and Affiliations
Contributions
All authors listed below meet at least the four authorship criteria, which are as follows: (1) substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; and (2) drafting the work or revising it critically for important intellectual content; and (3) final approval of the version to be published; and (4) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. No. 2–3–4 apply for all authors. In addition, under no. 1, here are the details: CO: study design, data acquisition, and interpretation. ZK: study design, data acquisition, and interpretation. LK: data acquisition and interpretation. KH: data analysis and interpretation. LT: data analysis and interpretation. DB: study design and data analysis. ZS: head of study group, data analysis, draft writing, supervision, and study design. Author statement: All co-authors are familiar with the final version of the manuscript and take full responsibility for the integrity of the study and all parts of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Conference abstracts (1) Kardos Z, Oláh C, Kostyál L, Hodosi K, Tamási L, Szekanecz Z. Cervical spine involvement in rheumatoid arthritis. Ann Rheum Dis 78 (Suppl 2): 1622, 2019 (EULAR congress). (2) Kardos Zs, Oláh Cs, Kostyál L, Hodosi K, Tamási L, Szekanecz Z. Rheumatoid arthritis – synovitis, erosions beyond the hand joints [Hungarian]. Hung Rheumatol 60: 138, 2019 (Congress of the Hungarian Association of Rheumatologists). /there is no DOI available).
The original article was revised due to interchange of given name and family name of the first author.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oláh, C., Kardos, Z., Kostyál, L. et al. Assessment of cervical spine involvement in rheumatoid arthritis patients in the era of biologics: a real-life, cross-sectional MRI study. Rheumatol Int 40, 915–921 (2020). https://doi.org/10.1007/s00296-020-04549-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-020-04549-w