Abstract
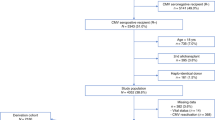
It has been shown recently that donor and/or recipient cytomegalovirus (CMV) seropositivity is associated with a significant overall survival (OS) decline in acute leukemia patients who underwent allogeneic hematopoietic stem cell transplantation (allo-HSCT). We now analyzed the prognostic impact of the donor/recipient CMV serostatus in 6968 patients with chronic hematological malignancies who underwent allo-HSCT. Donor and/or recipient CMV seropositivity was associated with a significantly reduced 2-year progression-free survival (PFS, 50% vs. 52%, p = 0.03) and OS (62% vs. 65%, p = 0.01). Multivariate Cox regression analyses showed an independent negative prognostic impact of donor and/or recipient CMV seropositivity on PFS (HR, 1.1; 95% CI, 1.0–1.2; p = 0.03), OS (HR, 1.1; 95% CI, 1.0–1.2; p = 0.003), and non-relapse mortality (HR, 1.2; 95% CI, 1.0–1.3; p = 0.02). OS decline was strongest for CMV-seropositive recipients with a CMV-seronegative donor (HR, 1.2; 95% CI, 1.1–1.3), followed by CMV-seropositive patients with a CMV-seropositive donor (HR, 1.1; 95% CI, 1.0–1.2). Conversely, OS did not differ significantly between CMV-seronegative recipients allografted from a CMV-seropositive donor (HR, 1.0; 95% CI, 0.9–1.2) and patients with donor/recipient CMV seronegativity (p = 0.001 for the four groups together). Non-relapse mortality was also significantly (p = 0.01) higher for CMV-seropositive patients with a CMV-seronegative graft (HR, 1.2; 95% CI, 1.1–1.4) than for CMV-seropositive patients with a CMV-seropositive graft (HR, 1.1; 95% CI, 0.9–1.2) or CMV-seronegative recipients with a CMV-seropositive graft (HR, 1.0; 95% CI, 0.8–1.2). Donor and/or recipient CMV seropositivity still results in an OS decline in patients with chronic hematological malignancies who have undergone allo-HSCT. However, this OS decline seems to be lower than that described for acute leukemia patients previously.

Similar content being viewed by others
References
Schmidt-Hieber M, Labopin M, Beelen D, Volin L, Ehninger G, Finke J, Socié G, Schwerdtfeger R, Kröger N, Ganser A, Niederwieser D, Polge E, Blau IW, Mohty M (2013) CMV serostatus still has an important prognostic impact in de novo acute leukemia patients after allogeneic stem cell transplantation: a report from the Acute Leukemia Working Party of EBMT. Blood 122(19):3359–3364. https://doi.org/10.1182/blood-2013-05-499830
Jang JE, Hyun SY, Kim YD, Yoon SH, Hwang DY, Kim SJ, Kim Y, Kim JS, Cheong JW, Min YH (2012) Risk factors for progression from cytomegalovirus viremia to cytomegalovirus disease after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 18(6):881–886. https://doi.org/10.1016/j.bbmt.2011.10.037
Marty FM, Winston DJ, Rowley SD, Vance E, Papanicolaou GA, Mullane KM, Brundage TM, Robertson AT, Godkin S, Momméja-Marin H, Boeckh M (2013) CMX001 to prevent cytomegalovirus disease in hematopoietic-cell transplantation. N Engl J Med 369(13):1227–1236. https://doi.org/10.1056/NEJMoa1303688
Chemaly RF, Ullmann AJ, Stoelben S, Richard MP, Bornhäuser M, Groth C, Einsele H, Silverman M, Mullane KM, Brown J, Nowak H, Kölling K, Stobernack HP, Lischka P, Zimmermann H, Rübsamen-Schaeff H, Champlin RE, Ehninger G (2014) Letermovir for cytomegalovirus prophylaxis in hematopoietic-cell transplantation. N Engl J Med 370(19):1781–1789. https://doi.org/10.1056/NEJMoa1309533
Green ML, Leisenring W, Xie H, Mast TC, Cui Y, Sandmaier BM, Sorror ML, Goyal S, Özkök S, Yi J, Sahoo F, Kimball LE, Jerome KR, Marks MA, Boeckh M (2016) Cytomegalovirus viral load and mortality after haemopoietic stem cell transplantation in the era of pre-emptive therapy: a retrospective cohort study. Lancet Haematol 3(3):27–e127. https://doi.org/10.1016/S2352-3026(15)00289-6
Marty FM, Ljungman P, Chemaly RF, Maertens J, Dadwal SS, Duarte RF, Haider S, Ullmann AJ, Katayama Y, Brown J, Mullane KM, Boeckh M, Blumberg EA, Einsele H, Snydman DR, Kanda Y, DiNubile MJ, Teal VL, Wan H, Murata Y, Kartsonis NA, Leavitt RY, Badshah C (2017) Letermovir prophylaxis for cytomegalovirus in hematopoietic-cell transplantation. N Engl J Med 377(25):2433–2444. https://doi.org/10.1056/NEJMoa1706640
Broers AE, van der Holt R, van Esser JW, Gratama JW, Henzen-Logmans S, Kuenen-Boumeester V, Löwenberg B, Cornelissen JJ (2000) Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation. Blood 95(7):2240–2245
Kröger N, Zabelina T, Krüger W, Renges H, Stute N, Schrum J, Kabisch H, Schafhausen P, Jaburg N, Löliger C, Schäfer P, Hinke A, Zander AR (2001) Patient cytomegalovirus seropositivity with or without reactivation is the most important prognostic factor for survival and treatment-related mortality in stem cell transplantation from unrelated donors using pretransplant in vivo T-cell depletion with anti-thymocyte globulin. Br J Haematol 113(4):1060–1071
Nichols WG, Corey L, Gooley T, Davis C, Boeckh M (2002) High risk of death due to bacterial and fungal infection among cytomegalovirus (CMV)-seronegative recipients of stem cell transplants from seropositive donors: evidence for indirect effects of primary CMV infection. J Infect Dis 185(3):273–282. https://doi.org/10.1086/338624
Yong MK, Ananda-Rajah M, Cameron PU, Morrissey CO, Spencer A, Ritchie D, Cheng AC, Lewin SR, Slavin M (2017) Cytomegalovirus reactivation is associated with increased risk of late-onset invasive fungal disease after allogeneic hematopoietic stem cell transplantation: a multicenter study in the current era of viral load monitoring. Biol Blood Marrow Transplant 23(11):1961–1967. https://doi.org/10.1016/j.bbmt.2017.07.025
Lönnqvist B, Ringdèn O, Ljungman P, Wahren B, Gahrton G (1986) Reduced risk of recurrent leukaemia in bone marrow transplant recipients after cytomegalovirus infection. Br J Haematol 63(4):671–679
Elmaagacli AH, Steckel NK, Koldehoff M, Hegerfeldt Y, Trenschel R, Ditschkowski M, Christoph S, Gromke T, Kordelas L, Ottinger HD, Ross RS, Horn PA, Schnittger S, Beelen DW (2011) Early human cytomegalovirus replication after transplantation is associated with a decreased relapse risk: evidence for a putative virus-versus-leukemia effect in acute myeloid leukemia patients. Blood 118(5):1402–1412. https://doi.org/10.1182/blood-2010-08-304121
Green ML, Leisenring WM, Xie H, Walter RB, Mielcarek M, Sandmaier BM, Riddell SR, Boeckh M (2013) CMV reactivation after allogeneic HCT and relapse risk: evidence for early protection in acute myeloid leukemia. Blood 122(7):1316–1324. https://doi.org/10.1182/blood-2013-02-487074
George B, Pati N, Gilroy N, Ratnamohan M, Huang G, Kerridge I, Hertzberg M, Gottlieb D, Bradstock K (2010) Pre-transplant cytomegalovirus (CMV) serostatus remains the most important determinant of CMV reactivation after allogeneic hematopoietic stem cell transplantation in the era of surveillance and preemptive therapy. Transpl Infect Dis 12(4):322–329. https://doi.org/10.1111/j.1399-3062.2010.00504.x
Ljungman P (2013) CMV: a warrior against leukemia? Blood 122(7):1101–1102. https://doi.org/10.1182/blood-2013-06-508515
Teira P, Battiwalla M, Ramanathan M, Barrett AJ, Ahn KW, Chen M, Green JS, Saad A, Antin JH, Savani BN, Lazarus HM, Seftel M, Saber W, Marks D, Aljurf M, Norkin M, Wingard JR, Lindemans CA, Boeckh M, Riches ML, Auletta JJ (2016) Early cytomegalovirus reactivation remains associated with increased transplant-related mortality in the current era: a CIBMTR analysis. Blood 127(20):2427–2438. https://doi.org/10.1182/blood-2015-11-679639
Koldehoff M, Ross SR, Dührsen U, Beelen DW, Elmaagacli AH (2017) Early CMV-replication after allogeneic stem cell transplantation is associated with a reduced relapse risk in lymphoma. Leuk Lymphoma 58(4):822–833. https://doi.org/10.1080/10428194.2016.1217524
Albano MS, Taylor P, Pass RF, Scaradavou A, Ciubotariu R, Carrier C, Dobrila L, Rubinstein P, Stevens CE (2006) Umbilical cord blood transplantation and cytomegalovirus: posttransplantation infection and donor screening. Blood 108(13):4275–4282. https://doi.org/10.1182/blood-2006-04-020313
Mikulska M, Raiola AM, Bruzzi P, Varaldo R, Annunziata S, Lamparelli T, Frassoni F, Tedone E, Galano B, Bacigalupo A, Viscoli C (2012) CMV infection after transplant from cord blood compared to other alternative donors: the importance of donor-negative CMV serostatus. Biol Blood Marrow Transplant 18(1):92–99. https://doi.org/10.1016/j.bbmt.2011.05.015
Auner HW, Szydlo R, van Biezen A, Iacobelli S, Gahrton G, Milpied N, Volin L, Janssen J, Nguyen Quoc S, Michallet M, Schoemans H, El Cheikh J, Petersen E, Guilhot F, Schönland S, Ahlberg L, Morris C, Garderet L, de Witte T, Kröger N (2013) Reduced intensity-conditioned allogeneic stem cell transplantation for multiple myeloma relapsing or progressing after autologous transplantation: a study by the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant 48(11):1395–1400. https://doi.org/10.1038/bmt.2013.73
Stern M, de Wreede LC, Brand R, van Biezen A, Dreger P, Mohty M, de Witte TM, Kröger N, Ruutu T (2014) Sensitivity of hematological malignancies to graft-versus-host effects: an EBMT megafile analysis. Leukemia 28(11):2235–2240. https://doi.org/10.1038/leu.2014.145
Robinson SP, Boumendil A, Finel H, Schouten H, Ehninger G, Maertens J, Crawley C, Rambaldi A, Russell N, Anders W, Blaise D, Yakoub-Agha I, Ganser A, Castagna L, Volin L, Cahn JY, Montoto S, Dreger P (2016) Reduced intensity allogeneic stem cell transplantation for follicular lymphoma relapsing after an autologous transplant achieves durable long term disease control: an analysis from the Lymphoma Working Party of the EBMT. Ann Oncol 27:1088–1094. https://doi.org/10.1093/annonc/mdw124
Martino R, Henseler A, van Lint M, Schaap N, Finke J, Beelen D, Vigouroux S, Alessandrino EP, Mufti GJ, Veelken JH, Bruno B, Yakoub-Agha I, Volin L, Maertens J, Or R, Leblond V, Rovira M, Kalhs P, Alvarez AF, Vitek A, Sierra J, Wagner E, Robin M, de Witte T, Kröger N (2017) Long-term follow-up of a retrospective comparison of reduced-intensity conditioning and conventional high-dose conditioning for allogeneic transplantation from matched related donors in myelodysplastic syndromes. Bone Marrow Transplant 52(8):1107–1112. https://doi.org/10.1038/bmt.2017.19
Sullivan KM (1999) Graft-versus-host-disease. In: Thomas E, Blume K, Forman SJ (eds) Hematopoietic Cell Transplantation, 2nd edn. Blackwell Science, Boston, MA, pp 515–526
Ljungman P (2014) The role of cytomegalovirus serostatus on outcome of hematopoietic stem cell transplantation. Curr Opin Hematol 21(6):466–469. https://doi.org/10.1097/MOH.0000000000000085
Ljungman P, Brand R, Hoek J, de La CR, Cordonnier C, Einsele H, Styczynski J, Ward KN, Cesaro S (2014) Donor cytomegalovirus status influences the outcome of allogeneic stem cell transplant: a study by the European group for blood and marrow transplantation. Clin Infect Dis 59(4):473–481. https://doi.org/10.1093/cid/ciu364
Ljungman P, Brandan R (2007) Factors influencing cytomegalovirus seropositivity in stem cell transplant patients and donors. Haematologica 92(8):1139–1142
Bacigalupo A, Socié G, Hamladji RM, Aljurf M, Maschan A, Kyrcz-Krzemien S, Cybicka A, Sengelov H, Unal A, Beelen D, Locasciulli A, Dufour C, Passweg JR, Oneto R, Signori A, Marsh JCW (2015) Current outcome of HLA identical sibling versus unrelated donor transplants in severe aplastic anemia: an EBMT analysis. Haematologica 100(5):696–702. https://doi.org/10.3324/haematol.2014.115345
Nishihori T, Shaheen M, El-Asmar J, Aljurf M, Kharfan-Dabaja MA (2015) Therapeutic strategies for cytomegalovirus in allogeneic hematopoietic cell transplantation. Immunotherapy 7(10):1059–1071. https://doi.org/10.2217/imt.15.70
Maffini E, Giaccone L, Festuccia M, Brunello L, Busca A, Bruno B (2016) Treatment of CMV infection after allogeneic hematopoietic stem cell transplantation. Expert Rev Hematol 9(6):585–596. https://doi.org/10.1080/17474086.2016.1174571
Gor D, Sabin C, Prentice HG, Vyas N, Man S, Griffiths PD, Emery VC (1998) Longitudinal fluctuations in cytomegalovirus load in bone marrow transplant patients: relationship between peak virus load, donor/recipient serostatus, acute GVHD and CMV disease. Bone Marrow Transplant 21(6):597–605. https://doi.org/10.1038/sj.bmt.1701139
Ganepola S, Gentilini C, Hilbers U, Lange T, Rieger K, Hofmann J, Maier M, Liebert UG, Niederwieser D, Engelmann E, Heilbronn R, Thiel E, Uharek L (2007) Patients at high risk for CMV infection and disease show delayed CD8+ T-cell immune recovery after allogeneic stem cell transplantation. Bone Marrow Transplant 39:293–299
van der Heiden PLJ, van Egmond HM, Veld SAJ, van de Meent M, Eefting M, de Wreede LC, Halkes CJM, Falkenburg JHF, Marijt WAF, Jedema I (2018) CMV seronegative donors: effect on clinical severity of CMV infection and reconstitution of CMV-specific immunity. Transpl Immunol 49:54–58. https://doi.org/10.1016/j.trim.2018.04.003
Verduyn Lunel FM, Raymakers R, van Dijk A, van der Wagen L, Minnema MC, Kuball J (2016) Cytomegalovirus status and the outcome of T cell-replete reduced-intensity allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 22(10):1883–1887. https://doi.org/10.1016/j.bbmt.2016.07.009
Ringdén O, Paulin T, Lönnqvist B, Nilsson B (1985) An analysis of factors predisposing to chronic graft-versus-host disease. Exp Hematol 13(10):1062–1067
Miller W, Flynn P, McCullough J, Balfour HH, Goldman A, Haake R, McGlave P, Ramsay N, Kersey J (1986) Cytomegalovirus infection after bone marrow transplantation: an association with acute graft-v-host disease. Blood 67(4):1162–1167
Boeckh M, Nichols WG (2004) The impact of cytomegalovirus serostatus of donor and recipient before hematopoietic stem cell transplantation in the era of antiviral prophylaxis and preemptive therapy. Blood 103(6):2003–2008. https://doi.org/10.1182/blood-2003-10-3616
Yakoub-Agha I, Mesnil F, Kuentz M, Boiron JM, Ifrah N, Milpied N, Chehata S, Esperou H, Vernant JP, Michallet M, Buzyn A, Gratecos N, Cahn JY, Bourhis JH, Chir Z, Raffoux C, Socié G, Golmard JL, Jouet JP (2006) Allogeneic marrow stem-cell transplantation from human leukocyte antigen-identical siblings versus human leukocyte antigen-allelic-matched unrelated donors (10/10) in patients with standard-risk hematologic malignancy: a prospective study from the French Society of Bone Marrow Transplantation and Cell Therapy. J Clin Oncol 24(36):5695–5702. https://doi.org/10.1200/JCO.2006.08.0952
Hahn T, McCarthy PL, Zhang M-J, Wang D, Arora M, Frangoul H, Gale RP, Hale GA, Horan J, Isola L, Maziarz RT, van Rood JJ, Gupta V, Halter J, Reddy V, Tiberghien P, Litzow M, Anasetti C, Pavletic S, Ringdén O (2008) Risk factors for acute graft-versus-host disease after human leukocyte antigen-identical sibling transplants for adults with leukemia. J Clin Oncol 26(35):5728–5734. https://doi.org/10.1200/JCO.2008.17.6545
Author information
Authors and Affiliations
Contributions
M.S.H., G.T., P.L., M.Mik., and J.S. designed the research. M.S.H., G.T., P.L., M.Mik., N.K., D.B., G.S., L.V., N.B., N.F., I.Y.A., E.F., J.M, P.C., J.P., J.C., N.R., C.C., J.H.B., T.M., P.R., J.Y.C., M.Mic., S.M., N.K., B.G., and J.S. provided important clinical data and/or performed statistical analyses. M.S.H. wrote the first draft of the manuscript. All authors approved the final version of the manuscript. A complete list of contributors appears in the online data supplement.
The authors thank all allogeneic transplantation centers of the European Bone Marrow Transplantation group for reporting the data to this registry.
Corresponding author
Ethics declarations
Conflict of interest
I.Y.A received honorarium from Biotest and MSD Sharp & Dohme GmbH that commercialize anti-CMV drugs. The other authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
According to EBMT policy, patients give informed consent for data reporting to the EBMT registry.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 44.8kb)
Rights and permissions
About this article
Cite this article
Schmidt-Hieber, M., Tridello, G., Ljungman, P. et al. The prognostic impact of the cytomegalovirus serostatus in patients with chronic hematological malignancies after allogeneic hematopoietic stem cell transplantation: a report from the Infectious Diseases Working Party of EBMT. Ann Hematol 98, 1755–1763 (2019). https://doi.org/10.1007/s00277-019-03669-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03669-z