Abstract
Purpose
The goal of this study is to characterize the normal size of parotid lymph nodes among healthy adult patients on CT.
Methods
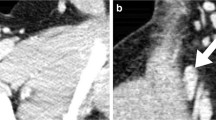
This was a single-center retrospective observational study of 543 patients who underwent maxillofacial CT scans between January 2019 and July 2019. The long and short axis diameters of the largest lymph nodes in the bilateral superficial parotid glands were measured.
Results
Among the 543 patients, 407 subjects with a mean age of 47.0 ± 18.4 years had a total of 719 detectable intraparotid lymph nodes. The mean patient age was 47.0 ± 18.4 years. Of all 719 measured intraparotid lymph nodes, the measured long and short axis diameter means were 4.4 ± 1.4 mm and 3.3 ± 1.1 mm, respectively. In our study, 96% (689/719) of all lymph nodes had a long axis diameter of 7 mm or less and 93% (671/719) of all lymph nodes had a short axis diameter of 5 mm or less. Younger patients had significantly larger lymph nodes than older patients in both long axis (4.5 vs 4.3 mm; P = 0.03) and short axis (3.4 vs 3.1 mm, P = 0.01) measurements.
Conclusion
Our findings suggest 5 mm as an upper limit of normal for the short axis diameter of superficial intraparotid lymph nodes.


Similar content being viewed by others
References
Ch'ng S, Maitra A, Lea R, Brasch H, Tan ST (2006) Parotid metastasis–an independent prognostic factor for head and neck cutaneous squamous cell carcinoma. J Plastic Reconstr Aesthe Surg JPRAS 59:1288–1293. https://doi.org/10.1016/j.bjps.2006.03.043
Ganeshalingam S, Koh D-M (2009) Nodal staging. Cancer Imaging 9:104–111. https://doi.org/10.1102/1470-7330.2009.0017
Garatea-Crelgo J, Gay-Escoda C, Bermejo B, Buenechea-Imaz R (1993) Morphological study of the parotid lymph nodes. J Cranio-Maxillo-fac Surg Off Publ Eur Assoc Cranio-Maxillo-fac Surg 21:207–209
Glazer GM, Gross BH, Quint LE, Francis IR, Bookstein FL, Orringer MB (1985) Normal mediastinal lymph nodes: number and size according to American Thoracic Society mapping. AJR Am J Roentgenol 144:261–265. https://doi.org/10.2214/ajr.144.2.261
Grimm LJ, Viradia NK, Johnson KS (2018) Normal axillary lymph node variability between white and black women on breast MRI. Acad Radiol 25:305–308. https://doi.org/10.1016/j.acra.2017.10.007
Harada H, Omura K (2009) Metastasis of oral cancer to the parotid node. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol 35:890–894. https://doi.org/10.1016/j.ejso.2008.09.013
Kashiwagi N, Murakami T, Toguchi M, Nakanishi K, Hidaka S, Fukui H, Kimura M, Kitano M, Tomiyama N (2016) Metastases to the parotid nodes: CT and MR imaging findings. Dento Maxillo Facial Radiol 45:20160201. https://doi.org/10.1259/dmfr.20160201
Lan M, Huang Y, Chen C-Y, Han F, Wu S-X, Tian L, Zheng L, Lu T-X (2015) Prognostic value of cervical nodal necrosis in nasopharyngeal carcinoma: analysis of 1800 patients with positive cervical nodal metastasis at MR Imaging. Radiology 276:536–544. https://doi.org/10.1148/radiol.15141251
Niu X, Fang Q, Liu F (2019) Role of intraparotid node metastasis in mucoepidermoid carcinoma of the parotid gland. BMC Cancer 19:417. https://doi.org/10.1186/s12885-019-5637-x
Ogassavara B, Tucunduva Neto RR, de Souza RR, Tucunduva MJ (2016) Ultrasound evaluation of the morphometric patterns of lymph nodes of the head and neck in young and middle-aged individuals. Radiol Bras 49:225–228. https://doi.org/10.1590/0100-3984.2015.0002
Silva CE, Souza LMB, Leung KJ, O’Neill A, Jayender J, Lee TC (2018) Jugulodigastric lymph node size by age on CT in an adult cancer-free population. Clin Imaging 47:30–33. https://doi.org/10.1016/j.clinimag.2017.07.013
Steinkamp HJ, Cornehl M, Hosten N, Pegios W, Vogl T, Felix R (1995) Cervical lymphadenopathy: ratio of long- to short-axis diameter as a predictor of malignancy. Br J Radiol 68:266–270. https://doi.org/10.1259/0007-1285-68-807-266
Thom JJ, Moore EJ, Price DL, Kasperbauer JL, Starkman SJ, Olsen KD (2014) The role of total parotidectomy for metastatic cutaneous squamous cell carcinoma and malignant melanoma. JAMA Otolaryngol Head Neck Surg 140:548–554. https://doi.org/10.1001/jamaoto.2014.352
van den Brekel MW, Castelijns JA, Snow GB (1998) The size of lymph nodes in the neck on sonograms as a radiologic criterion for metastasis: how reliable is it? Am J Neuroradiol 19:695–700
van den Brekel MW, Stel HV, Castelijns JA, Nauta JJ, van der Waal I, Valk J, Meyer CJ, Snow GB (1990) Cervical lymph node metastasis: assessment of radiologic criteria. Radiology 177:379–384. https://doi.org/10.1148/radiology.177.2.2217772
Wang H, Cao C, Luo J, Yi J, Huang X, Zhang S, Wang K, Qu Y, Xiao J, Li S, Gao L, Xu G (2016) High-risk factors of parotid lymph node metastasis in nasopharyngeal carcinoma: a case-control study. Radiat Oncol Lond Engl. https://doi.org/10.1186/s13014-016-0691-x
Wang S, Lou J, Zhang S, Guo L, Wang K, Ge M (2015) Metastasis of nasopharyngeal carcinoma to parotid lymph nodes: a retrospective study. World J Surg Oncol 13:1. https://doi.org/10.1186/1477-7819-13-1
Ying M, Ahuja A (2003) Sonography of neck lymph nodes. Part I: normal lymph nodes. Clin Radiol 58:351–358. https://doi.org/10.1016/S0009-9260(02)00584-6
Ying M, Ahuja A, Brook F (2002) Gray scale and power Doppler sonography of normal cervical lymph nodes: comparison between Chinese and white subjects. J Ultrasound Med 21:59–65. https://doi.org/10.7863/jum.2002.21.1.59
Ying M, Ahuja A, Brook F (2002) Sonographic appearances of cervical lymph nodes: variations by age and sex. J Clin Ultrasound 30:1–11. https://doi.org/10.1002/jcu.10022
Ying M, Ahuja A, Brook F, Brown B, Metreweli C (1996) Sonographic appearance and distribution of normal cervical lymph nodes in a Chinese population. J Ultrasound Med 15:431–436. https://doi.org/10.7863/jum.1996.15.6.431
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
MH Zhang: project development, data collection, data analysis, and manuscript writing. DT Ginat: project development, data analysis, manuscript writing, and revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, M.H., Ginat, D.T. Normative measurements of parotid lymph nodes on CT imaging. Surg Radiol Anat 42, 1109–1112 (2020). https://doi.org/10.1007/s00276-020-02494-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-020-02494-8