Abstract
Background
As the leading cause of mortality for retroperitoneal liposarcoma (RPLS) cases, postoperative recurrence has complicated and unclear risk factors. This study was conducted to explore the correlations between demographic, surgical, and pathological characteristics with local recurrence-free survival (LRFS) for surgical resected RPLS.
Methods
RPLS cases that underwent radical operation were considered to be included in this analysis. LRFS rates were estimated based on the Kaplan–Meier method and were compared between groups by the log-rank test. Cox proportional hazard regression models were constructed to identified the predictors of LRFS. Subsequently, the independent predictors acquired from multivariate analyses were used to construct a nomogram.
Results
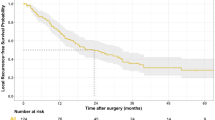
348 RPLS cases who underwent radical operation were included. Of the 348 cases, 333 had tumor recurrence or with a follow-up period ≥5 years. Thus, 296 (88.9%) of the 333 cases had recurrent disease, and the median LRFS duration of 296 recurrence cases was 17.0 (95% confidence interval (CI) 13.2–20.8) months. Multivariate analysis identified the preoperative neutrophil/lymphocyte ratio (NLR), surgical frequency, operative time, tumor shape, histological subtype, and tumor necrosis as independent predictors of LRFS. Based on above independent predictors, a nomogram was constructed to predict the 1-, 3-, and 5-year LRFS of surgical resected RPLS.
Conclusion
Elevated preoperative NLR, ≥2nd time surgical frequency, extended operation time, irregular tumor shape, no well-differentiated histological subtype, and tumor necrosis could be used as predictors of LRFS for surgical resected RPLS.




Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bagaria SP, Gabriel E, Mann GN (2018) Multiply recurrent retroperitoneal liposarcoma. J Surg Oncol 117:62–68
Li Y, Wu G, Zhang Y et al (2022) Development and validation of a prognostic model to predict the prognosis of patients with retroperitoneal liposarcoma: a large international population-based cohort study. Front Oncol 12:857827
Muratori F, Frenos F, Bettini L et al (2018) Liposarcoma: clinico-pathological analysis, prognostic factors and survival in a series of 307 patients treated at a single institution. J Orthop Sci 23:1038–1044
Salerno KE, Baldini EH (2022) Role of radiation therapy in retroperitoneal sarcoma. J Natl Compr Cancer Netw 20:845–849
Molina G, Hull MA, Chen YL et al (2016) Preoperative radiation therapy combined with radical surgical resection is associated with a lower rate of local recurrence when treating unifocal, primary retroperitoneal liposarcoma. J Surg Oncol 114:814–820
Lewis JJ, Leung D, Woodruff JM et al (1998) Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 228:355–365
Neuhaus SJ, Barry P, Clark MA et al (2005) Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 92:246–252
Singer S, Antonescu CR, Riedel E et al (2003) Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg 238:358–371
Xue G, Wang Z, Li C et al (2021) A novel nomogram for predicting local recurrence-free survival after surgical resection for retroperitoneal liposarcoma from a Chinese tertiary cancer center. Int J Clin Oncol 26:145–153
Sánchez-Hidalgo JM, Rufián-Peña S, Durán-Martínez M et al (2018) Risk factors of early recurrence in retroperitoneal liposarcoma. Factores de riesgo implicados en la recurrencia precoz del liposarcoma retroperitoneal. Cir Esp (Engl Ed) 96:568–576
Yan Y, Xia S, Teng D et al (2020) Resection outcomes for primary and local recurrent retroperitoneal liposarcoma patients. Ann Transl Med 8:1450
Sun P, Ma R, Liu G et al (2021) Pathological prognostic factors of retroperitoneal liposarcoma: comprehensive clinicopathological analysis of 124 cases. Ann Transl Med 9:574
Wu YX, Liu JY, Liu JJ et al (2018) A retrospective, single-center cohort study on 65 patients with primary retroperitoneal liposarcoma. Oncol Lett 15:1799–1810
Ishii K, Yokoyama Y, Nishida Y et al (2020) Characteristics of primary and repeated recurrent retroperitoneal liposarcoma: outcomes after aggressive surgeries at a single institution. Jpn J Clin Oncol 50:1412–1418
Gronchi A, Miah AB, Dei Tos AP et al (2021) Soft tissue and visceral sarcomas: ESMO-EURACAN-GENTURIS Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 32:1348–1365
Nassif EF, Cope B, Traweek R et al (2022) Real-world use of palbociclib monotherapy in retroperitoneal liposarcomas at a large volume sarcoma center. Int J Cancer 150:2012–2024
Naszai M, Kurjan A, Maughan TS (2021) The prognostic utility of pre-treatment neutrophil-to-lymphocyte-ratio (NLR) in colorectal cancer: a systematic review and meta-analysis. Cancer Med 10:5983–5997
Zurlo IV, Schino M, Strippoli A et al (2022) Predictive value of NLR, TILs (CD4+/CD8+) and PD-L1 expression for prognosis and response to preoperative chemotherapy in gastric cancer. Cancer Immunol Immunother 71:45–55
Simonaggio A, Elaidi R, Fournier L et al (2020) Variation in neutrophil to lymphocyte ratio (NLR) as predictor of outcomes in metastatic renal cell carcinoma (mRCC) and non-small cell lung cancer (mNSCLC) patients treated with nivolumab. Cancer Immunol Immunother 69:2513–2522
Aloe C, Wang H, Vlahos R et al (2021) Emerging and multifaceted role of neutrophils in lung cancer. Transl Lung Cancer Res 10:2806–2818
Guthrie GJ, Charles KA, Roxburgh CS et al (2013) The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol 88:218–230
Abdelfatah E, Guzzetta AA, Nagarajan N et al (2016) Long-term outcomes in treatment of retroperitoneal sarcomas: a 15 year single-institution evaluation of prognostic features. J Surg Oncol 114:56–64
Homsy P, Blomqvist C, Heiskanen I et al (2020) Multidisciplinary oncovascular surgery is safe and effective in the treatment of intra-abdominal and retroperitoneal sarcomas: a retrospective single centre cohort study and a comprehensive literature review. Eur J Vasc Endovasc Surg 60:752–763
Honoré C, Faron M, Mir O et al (2018) Management of locoregional recurrence after radical resection of a primary nonmetastatic retroperitoneal soft tissue sarcoma: the Gustave Roussy experience. J Surg Oncol 118:1318–1325
Sato T, Yamaguchi T, Azekura K et al (2006) Repeated resection for intra-abdominal and retroperitoneal liposarcomas: long-term experience in a single cancer center in Japan. Int Surg 91:267–271
Masaki N, Onozawa M, Inoue T et al (2021) Clinical features of multiply recurrent retroperitoneal liposarcoma: a single-center experience. Asian J Surg 44:380–385
Suarez-Kelly LP, Baldi GG, Gronchi A (2019) Pharmacotherapy for liposarcoma: current state of the art and emerging systemic treatments. Expert Opin Pharmacother 20:1503–1515
Sbaraglia M, Bellan E, Dei Tos AP (2021) The 2020 WHO classification of soft tissue tumours: news and perspectives. Pathologica 113:70–84
Littau MJ, Kulshrestha S, Bunn C et al (2021) The importance of the margin of resection and radiotherapy in retroperitoneal liposarcoma. Am J Surg 221:554–560
Dehner CA, Hagemann IS, Chrisinger JSA (2021) Retroperitoneal dedifferentiated liposarcoma. Am J Clin Pathol 156:920–925
Xiao J, Liu J, Chen M et al (2021) Diagnosis and prognosis of retroperitoneal liposarcoma: a single Asian center cohort of 57 cases. J Oncol 2021:7594027
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ZY: study design, data curation, data analysis and interpretation, statistical analysis, writing—original draft, writing—review and editing, formal analysis. XZ: data acquisition, supervision, formal analysis, methodology, writing—original draft. JG: data acquisition, quality control of data and algorithms. Data analysis and interpretation. SZ: study design, data curation, statistical analysis, writing—review and editing. NL: data acquisition, data analysis and interpretation, statistical analysis, writing—review and editing. PL: study design, quality control of data and algorithms, data analysis and interpretation, supervision, writing—review and editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the Medical Ethics Committee of the First Medical Center of the Chinese PLA General Hospital and was performed in accordance with the Declaration of Helsinki.
Informed consent
All procedures were performed after obtaining written informed consent from participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Z., Zhao, X., Gao, J. et al. Correlation Analysis Between Demographic, Surgical, and Pathological Characteristics with Local Recurrence-Free Survival for Surgical Resected Retroperitoneal Liposarcoma. World J Surg 47, 1946–1955 (2023). https://doi.org/10.1007/s00268-023-07009-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07009-1