Abstract
Background
Research in early esophageal adenocarcinoma focused on prediction of lymph node metastases in order to stratify patients for endoscopic treatment instead of esophagectomy. Although distant metastases were described in rates of up to 13% of patients within a follow-up of 3 years, their prediction has been neglected so far.
Methods
In a secondary analysis, a cohort of 217 patients (53 T1a and 164 T1b) treated by esophagectomy was analyzed for histopathological risk factors. Their ability to predict the combination of lymph node metastases at surgery as well as metachronous locoregional and distant metastases (overall metastatic rate) was assessed by uni- and multivariate logistic regression analysis.
Results
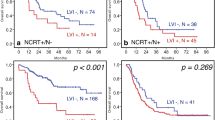
Tumor invasion depth was correlated with both lymph node metastases at surgery (τ = 0.141; P = .012), tumor recurrences (τ = 0.152; P = .014), and distant metastases (τ = 0.122; P = 0.04). Multivariate analysis showed an odds ratio of 1.31 (95% CI 1.02–1.67; P = .033) per increasing tumor invasion depth and of 3.5 (95% CI 1.70–6.56; P < .001) for lymphovascular invasion. The pre-planned subgroup analysis in T1b tumors demonstrated an even lower predictive ability of lymphovascular invasion with an odds ratio of 2.5 (95% CI 1.11–5.65; P = 0.028), whereas the predictive effect of sm2 (odds ratio 3.44; 95% CI 1.00–11.9; P = 0.049) and sm3 (odds ratio 3.44; 95% CI 1.00–11.9; P = 0.049) tumor invasion depth was similar.
Conclusions
The present report demonstrates the insufficient risk prediction of histopathologic risk factors for the overall metastatic rate.

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Thrift AP (2016) The epidemic of oesophageal carcinoma: where are we now? Cancer Epidemiol 41:88–95. https://doi.org/10.1016/j.canep.2016.01.013
Dunbar KB, Spechler SJ (2012) The risk of lymph-node metastases in patients with high-grade dysplasia or intramucosal carcinoma in Barrett’s esophagus: a systematic review. Am J Gastroenterol 107:850–862. https://doi.org/10.1038/ajg.2012.78quiz 863
Westerterp M, Koppert LB, Buskens CJ et al (2005) Outcome of surgical treatment for early adenocarcinoma of the esophagus or gastro-esophageal junction. Virchows Arch Int J Pathol 446:497–504. https://doi.org/10.1007/s00428-005-1243-1
Lorenz D, Origer J, Pauthner M et al (2014) Prognostic risk factors of early esophageal adenocarcinomas. Ann Surg 259:469–476. https://doi.org/10.1097/SLA.0000000000000217
Schölvinck D, Künzli H, Meijer S et al (2016) Management of patients with T1b esophageal adenocarcinoma: a retrospective cohort study on patient management and risk of metastatic disease. Surg Endosc 30:4102–4113. https://doi.org/10.1007/s00464-016-5071-y
Gamboa AM, Kim S, Force SD et al (2016) Treatment allocation in patients with early-stage esophageal adenocarcinoma: prevalence and predictors of lymph node involvement. Cancer 122:2150–2157. https://doi.org/10.1002/cncr.30040
Manner H, Pech O, Heldmann Y et al (2015) The frequency of lymph node metastasis in early-stage adenocarcinoma of the esophagus with incipient submucosal invasion (pT1b sm1) depending on histological risk patterns. Surg Endosc 29:1888–1896. https://doi.org/10.1007/s00464-014-3881-3
Manner H, Wetzka J, May A et al (2017) Early-stage adenocarcinoma of the esophagus with mid to deep submucosal invasion (pT1b sm2-3): the frequency of lymph-node metastasis depends on macroscopic and histological risk patterns: LN metastasis in pT1b sm2-3 EAC. Dis Esophagus 30:1–11. https://doi.org/10.1111/dote.12462
Merkow RP, Bilimoria KY, Keswani RN et al (2014) Treatment trends, risk of lymph node metastasis, and outcomes for localized esophageal cancer. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju133
Chadwick G, Riley S, Hardwick RH et al (2016) Population-based cohort study of the management and survival of patients with early-stage oesophageal adenocarcinoma in England. Br J Surg 103:544–552. https://doi.org/10.1002/bjs.10116
Tian J, Prasad GA, Lutzke LS et al (2011) Outcomes of T1b esophageal adenocarcinoma patients. Gastrointest Endosc 74:1201–1206. https://doi.org/10.1016/j.gie.2011.08.006
Ballard DD, Choksi N, Lin J et al (2016) Outcomes of submucosal (T1b) esophageal adenocarcinomas removed by endoscopic mucosal resection. World J Gastrointest Endosc 8:763. https://doi.org/10.4253/wjge.v8.i20.763
Lee L, Ronellenfitsch U, Hofstetter WL et al (2013) Predicting lymph node metastases in early esophageal adenocarcinoma using a simple scoring system. J Am Coll Surg 217:191–199. https://doi.org/10.1016/j.jamcollsurg.2013.03.015
Davison JM, Landau MS, Luketich JD et al (2016) A model based on pathologic features of superficial esophageal adenocarcinoma complements clinical node staging in determining risk of metastasis to lymph nodes. Clin Gastroenterol Hepatol 14:369–377.e3. https://doi.org/10.1016/j.cgh.2015.10.020
Weksler B, Kennedy KF, Sullivan JL (2017) Using the National Cancer Database to create a scoring system that identifies patients with early-stage esophageal cancer at risk for nodal metastases. J Thorac Cardiovasc Surg 154:1787–1793. https://doi.org/10.1016/j.jtcvs.2017.07.036
Oetzmann von Sochaczewski C, Haist T, Pauthner M et al (2018) The overall metastatic rate in early esophageal adenocarcinoma: long-time follow-up of surgically treated patients. Dis Esophagus. https://doi.org/10.1093/dote/doy127
Japan Esophageal Society (2009) Japanese classification of esophageal cancer, tenth edition: parts II and III. Esophagus 6:71–94. https://doi.org/10.1007/s10388-009-0193-0
Japan Esophageal Society (2017) Japanese classification of esophageal cancer, 11th edition: part II and III. Esophagus 14:37–65. https://doi.org/10.1007/s10388-016-0556-2
Akutsu Y, Uesato M, Shuto K et al (2013) The overall prevalence of metastasis in T1 esophageal squamous cell carcinoma: a retrospective analysis of 295 patients. Ann Surg 257:1032–1038. https://doi.org/10.1097/SLA.0b013e31827017fc
Nobel TB, Barbetta A, Hsu M et al (2019) Ongoing challenges with clinical assessment of nodal status in T1 esophageal adenocarcinoma. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2019.04.032
Kauppi J, Gockel I, Rantanen T et al (2013) Cause of death during long-term follow-up for superficial esophageal adenocarcinoma. Ann Surg Oncol 20:2428–2433. https://doi.org/10.1245/s10434-013-2866-0
Barbour AP, Jones M, Brown I et al (2010) Risk stratification for early esophageal adenocarcinoma: analysis of lymphatic spread and prognostic factors. Ann Surg Oncol 17:2494–2502. https://doi.org/10.1245/s10434-010-1025-0
Nelson DB, Dhupar R, Katkhuda R et al (2018) Outcomes after endoscopic mucosal resection or esophagectomy for submucosal esophageal adenocarcinoma. J Thorac Cardiovasc Surg 156:406–413.e3. https://doi.org/10.1016/j.jtcvs.2018.02.093
Boys JA, Worrell SG, Chandrasoma P et al (2016) Can the risk of lymph node metastases be gauged in endoscopically resected submucosal esophageal adenocarcinomas? A multi-center study. J Gastrointest Surg 20:6–12. https://doi.org/10.1007/s11605-015-2950-9discussion 12
Weber HC, Venzon DJ, Lin JT et al (1995) Determinants of metastatic rate and survival in patients with Zollinger–Ellison syndrome: a prospective long-term study. Gastroenterology 108:1637–1649
Ishihara R, Oyama T, Abe S et al (2016) Risk of metastasis in adenocarcinoma of the esophagus: a multicenter retrospective study in a Japanese population. J Gastroenterol. https://doi.org/10.1007/s00535-016-1275-0
Pech O, May A, Manner H et al (2014) Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology 146:652–660.e1. https://doi.org/10.1053/j.gastro.2013.11.006
Leers JM, DeMeester SR, Oezcelik A et al (2011) The prevalence of lymph node metastases in patients with T1 esophageal adenocarcinoma a retrospective review of esophagectomy specimens. Ann Surg 253:271–278. https://doi.org/10.1097/SLA.0b013e3181fbad42
Hölscher AH, Bollschweiler E, Schröder W et al (2011) Prognostic impact of upper, middle, and lower third mucosal or submucosal infiltration in early esophageal cancer. Ann Surg 254:802–807. https://doi.org/10.1097/SLA.0b013e3182369128discussion 807-808
Newton AD, Predina JD, Xia L et al (2018) Surgical management of early-stage esophageal adenocarcinoma based on lymph node metastasis risk. Ann Surg Oncol 25:318–325. https://doi.org/10.1245/s10434-017-6238-z
Gertler R, Stein HJ, Schuster T et al (2014) Prevalence and topography of lymph node metastases in early esophageal and gastric cancer. Ann Surg 259:96–101. https://doi.org/10.1097/SLA.0000000000000239
Emi M, Hihara J, Hamai Y et al (2017) Clinicopathologic features of submucosal esophageal squamous cell carcinoma. Ann Thorac Surg 104:1858–1864. https://doi.org/10.1016/j.athoracsur.2017.06.037
Kadota T, Yano T, Fujita T et al (2017) Submucosal invasive depth predicts lymph node metastasis and poor prognosis in submucosal invasive esophageal squamous cell carcinoma. Am J Clin Pathol 148:416–426. https://doi.org/10.1093/ajcp/aqx093
Miyata H, Sugimura K, Motoori M et al (2019) Clinical features of metastasis from superficial squamous cell carcinoma of the thoracic esophagus. Surgery. https://doi.org/10.1016/j.surg.2019.07.022
Stein HJ, Feith M, Bruecher BLDM et al (2005) Early esophageal cancer: pattern of lymphatic spread and prognostic factors for long-term survival after surgical resection. Ann Surg 242:566–573 discussion 573-575
Bollschweiler E, Baldus SE, Schröder W et al (2006) High rate of lymph-node metastasis in submucosal esophageal squamous-cell carcinomas and adenocarcinomas. Endoscopy 38:149–156. https://doi.org/10.1055/s-2006-924993
Ma DW, Jung DH, Kim J-H et al (2019) Predicting lymph node metastasis for endoscopic resection of superficial esophageal squamous cell carcinoma. J Thorac Cardiovasc Surg 157:397–402.e1. https://doi.org/10.1016/j.jtcvs.2018.07.034
Suzuki L, ten Kate FJC, Gotink AW et al (2019) Olfactomedin 4 (OLFM4) expression is associated with nodal metastases in esophageal adenocarcinoma. PLoS ONE 14:e0219494. https://doi.org/10.1371/journal.pone.0219494
Gu J, Zhang J, Zheng L et al (2018) Serum miR-331-3p predicts tumor recurrence in esophageal adenocarcinoma. Sci Rep 8:14006. https://doi.org/10.1038/s41598-018-32282-9
Frankell AM, Jammula S, Li X et al (2019) The landscape of selection in 551 esophageal adenocarcinomas defines genomic biomarkers for the clinic. Nat Genet 51:506–516. https://doi.org/10.1038/s41588-018-0331-5
Acknowledgements
The authors thank Alexander Traut, Klinikum Essen-Mitte, Essen, Germany, for his assistance in statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Statement of human rights
The present research was approved by the Medical Council of the State of Hessen (permit no. 48 of 99).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The basis for the present study was laid during the mutual time in a joint working group at the Dr.-Horst-Schmidt-Kliniken, a tertiary referral hospital for upper GI-tumors of the city of Wiesbaden.
Rights and permissions
About this article
Cite this article
Oetzmann von Sochaczewski, C., Haist, T., Pauthner, M. et al. Infiltration Depth is the Most Relevant Risk Factor for Overall Metastases in Early Esophageal Adenocarcinoma. World J Surg 44, 1192–1199 (2020). https://doi.org/10.1007/s00268-019-05291-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05291-6