Abstract
Background
The consequences of lymphadenectomy (LND) on cirrhotic patients undergoing hepatectomy for intrahepatic cholangiocarcinoma (ICC) have not been investigated. We sought to analyze the impact of LND on morbidity among patients undergoing resection for ICC.
Methods
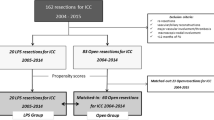
A total of 1005 patients who underwent hepatectomy for ICC at one of the 14 participating institutions between 1990 and 2015 were identified. A propensity score match analysis was performed to reduce confounding biases between cirrhosis and non-cirrhosis groups.
Results
Cirrhosis was diagnosed in 118 (11.7%) patients. Among non-cirrhotic patients, 63% underwent major liver resection versus only 20% among patients with cirrhosis (p < 0.001). LND was also less common among cirrhotic versus non-cirrhotic patients (19 vs. 50%, p < 0.001). The incidence of complications was 41 and 30% among patients who did not and did have cirrhosis, respectively (p = 0.022). The propensity-matched cohort included 150 patients. The incidence of complications was 71% among patients who underwent lymphadenectomy versus 23% among patients who did not undergo lymphadenectomy (OR 8.39) (p < 0.001). In the propensity-matched analysis, the median HLN was comparable among patients independent of cirrhosis status (median HLN: non-cirrhosis, 2.5 vs. cirrhosis, 2) (p = 0.95). While lymphadenectomy was associated with a higher risk of infections (non-cirrhosis, 0% vs. cirrhosis, 21%, p < 0.001) among patients with cirrhosis, infections were not associated with lymphadenectomy among non-cirrhotic patients (p = 0.19).
Conclusion
Lymphadenectomy was associated with an increased risk of complications among patients with cirrhosis undergoing surgery for ICC. The benefit of lymphadenectomy in cirrhotic patients should be considered in light of the higher risk of postoperative complications compared with non-cirrhotic patients.


Similar content being viewed by others
References
Plentz RR, Malek NP (2015) Clinical presentation, risk factors and staging systems of cholangiocarcinoma. Best Pract Res Clin Gastroenterol 29:245–252
Shin HR, Oh JK, Masuyer E et al (2010) Epidemiology of cholangiocarcinoma: an update focusing on risk factors. Cancer Sci 101:579–585
Chan-On W, Kuwahara K, Kobayashi N et al (2009) Cholangiocarcinomas associated with long-term inflammation express the activation-induced cytidine deaminase and germinal center-associated nuclear protein involved in immunoglobulin V-region diversification. Int J Oncol 35:287–295
Goral V (2017) Cholangiocarcinoma: new insights. Asian Pac J Cancer Prev 18:1469–1473
Thinkhamrop K, Khuntikeo N, Phonjitt P et al (2015) Association between diabetes mellitus and fatty liver based on ultrasonography screening in the world’s highest cholangiocarcinoma incidence region, Northeast Thailand. Asian Pac J Cancer Prev 16:3931–3936
Zhang H, Yang T, Wu M et al (2016) Intrahepatic cholangiocarcinoma: epidemiology, risk factors, diagnosis and surgical management. Cancer Lett 379:198–205
Welzel TM, Graubard BI, El-Serag HB et al (2007) Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case-control study. Clin Gastroenterol Hepatol 5:1221–1228
Shaib YH, Davila JA, McGlynn K et al (2004) Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? J Hepatol 40:472–477
Peng NF, Li LQ, Qin X et al (2011) Evaluation of risk factors and clinicopathologic features for intrahepatic cholangiocarcinoma in Southern China: a possible role of hepatitis B virus. Ann Surg Oncol 18:1258–1266
Michelotti GA, Machado MV, Diehl AM (2013) NAFLD NASH and liver cancer. Nat Rev Gastroenterol Hepatol 10:656–665
Cauchy F, Fuks D, Zarzavadjian Le Bian A et al (2014) Metabolic syndrome and non-alcoholic fatty liver disease in liver surgery: the new scourges? World J Hepatol 6:306–314
Shaib YH, El-Serag HB, Davila JA et al (2005) Risk factors of intrahepatic cholangiocarcinoma in the United States: a case-control study. Gastroenterology 128:620–626
Amin MB, American Joint Committee on Cancer (2017) AJCC cancer staging manual Chicago, American Joint Committee on Cancer, Springer
Bagante F, Spolverato G, Weiss M et al. (2018) Assessment of the lymph node status in patients undergoing liver resection for intrahepatic cholangiocarcinoma: the new eighth edition AJCC staging system. J Gastrointest Surg 22(1):52–59
Lee JH, Kim J, Cheong JH et al (2005) Gastric cancer surgery in cirrhotic patients: result of gastrectomy with D2 lymph node dissection. World J Gastroenterol 11:4623–4627
Tachibana M, Kotoh T, Kinugasa S et al (2000) Esophageal cancer with cirrhosis of the liver: results of esophagectomy in 18 consecutive patients. Ann Surg Oncol 7:758–763
Hackl C, Schlitt HJ, Renner P et al (2016) Liver surgery in cirrhosis and portal hypertension. World J Gastroenterol 22:2725–2735
Austin PC, Grootendorst P, Anderson GM (2007) A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med 26:734–753
El-Serag HB (2011) Hepatocellular carcinoma. N Engl J Med 365:1118–1127
Scaglione S, Kliethermes S, Cao G et al (2015) The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol 49:690–696
Affo S, Yu LX, Schwabe RF (2017) The role of cancer-associated fibroblasts and fibrosis in liver cancer. Annu Rev Pathol 12:153–186
Vijgen S, Terris B, Rubbia-Brandt L (2017) Pathology of intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr 6:22–34
Tyson GL, El-Serag HB (2011) Risk factors for cholangiocarcinoma. Hepatology 54:173–184
Jeong S, Cheng Q, Huang L et al (2017) Risk stratification system to predict recurrence of intrahepatic cholangiocarcinoma after hepatic resection. BMC Cancer 17:464
Wang Y, Li J, Xia Y et al (2013) Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol 31:1188–1195
Ali SM, Clark CJ, Mounajjed T et al (2015) Model to predict survival after surgical resection of intrahepatic cholangiocarcinoma: the Mayo Clinic experience. HPB (Oxford) 17:244–250
Doussot A, Lim C, Gomez Gavara C et al (2016) Multicentre study of the impact of morbidity on long-term survival following hepatectomy for intrahepatic cholangiocarcinoma. Br J Surg 103:1887–1894
Doussot A, Gonen M, Wiggers JK et al (2016) Recurrence patterns and disease-free survival after resection of intrahepatic cholangiocarcinoma: preoperative and postoperative prognostic models. J Am Coll Surg 223:493–505
Kim Y, Moris DP, Zhang XF et al. (2017) Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: a surveillance, epidemiology, and end results (SEER) analysis. J Surg Oncol 116(6):643–650
Bagante F, Gani F, Spolverato G et al (2015) Intrahepatic cholangiocarcinoma: prognosis of patients who did not undergo lymphadenectomy. J Am Coll Surg 221:e1031–e1034
Kim Y, Spolverato G, Amini N et al (2015) Surgical management of intrahepatic cholangiocarcinoma: defining an optimal prognostic lymph node stratification schema. Ann Surg Oncol 22:2772–2778
Zhang XF, Chakedis J, Bagante F et al (accepted) Trends in utilization of lymphadenectomy in curative-intent surgery for intrahepatic cholangiocarcinoma. Brit J Surg
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bagante, F., Spolverato, G., Weiss, M. et al. Surgical Management of Intrahepatic Cholangiocarcinoma in Patients with Cirrhosis: Impact of Lymphadenectomy on Peri-Operative Outcomes. World J Surg 42, 2551–2560 (2018). https://doi.org/10.1007/s00268-017-4453-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4453-1