Abstract
Background
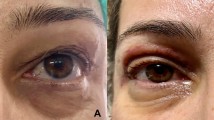
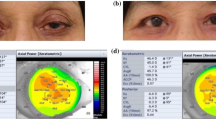
The aim of this study was to assess the effect of different grades of dermatochalasis (DC) and upper eyelid blepharoplasty (UEB) surgery on corneal epithelial thickness (CET), objectively using anterior segment-optical coherence tomography (AS-OCT) measurements.
Methods
90 eyes of patients with DC were divided into three groups according to the severity of the DC. Forty-one eyes of age and sex-matched patients without DC were randomly selected as the control group. The study did not include patients with more than 2 D of spherical refractive error and more than 1.5 D of astigmatism, a history of previous eyelid surgery, ocular surface disease, contact lens use, and ophthalmic eye drop use. CET measurements of all the patients were performed with an AS-OCT (RTVue-XR, Optovue Inc., USA).
Results
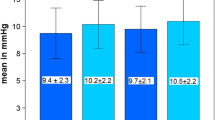
There were statistically significant differences in the CET of the superior, superonasal, superotemporal, inferotemporal, and temporal sectors between the DC and control groups (p = 0.001, p = 0.02, p = 0.03, p = 0.02, p = 0.04, respectively). While there were no differences in CET among the sectors of the control group, there was a difference in CET among some sectors of the DC group. When the DC group was subdivided by severity, there was no difference between subgroups for CET across all sectors both preoperatively and postoperatively. In the measurements made 6 months after UEB surgery, the CET in all sectors increased statistically significantly compared to those measured in the preoperative period.
Conclusion
This study revealed that DC reshaped the corneal epithelium and UEB surgery restored this remodeling 6 months after surgery.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.


Similar content being viewed by others
References
Dogan E, AkbasKocaoglu F, YalnizAkkaya Z, Elbeyli A, Burcu A, Ornek F (2015) Scheimpflug imaging in dermatochalasis patients before and after upper eyelid blepharoplasty. Semin Ophthalmol 30:193–1966
Kim JW, Lee H, Chang M, Park M, Lee TS, Baek S (2013) What causes increased contras sensitivity and improved functional visual acuity after upper eyelid blepharoplasty? Craniofac Surg 24:1582–1585
Bhattacharjee K, Misra D, Singh M, Deori N (2020) Long-term changes in contrast-sensitivity, corneal topography and higher-order aberrations after upper eyelid blepharoplasty: a prospective interventional study. Indian J Ophthalmol 68:2906–2910
Simon G, Ren Q, Kervick GN, Parel JM (1993) Optics of the corneal epithelium. Refract Corneal Surg 9(1):42–50
Wang J, Fonn D, Simpson TL, Jones L (2002) The measurement of corneal epithelial thickness in response to hypoxia using optical coherence tomography. Am J Ophthalmol 133:315–319
Rocha KM, Perez-Straziota E, Stulting RD, Randleman JB (2013) SD-OCT analysis of regional epithelial thickness profiles in keratoconus, postoperative corneal ectasia, and normal eyes. J Refract Surg 29:173–179
Rattan SA, Anwar DS (2020) Comparison of corneal epithelial thickness profile in dry eye patients, keratoconus suspect, and healthy eyes. Eur J Ophthalmol 30(6):1506–1511
Sin S, Simpson TL (2006) The repeatability of corneal and corneal epithelial thickness measurements using optical coherence tomography. Optom Vis Sci 83(6):360–365
Jacobs LC, Liu F, Bleyen I, Gunn DA, Hofman A, Klaver CC, Uitterlinden AG, Neumann HA, Bataille V, Spector TD, Kayser M, Nijsten T (2014) Intrinsic and extrinsic risk factors for sagging eyelids. JAMA Dermatol 150(8):836–843
Wan K, Yau HT, Cheung SW, Cho P (2021) Corneal thickness changes in myopic children during and after short-term orthokeratology lens wear. Ophthalmic Physiol Opt 41(4):757–767
Abdolalizadeh P, Karimi M, Latifi G, Nouri L, Hashemian MN, Hashemian H, Mehrpour M, Alipour F (2022) Role of different types of contact lenses in epithelial thickness. Eye Contact Lens 48(5):210–216
Cui X, Hong J, Wang F, Deng SX, Yang Y, Zhu X, Wu D, Zhao Y, Xu J (2014) Assessment of corneal epithelial thickness in dry eye patients. Optom Vis Sci 91(12):1446–1454
Dogan AS, Acar M, Kosker M, Arslan N, Gurdal C (2018) Alterations in corneal epithelial thickness in patients with congenital myogenic eyelid ptosis. Int Ophthalmol 38(1):53–57
Reinstein DZ, Archer TJ, Vida RS (2022) Epithelial thickness mapping for corneal refractive surgery. Curr Opin Ophthalmol 33(4):258–268
Kanellopoulos AJ, Asimellis G (2014) In vivo 3-dimension corneal epithelial thickness mapping as an indicator of dry eye: preliminary clinical assessment. Am J Ophthalmol 157(1):63–68
Kobayashi A, Yokogawa H, Sugiyama K (2012) In vivo laser confocal microscopy findings in patients with map-dot-fingerprint (epithelial basement membrane) dystrophy. Clin Ophthalmol 6:1187–1190
Kalas T, Gunn D (2022) Corneal epithelial remodeling as a cause of chalazion-induced hypermetropia. Cornea 41(6):785–788
AltinEkin M, KaradenizUgurlu S (2020) Prospective analysis of visual function changes in patients with dermatochalasis after upper eyelid blepharoplasty. Eur J Ophthalmol 30(5):978–984
Funding
There is no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The ethics committee of our institution approved this study.
Informed Consent
All the patients were given written informed consent before the procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arslan, N., Kocamış, S.İ., Sabur, H. et al. Evaluation of the Effect of Dermatochalasis and Upper Eyelid Blepharoplasty Surgery on Corneal Epithelial Thickness Alterations. Aesth Plast Surg 47, 647–651 (2023). https://doi.org/10.1007/s00266-022-03131-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-03131-y