Abstract
Background
Following a total hip arthroplasty (THA), early hospital re-admission rates of 3–11% are considered as ‘acceptable’ in terms of medical care cost policies. Surprisingly, the impact of re-admissions on mortality has not been priorly portrayed. Therefore, we sought to determine the mortality rate after 90-day re-admissions following a THA in a series of patients from a captive medical care program.
Patients and methods
We prospectively analysed 90-day readmissions of 815 unilateral, elective THA patients operated upon between 2010 and 2014 whose medical care was the one offered by our institution. We stratified our sample into readmitted and non-readmitted cohorts. Through a Cox proportional hazards model, we compared demographic characteristics, clinical comorbidities, surgical outcomes and laboratory values between both groups in order to determine association with early and late mortality.
Results
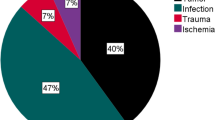
We found 37 (4.53%) re-admissions at a median time of 40.44 days (IQR 17.46–60.69). Factors associated with re-admission were hospital stay (p = 0.00); surgical time (p = 0.01); chronic renal insufficiency (p = 0.03); ASA class 4 (p = 0.00); morbid obesity (p = 0.006); diabetes (p = 0.04) and a high Charlson index (p = 0.00). Overall mortality rate of the series was 3.31% (27/815). Median time to mortality was 455.5 days (IQR 297.58–1170.65). One-third (11/37) of the re-admitted patients died, being sepsis non-related to the THA the most common cause of death. After adjusting for confounders, 90-day re-admissions remained associated with mortality with an adjusted HR of 3.14 (CI95% 1.05–9.36, p = 0.04).
Conclusions
Unplanned re-admissions were an independent risk factor for future mortality, increasing three times the risk of mortality.



Similar content being viewed by others
References
Daigle ME, Weinstein AM, Katz JN, Losina E (2012) The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol 26:649–658. https://doi.org/10.1016/j.berh.2012.07.013
Learmonth ID, Young C, Rorabeck C (2007) The operation of the century: total hip replacement. Lancet 370:1508–1519. https://doi.org/10.1016/S0140-6736(07)60457-7
Clement RC, Derman PB, Graham DS et al (2013) Risk factors, causes, and the economic implications of unplanned readmissions following total hip arthroplasty. J Arthroplast 28:7–10. https://doi.org/10.1016/j.arth.2013.04.055
Kurtz SM, Lau EC, Ong KL et al (2017) Which clinical and patient factors influence the national economic burden of hospital readmissions after total joint arthroplasty? Clin Orthop Relat Res. https://doi.org/10.1007/s11999-017-5244-6
Zmistowski B, Restrepo C, Hess J et al (2013) Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am 95:1869–1876. https://doi.org/10.2106/JBJS.L.00679
de Vries LM, Sturkenboom MCJM, Verhaar JAN et al (2011) Complications after hip arthroplasty and the association with hospital procedure volume. Acta Orthop 82:545–552. https://doi.org/10.3109/17453674.2011.618907
Hackbarth G, Reischauer R, Mutti A (2008) Collective accountability for medical care—toward bundled Medicare payments. N Engl J Med 359:3–5. https://doi.org/10.1056/NEJMp0803749
Mednick RE, Alvi HM, Krishnan V et al (2014) Factors affecting readmission rates following primary total hip arthroplasty. J Bone Jt Surgery-American 96:1201–1209. https://doi.org/10.2106/JBJS.M.00556
Paxton EW, Inacio MCS, Singh JA et al (2015) Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system? Clin Orthop Relat Res 473:3446–3455. https://doi.org/10.1007/s11999-015-4278-x
Schairer WW, Sing DC, Vail TP, Bozic KJ (2014) Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res 472:464–470. https://doi.org/10.1007/s11999-013-3121-5
Navathe AS, Troxel AB, Liao JM et al (2017) Cost of joint replacement using bundled payment models. JAMA Intern Med 79:1–105. https://doi.org/10.1001/jamainternmed.2016.8263
Centers for Medicare & Medicaid Services (CMS) H (2017) Medicare program; advancing care coordination through episode payment models (EPMs); cardiac rehabilitation incentive payment model; and changes to the comprehensive care for joint replacement model (CJR). Final rule. Fed Regist 82:180–651
Stone A V., Jinnah A, Wells BJ, et al. (2017) Nutritional markers may identify patients with greater risk of re-admission after geriatric hip fractures. Int Orthop 1–8. https://doi.org/10.1007/s00264-017-3663-3
Weinberg DS, Kraay MJ, Fitzgerald SJ et al (2016) Are readmissions after THA preventable? Clin Orthop Relat Res. https://doi.org/10.1007/s11999-016-5156-x
Boraiah S, Joo L, Inneh IA et al (2015) Management of modifiable risk factors prior to primary hip and knee arthroplasty: a readmission risk assessment tool. J Bone Jt Surg 97:1921–1928. https://doi.org/10.2106/JBJS.N.01196
Wasfy JH, Zigler CM, Choirat C et al (2016) Readmission rates after passage of the hospital readmissions reduction program. Ann Intern Med 366:1364–1366. https://doi.org/10.7326/M16-0185
Saucedo J, Marecek GS, Lee J et al (2013) How accurately are we coding readmission diagnoses after total joint arthroplasty? J Arthroplast 28:1076–1079. https://doi.org/10.1016/j.arth.2013.05.006
Haynes SR, Lawler PG (1995) An assessment of the consistency of ASA physical status classification allocation. Anaesthesia 50:195–199
Jones CA, Cox V, Jhangri GS, Suarez-Almazor ME (2012) Delineating the impact of obesity and its relationship on recovery after total joint arthroplasties. Osteoarthr Cartil 20:511–518. https://doi.org/10.1016/j.joca.2012.02.637
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619. https://doi.org/10.1016/0895-4356(92)90133-8
Gulotta LV, Padgett DE, Sculco TP et al (2011) Fast track THR: one hospital’s experience with a 2-day length of stay protocol for total hip replacement. HSS J 7:223–228. https://doi.org/10.1007/s11420-011-9207-2
Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT (2016) Hospital, patient, and clinical factors influence 30- and 90-day readmission after primary total hip arthroplasty. J Arthroplasty 31(10):2130–2138. https://doi.org/10.1016/j.arth.2016.03.041
Bliemel C, Buecking B, Oberkircher L et al (2017) The impact of pre-existing conditions on functional outcome and mortality in geriatric hip fracture patients. Int Orthop 41:1995–2000. https://doi.org/10.1007/s00264-017-3591-2
Carow J, Carow JB, Coburn M et al (2017) Mortality and cardiorespiratory complications in trochanteric femoral fractures: a ten year retrospective analysis. Int Orthop 41:2371–2380. https://doi.org/10.1007/s00264-017-3639-3
Wong SHJ, Fang XC, Yee KHD, Wong TM, Pun CTT, Lau TW, Leung KLF (2018) Hip fracture time-to-surgery and mortality revisited: mitigating comorbidity confounding by effect of holidays on surgical timing. Int Orthop. https://doi.org/10.1007/s00264-017-3737-2
Tulic G, Dubljanin-Raspopovic E, Tomanovic-Vujadinovic S et al (2017) Prolonged pre-operative hospital stay as a predictive factor for early outcomes and mortality after geriatric hip fracture surgery: a single institution open prospective cohort study. Int Orthop. https://doi.org/10.1007/s00264-017-3643-7
Jørgensen CC, Kehlet H (2017) Time course and reasons for 90-day mortality in fast-track hip and knee arthroplasty. Acta Anaesthesiol Scand 61:436–444. https://doi.org/10.1111/aas.12860
Calvani R, Marini F, Cesari M et al (2015) Biomarkers for physical frailty and sarcopenia: state of the science and future developments. J Cachexia Sarcopenia Muscle 6:278–286. https://doi.org/10.1002/jcsm.12051
Kim S-W, Han H-S, Jung H-W et al (2014) Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA Surg 149:633–640. https://doi.org/10.1001/jamasurg.2014.241
Wise BL, Parimi N, Zhang Y et al (2014) Frailty and hip osteoarthritis in men in the MrOS cohort. Journals Gerontol - Ser A Biol Sci Med Sci 69(A):602–608. https://doi.org/10.1093/gerona/glt126
Hunt LP, Ben-Shlomo Y, Clark EM et al (2013) 90-day mortality after 409 096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 382:1097–1104. https://doi.org/10.1016/S0140-6736(13)61749-3
Lisenda L, Mokete L, Mkubwa J, Lukhele M (2016) Inpatient mortality after elective primary total hip and knee joint arthroplasty in Botswana. Int Orthop 40:2453–2458. https://doi.org/10.1007/s00264-016-3280-6
Phruetthiphat O-A, Gao Y, Anthony CA et al (2016) Incidence of and preoperative risk factors for surgical delay in primary total hip arthroplasty: analysis from the American College of Surgeons National Surgical Quality Improvement Program. J Arthroplast. https://doi.org/10.1016/j.arth.2016.05.054
Brooke BS, Goodney PP, Kraiss LW et al (2015) Readmission destination and risk after major surgery: an observational cohort study. Lancet 386:884–895. https://doi.org/10.1016/S0140-6736(15)60087-3.Readmission
McIsaac DI, Beaulé PE, Bryson GL, van Walraven C (2016) The impact of frailty on outcomes and healthcare resource usage after total joint arthroplasty: a population-based cohort study. Bone Joint J 98–B:799–805. https://doi.org/10.1302/0301-620X.98B6.37124
Bellamy JL, Runner RP, Vu CCL et al (2017) Modified frailty index is an effective risk assessment tool in primary total hip arthroplasty. J Arthroplast 32:2963–2968. https://doi.org/10.1016/j.arth.2017.04.056
Huddleston JI, Wang Y, Uquillas C et al (2012) Age and obesity are risk factors for adverse events after total hip arthroplasty. Clin Orthop Relat Res 470:490–496. https://doi.org/10.1007/s11999-011-1967-y
Miric A, Inacio MCS, Kelly MP, Namba RS (2015) Are nonagenarians too old for total hip arthroplasty? An evaluation of morbidity and mortality within a total joint replacement registry. J Arthroplast 30:1324–1327. https://doi.org/10.1016/j.arth.2015.03.008
Comba F, Hidalgo IA, Buttaro M, Piccaluga F (2012) Risk factor analysis for 30-day mortality after primary THA in a single institution. HSS J 8:111–115. https://doi.org/10.1007/s11420-012-9279-7
Liu SS, Della Valle AG, Besculides MC et al (2009) Trends in mortality, complications, and demographics for primary hip arthroplasty in the United States. Int Orthop 33:643–651. https://doi.org/10.1007/s00264-008-0549-4
Khan SK, Malviya A, Muller SD et al (2014) Reduced short-term complications and mortality following enhanced recovery primary hip and knee arthroplasty: results from 6,000 consecutive procedures. Acta Orthop 85:26–31. https://doi.org/10.3109/17453674.2013.874925
Malviya A, Martin K, Harper I et al (2011) Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop 82:577–581. https://doi.org/10.3109/17453674.2011.618911
Savaridas T, Serrano-Pedraza I, Khan SK et al (2013) Reduced medium-term mortality following primary total hip and knee arthroplasty with an enhanced recovery program. A study of 4,500 consecutive procedures. Acta Orthop 84:40–43. https://doi.org/10.3109/17453674.2013.771298
Sibia US, Waite KA, Callanan MA et al (2017) Do shorter lengths of stay increase readmissions after total joint replacements? Arthroplast Today 3:51–55. https://doi.org/10.1016/j.artd.2016.05.001
Jans Ø, Jørgensen C, Kehlet H et al (2014) Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion 54:717–726. https://doi.org/10.1111/trf.12332
Pitter FT, Jørgensen CC, Lindberg-Larsen M, Kehlet H (2016) Postoperative morbidity and discharge destinations after fast-track hip and knee arthroplasty in patients older than 85 years. Anesth Analg 122:1807–1815. https://doi.org/10.1213/ANE.0000000000001190
Acknowledgements
The authors have nobody to acknowledge.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Each author certifies that his institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Slullitel, P.A., Estefan, M., Ramírez-Serrudo, W.M. et al. Re-admissions treble the risk of late mortality after primary total hip arthroplasty. International Orthopaedics (SICOT) 42, 2015–2023 (2018). https://doi.org/10.1007/s00264-018-3876-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3876-0