Abstract
Purpose
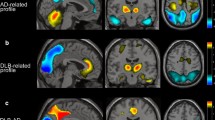
The aim of this study was to verify the reliability and generalizability of an automatic tool for the detection of Alzheimer-related hypometabolic pattern based on a Support-Vector-Machine (SVM) model analyzing 18F-fluorodeoxyglucose (FDG) PET data.
Methods
The SVM model processed metabolic data from anatomical volumes of interest also considering interhemispheric asymmetries. It was trained on a homogeneous dataset from a memory clinic center and tested on an independent multicentric dataset drawn from the Alzheimer’s Disease Neuroimaging Initiative. Subjects were included in the study and classified based on a diagnosis confirmed after an adequate follow-up time.
Results
The accuracy of the discrimination between patients with Alzheimer Disease (AD), in either prodromal or dementia stage, and normal aging subjects was 95.8%, after cross-validation, in the training set. The accuracy of the same model in the testing set was 86.5%. The role of the two datasets was then reversed, and the accuracy was 89.8% in the multicentric training set and 88.0% in the monocentric testing set. The classification rate was also evaluated in different subgroups, including non-converter mild cognitive impairment (MCI) patients, subjects with MCI reverted to normal conditions and subjects with non-confirmed memory concern. The percent of pattern detections increased from 77% in early prodromal AD to 91% in AD dementia, while it was about 10% for healthy controls and non-AD patients.
Conclusions
The present findings show a good level of reproducibility and generalizability of a model for detecting the hypometabolic pattern in AD and confirm the accuracy of FDG-PET in Alzheimer disease.




Similar content being viewed by others
References
Frisoni GB, Bocchetta M, Chételat G, Rabinovici GD, De Leon MJ, Kaye J, et al. Imaging markers for Alzheimer disease: which vs how. Neurology. 2013;81:487–500.
Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–28.
Landau SM, Harvey D, Madison CM, Koeppe RA, Reiman EM, Foster NL, et al. Associations between cognitive, functional, and FDG-PET measures of decline in AD and MCI. Neurobiol Aging. 2011;32:1207–18.
Signorini M, Paulesu E, Friston K, Perani D, Colleluori A, Lucignani G, et al. Rapid assessment of regional cerebral metabolic abnormalities in single subjects with quantitative and nonquantitative [18F]FDG PET: a clinical validation of statistical parametric mapping. NeuroImage. 1999;9:63–80.
Caminiti SP, Ballarini T, Sala A, Cerami C, Presotto L, Santangelo R, et al. FDG-PET and CSF biomarker accuracy in prediction of conversion to different dementias in a large multicentre MCI cohort. NeuroImage Clin. Elsevier. 2018;18:167–77.
Perani D, Della Rosa PA, Cerami C, Gallivanone F, Fallanca F, Vanoli EG, et al. Validation of an optimized SPM procedure for FDG-PET in dementia diagnosis in a clinical setting. NeuroImage Clin [Internet]. Elsevier B.V. 2014;6:445–54. Available from: https://doi.org/10.1016/j.nicl.2014.10.009.
Herholz K, Salmon E, Perani D, Baron JC, Holthoff V, Frölich L, et al. Discrimination between Alzheimer dementia and controls by automated analysis of multicenter FDG PET. NeuroImage. 2002;17:302–16.
Haense C, Herholz K, Jagust WJ, Heiss WD. Performance of FDG PET for detection of Alzheimer’s disease in two independent multicentre samples (NEST-DD and ADNI). Dement Geriatr Cogn Disord. 2009;28:259–66.
Chen K, Ayutyanont N, Langbaum JBS, Fleisher AS, Reschke C, Lee W, et al. Characterizing Alzheimer’s disease using a hypometabolic convergence index. NeuroImage [Internet]. Elsevier Inc. 2011;56:52–60. Available from: https://doi.org/10.1016/j.neuroimage.2011.01.049.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage. 2002;15:273–89.
Pagani M, De Carli F, Morbelli S, Öberg J, Chincarini A, Frisoni GB, et al. Volume of interest-based [18F]fluorodeoxyglucose PET discriminates MCI converting to Alzheimer’s disease from healthy controls. A European Alzheimer’s disease consortium (EADC) study. NeuroImage Clin [Internet]. 2015;7:34–42. Available from: http://europepmc.org/abstract/med/25610765.
Pagani M, Nobili F, Morbelli S, Arnaldi D, Giuliani A, Öberg J, et al. Early identification of MCI converting to AD: a FDG PET study. Eur J Nucl Med Mol Imaging. 2017;44:2042–52.
Smailagic N, Vacante M, Hyde C, Martin S, Ukoumunne O, Sachpekidis C. F-FDG-PET for the early diagnosis of Alzheimer ’ s disease dementia and other dementias in people with mild cognitive impairment ( MCI ) (review). Cochrane Database Syst Rev. 2015:1–104.
Rathore S, Habes M, Iftikhar MA, Shacklett A, Davatzikos C. A review on neuroimaging-based classification studies and associated feature extraction methods for Alzheimer’s disease and its prodromal stages. NeuroImage. Elsevier. 2017;155:530–48.
Morbelli S, Drzezga A, Perneczky R, Frisoni GB, Caroli A, Van Berckel BNM, et al. Resting metabolic connectivity in prodromal Alzheimer’s disease. A European Alzheimer disease consortium (EADC) project. Neurobiol Aging [Internet]. Elsevier Inc. 2012;33:2533–50. Available from: https://doi.org/10.1016/j.neurobiolaging.2012.01.005.
Herholz K. PET studies in dementia. Ann Nucl Med. 2003;17:79–89.
Herholz K, Westwood S, Haense C, Dunn G. Evaluation of a calibrated 18F-FDG PET score as a biomarker for progression in Alzheimer disease and mild cognitive impairment. J Nucl Med [Internet]. 2011;52:1218–26. Available from: http://jnm.snmjournals.org/cgi/doi/10.2967/jnumed.111.090902.
Caroli A, Prestia A, Chen K, Ayutyanont N, Landau SM, Madison CM, et al. Summary metrics to assess Alzheimer disease-related hypometabolic pattern with 18F-FDG PET: head-to-head comparison. J Nucl Med [Internet]. 2012;53:592–600. Available from: http://jnm.snmjournals.org/cgi/doi/10.2967/jnumed.111.094946.
Pagani M, De Carli F, Morbelli S, Öberg J, Chincarini A, Frisoni GB, et al. Volume of interest-based [18F]fluorodeoxyglucose PET discriminates MCI converting to Alzheimer’s disease from healthy controls. A European Alzheimer’s disease consortium (EADC) study. NeuroImage Clin [Internet]. Elsevier B.V. 2015;7:34–42. Available from: https://doi.org/10.1016/j.nicl.2014.11.007.
Pagani M, Giuliani A, Öberg J, De Carli F, Morbelli S, Girtler N, et al. Progressive disintegration of brain networking from Normal aging to Alzheimer disease: analysis of independent components of 18 F-FDG PET data. J Nucl Med [Internet]. 2017;58:1132–9. Available from: http://jnm.snmjournals.org/lookup/doi/10.2967/jnumed.116.184309.
Petersen RC, Negash S. Mild cognitive impairment: an overview. CNS Spectr. 2008;13:45–53.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement [Internet]. Elsevier Ltd. 2011;7:270–9. Available from: https://doi.org/10.1016/j.jalz.2011.03.008.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement [Internet]. Elsevier Ltd. 2011;7:263–9. Available from: https://doi.org/10.1016/j.jalz.2011.03.005.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Någren K, et al. EANM procedure guidelines for PET brain imaging using [18F]FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10.
Della Rosa PA, Cerami C, Gallivanone F, Prestia A, Caroli A, Castiglioni I, et al. A standardized [18F]-FDG-PET template for spatial normalization in statistical parametric mapping of dementia. Neuroinformatics. 2014;12:575–93.
Soonawala D, Amin T, Ebmeier KP, Steele DJ, Dougall NJ, Best J, et al. Statistical parametric mapping of99mTc-HMPAO-SPECT images for the diagnosis of Alzheimer’s disease: normalizing to cerebellar tracer uptake. NeuroImage. 2002;17:1193–202.
Dukart J, Mueller K, Horstmann A, Vogt B, Frisch S, Barthel H, et al. Differential effects of global and cerebellar normalization on detection and differentiation of dementia in FDG-PET studies. Neuroimage. Elsevier Inc. 2010;49:1490–5.
Morbelli S, Brugnolo A, Bossert I, Buschiazzo A, Frisoni GB, Galluzzi S, et al. Visual versus semi-quantitative analysis of18F-FDG-PET in amnestic MCI: an European Alzheimer’s disease consortium (EADC) project. J Alzheimer’s Dis [Internet]. 2015;44:815–26. Available from: http://europepmc.org/abstract/med/25362041.
Zahn R, Juengling F, Bubrowski P, Jost E, Dykierek P, Talazko J, et al. Hemispheric asymmetries of hypometabolism associated with semantic memory impairment in Alzheimer’s disease: a study using positron emission tomography with fluorodeoxyglucose-F18. Psychiatry Res Neuroimaging. 2004;132:159–72.
Brown LD, Cai TT, Dasgupta A. Interval estimation for a binomial. Stat Sci. 2001;16:101–33.
Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol [Internet]. 1991;44:763–70. Available from: http://www.sciencedirect.com/science/article/pii/089543569190128V.
Chen F, Xue Y, Tan MT, Chen P. Efficient statistical tests to compare Youden index: accounting for contingency correlation. Stat Med. 2015;34:1560–76.
Qin G, Hotilovac L. Comparison of non-parametric confidence intervals for the area under the ROC curve of a continuous-scale diagnostic test. Stat Methods Med Res. 2008;17:207–21.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology [Internet]. Radiological Society of North America. 1982;143:29–36. Available from: https://doi.org/10.1148/radiology.143.1.7063747.
Landau SM, Mintun MA, Joshi AD, Koeppe RA, Petersen RC, Aisen PS, et al. Amyloid deposition, hypometabolism, and longitudinal cognitive decline. Ann Neurol [Internet]. 2012;72:578–86. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3786871/.
Cabral C, Morgado PM, Campos Costa D, Silveira M. Predicting conversion from MCI to AD with FDG-PET brain images at different prodromal stages. Comput Biol Med [Internet]. Elsevier. 2015;58:101–9. Available from: https://doi.org/10.1016/j.compbiomed.2015.01.003.
Pagani M, Giuliani A, Öberg J, Chincarini A, Morbelli S, Brugnolo A, et al. Predicting the transition from normal aging to Alzheimer’s disease: a statistical mechanistic evaluation of FDG-PET data. Neuroimage [Internet]. Elsevier Inc. 2016;141:282–90. Available from: https://doi.org/10.1016/j.neuroimage.2016.07.043.
Arnaldi D, Morbelli S, Brugnolo A, Girtler N, Picco A, Ferrara M, et al. Functional neuroimaging and clinical features of drug naive patients with de novo Parkinson’s disease and probable RBD. Parkinsonism Relat Disord. 2016;29:47–53.
Kryscio RJ, Abner EL, Cooper GE, Fardo DW, Jicha GA, Nelson PT, et al. Self-reported memory complaints: implications from a longitudinal cohort with autopsies. Neurology. 2014;83(15):1359-65.
Rasmussen JM, Lakatos A, van Erp TGM, Kruggel F, Keator DB, Fallon JT, et al. Empirical derivation of the reference region for computing diagnostic sensitive18fluorodeoxyglucose ratios in Alzheimer’s disease based on the ADNI sample. Biochim Biophys Acta - Mol Basis Dis [Internet]. Elsevier B.V. 2012;1822:457–66. Available from: https://doi.org/10.1016/j.bbadis.2011.09.008.
Braak H, Braak E, Bohl J, Lang W. Alzheimer’s disease: amyloid plaques in the cerebellum. J Neurol Sci. 1989;93:277–87.
Catafau AM, Bullich S, Seibyl JP, Barthel H, Ghetti B, Leverenz J, et al. Cerebellar amyloid- plaques: how frequent are they, and do they influence 18F-Florbetaben SUV ratios? J Nucl Med [Internet]. 2016;57:1740–5 Available from: http://jnm.snmjournals.org/cgi/doi/10.2967/jnumed.115.171652.
Ishii K, Sasaki M, Kitagaki H, Yamaji S, Sakamoto S, Matsuda K, et al. Reduction of cerebellar glucose metabolism in advanced Alzheimer’s disease. J Nucl Med [Internet]. 1997;38:925–8 Available from: http://jnm.snmjournals.org/content/38/6/925.full.pdf.
Bocchetta M, Cardoso MJ, Cash DM, Ourselin S, Warren JD, Rohrer JD. Patterns of regional cerebellar atrophy in genetic frontotemporal dementia. NeuroImage Clin [Internet]. The Authors. 2016;11:287–90. Available from: https://doi.org/10.1016/j.nicl.2016.02.008.
Bauckneht M, Chincarini A, Piva R, Arnaldi D, Girtler N, Massa F, et al. Metabolic correlates of reserve and resilience in MCI due to Alzheimer’s disease (AD) Rik Ossenkoppele. Alzheimer’s Res Ther Alzheimer’s Research & Therapy. 2018;10:1–13.
Acknowledgements
Data collection and sharing for this project was partly funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research&Development, LLC.; Johnson & Johnson Pharmaceutical Research&Development LLC.; Lumosity; Lundbeck; Merck&Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research provides funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
A substantial part of data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
F.N.: received personal fees and nonfinancial support from GE Healthcare, non-financial support from Eli-Lilly and grants from Chiesi Farmaceutici; D.A. received speaking honoraria from Fidia s.p.a.; S.M. acted as a consultant for Eli Lilly in 2014 and for Avid Radiopharmaceuticals in 2016. All other authors have no potential conflicts to declare.
Ethical approval
The institutional review board of the University of Genoa approved the recording and data treatment procedures involving human participants in this study and all procedures were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
(PDF 440 kb)
Rights and permissions
About this article
Cite this article
De Carli, F., Nobili, F., Pagani, M. et al. Accuracy and generalization capability of an automatic method for the detection of typical brain hypometabolism in prodromal Alzheimer disease. Eur J Nucl Med Mol Imaging 46, 334–347 (2019). https://doi.org/10.1007/s00259-018-4197-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4197-7