Abstract
Purpose
To assess the relationship between regional myocardial perfusion and sympathetic innervation parameters at myocardial scintigraphy and intra-cavitary electrophysiological data in patients with ventricular arrhythmias (VA) submitted to invasive electrophysiological study and ablation procedure.
Methods
Sixteen subjects underwent invasive electrophysiological study with electroanatomical mapping (EAM) followed by trans-catheter ablations of VA. Before ablation all patients were studied with a combined evaluation of regional myocardial perfusion and sympathetic innervation by means of tomographic 99mTc-tetrofosmin and 123I- metaiodobenzylguanidine cadmium-zinc-telluride (CZT) scintigraphies, respectively. Off-line spatial co-registration of CZT perfusion and innervation data with the three-dimensional EAM reconstruction was performed in every patient.
Results
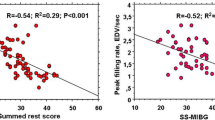
CZT revealed the presence of myocardial scar in 55 (20 %) segments. Of the viable myocardial segments, 131 (60 %) presented a preserved adrenergic innervation, while 86 (40 %) showed a significantly depressed innervation (i.e. innervation/perfusion mismatch). On EAM, the invasively measured intra-cavitary voltage was significantly lower in scarred segments than in viable ones (1.7 ± 1.5 mV vs. 4.0 ± 2.2 mV, P < 0.001). Interestingly, among the viable segments, those showing an innervation/perfusion mismatch presented a significantly lower intra-cavitary voltage than those with preserved innervation (1.9 ± 2.5 mV vs. 4.7 ± 2.3 mV, P < 0.001). Intra-cardiac ablation was performed in 63 (23 %) segments. On multivariate analysis, after correction for scar burden, the segments showing an innervation/perfusion mismatch remained the most frequent ablation targets (OR 5.6, 95 % CI 1.5–20.8; P = 0.009).
Conclusions
In patients with VA, intra-cavitary electrical abnormalities frequently originate at the level of viable myocardial segments with depressed sympathetic innervation that frequently represents the ultimate ablation target.



Similar content being viewed by others
References
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC) Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–867.
Klein T, Dilsizian V, Cao Q, Chen W, Dickfeld TM. The potential role of iodine-123 metaiodobenzylguanidine imaging for identifying sustained ventricular tachycardia in patients with cardiomyopathy. Curr Cardiol Rep. 2013;15:359.
Paul M, Wichter T, Kies P, Gerss J, Wollmann C, Rahbar K, et al. Cardiac sympathetic dysfunction in genotyped patients with arrhythmogenic right ventricular cardiomyopathy and risk of recurrent ventricular tachyarrhythmias. J Nucl Med. 2011;52:1559–65.
Fallavollita JA, Heavey BM, Luisi Jr AJ, Michalek SM, Baldwa S, Mashtare Jr TL, et al. Regional myocardial sympathetic denervation predicts the risk of sudden cardiac arrest in ischemic cardiomyopathy. J Am Coll Cardiol. 2014;63:141–9.
Jacobson AF, Senior R, Cerqueira MD, Wong ND, Thomas GS, Lopez VA, et al. Myocardial iodine-123 meta-iodobenzylguanidine imaging and cardiac events in heart failure. Results of the prospective ADMIRE-HF (AdreView Myocardial Imaging for Risk Evaluation in Heart Failure) study. J Am Coll Cardiol. 2010;55:2212–21.
Dimitriu-Leen AC, Gimelli A, Al Younis I, Veltman CE, Verberne HJ, Wolterbeek R, et al. The impact of acquisition time of planar cardiac (123)I-MIBG imaging on the late heart to mediastinum ratio. Eur J Nucl Med Mol Imaging. 2016;43:326–32.
Clements IP, Garcia EV, Chen J, Folks RD, Butler J, Jacobson AF. Quantitative iodine-123-metaiodobenzylguanidine (MIBG) SPECT imaging in heart failure with left ventricular systolic dysfunction: development and validation of automated procedures in conjunction with technetium-99m tetrofosmin myocardial perfusion SPECT. J Nucl Cardiol. 2016;23:425–35.
Gimelli A, Liga R, Giorgetti A, Genovesi D, Marzullo P. Assessment of myocardial adrenergic innervation with a solid-state dedicated cardiac cadmium-zinc-telluride camera: first clinical experience. Eur Heart J Cardiovasc Imaging. 2014;15:575–85.
Zhou Y, Zhou W, Folks RD, Manatunga DN, Jacobson AF, Garcia EV, et al. I-123 mIBG and Tc-99m myocardial SPECT imaging to predict inducibility of ventricular arrhythmia on electrophysiology testing: a retrospective analysis. J Nucl Cardiol. 2014;21:913–20.
Bax JJ, Kraft O, Buxton AE, Fjeld JG, Parízek P, Agostini D, et al. 123 I-mIBG scintigraphy to predict inducibility of ventricular arrhythmias on cardiac electrophysiology testing: a prospective multicenter pilot study. Circ Cardiovasc Imaging. 2008;1:131–40.
Gimelli A, Liga R, Genovesi D, Giorgetti A, Kusch A, Marzullo P. Association between left ventricular regional sympathetic denervation and mechanical dyssynchrony in phase analysis: a cardiac CZT study. Eur J Nucl Med Mol Imaging. 2014;41:946–55.
Knackstedt C, Schauerte P, Kirchhof P. Electro-anatomic mapping systems in arrhythmias. Europace. 2008;10 Suppl 3:iii28–34.
Robinson MR, Hutchinson MD. Use of imaging techniques to guide catheter ablation procedures. Curr Cardiol Rep. 2010;12:374–81.
Gimelli A, Masci PG, Liga R, Grigoratos C, Pasanisi EM, Lombardi M, et al. Regional heterogeneity in cardiac sympathetic innervation in acute myocardial infarction: relationship with myocardial oedema on magnetic resonance. Eur J Nucl Med Mol Imaging. 2014;41:1692–4.
Romero J, Lupercio F, Goodman-Meza D, Ruiz JC, Briceno DF, Fisher JD, et al. Electroanatomic mapping systems (CARTO/EnSite NavX) vs. conventional mapping for ablation procedures in a training program. J Interv Card Electrophysiol. 2016;45:71–80.
Heidbuchel H, Wittkampf FH, Vano E, Ernst S, Schilling R, Picano E, et al. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014;16:946–64.
Marchlinski FE, Callans DJ, Gottlieb CD, Zado E. Linear ablation lesions for control of unmappable ventricular tachycardia in patients with ischemic and nonischemic cardiomyopathy. Circulation. 2000;101:1288–96.
Hsia HH, Lin D, Sauer WH, Callans DJ, Marchlinski FE. Anatomic characterization of endocardial substrate for hemodynamically stable reentrant ventricular tachycardia: identification of endocardial conducting channels. Heart Rhythm. 2006;3:503–12.
Sacher F, Lim HS, Derval N, Denis A, Berte B, Yamashita S, et al. Substrate mapping and ablation for ventricular tachycardia: the LAVA approach. J Cardiovasc Electrophysiol. 2015;26:464–71.
Kuteszko R, Pytkowski M, Farkowski MM, Maciag A, Sterlinski M, Jankowska A, et al. Utility of automated template matching for the interpretation of pace mapping in patients ablated due to outflow tract ventricular arrhythmias. Europace. 2015;17:1428–34.
Klein T, Abdulghani M, Smith M, Huang R, Asoglu R, Remo BF, et al. Three-dimensional 123I-meta-iodobenzylguanidine cardiac innervation maps to assess substrate and successful ablation sites for ventricular tachycardia: feasibility study for a novel paradigm of innervation imaging. Circ Arrhythm Electrophysiol. 2015;8:583–91.
Zhao C, Shuke N, Yamamoto W, Okizaki A, Sato J, Ishikawa Y, et al. Comparison of cardiac sympathetic nervous function with left ventricular function and perfusion in cardiomyopathies by 123I-MIBG SPECT and 99mTc-tetrofosmin electrocardiographically gated SPECT. J Nucl Med. 2001;42:1017–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Alessia Gimelli and Francesca Menichetti shared first co-authorship.
Rights and permissions
About this article
Cite this article
Gimelli, A., Menichetti, F., Soldati, E. et al. Relationships between cardiac innervation/perfusion imbalance and ventricular arrhythmias: impact on invasive electrophysiological parameters and ablation procedures. Eur J Nucl Med Mol Imaging 43, 2383–2391 (2016). https://doi.org/10.1007/s00259-016-3461-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-016-3461-y