Abstract
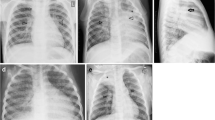
Imaging is crucial in the diagnostic work-up and follow-up after treatment in children with thoracic tuberculosis (TB). Despite various technological advances in imaging modalities, chest radiography is the primary imaging modality for initial care and in emergency settings, especially in rural areas and where resources are limited. Ultrasonography (US) of the thorax in TB is one of the emerging applications of US as a radiation-free modality in children. Magnetic resonance imaging (MRI) is the ideal radiation-free, emerging imaging modality for thoracic TB in children. However, only limited published data is available regarding the utility of MRI in thoracic TB. In this pictorial review, we demonstrate the use of US and rapid lung MRI in evaluating children with thoracic TB, specifically for mediastinal lymphadenopathy and pulmonary complications of TB.
Graphical Abstract






















Similar content being viewed by others
References
Pool KL, Heuvelings CC, Bélard S et al (2017) Technical aspects of mediastinal ultrasound for pediatric pulmonary tuberculosis. Pediatr Radiol 47:1839–1848. https://doi.org/10.1007/s00247-017-3954-2
Ruby LC, Heuvelings CC, Grobusch MP et al (2022) Transthoracic mediastinal ultrasound in childhood tuberculosis: a review. Paediatr Respir Rev 41:40–48. https://doi.org/10.1016/j.prrv.2020.11.002
Bhalla D, Sinha P, Naranje P et al (2022) Transcutaneous mediastinal ultrasonography for lymphadenopathy in children: a pictorial essay of technique and imaging findings. J Ultrasound Med 41:773–783. https://doi.org/10.1002/jum.15760
Heuvelings CC, Bélard S, Familusi MA et al (2019) Chest ultrasound for the diagnosis of paediatric pulmonary diseases: a systematic review and meta-analysis of diagnostic test accuracy. In: British Medical Bulletin (Vol. 129, Issue 1) Oxford University Press, pp. 69–78. https://doi.org/10.1093/bmb/ldy041
Di Gennaro F, Pisani L, Veronese N et al (2018) Potential diagnostic properties of chest ultrasound in thoracic tuberculosis-a systematic review. Int J Environ Res Public Health 15:2235. https://doi.org/10.3390/ijerph15102235
Pillay T, Andronikou S, Zar HJ (2020) Chest imaging in paediatric pulmonary TB. Paediatr Respir Rev 36:65–72. https://doi.org/10.1016/j.prrv.2020.10.002
Sodhi KS, Khandelwal N, Saxena AK et al (2016) Rapid lung MRI in children with pulmonary infections: time to change our diagnostic algorithms. J Magn Reson Imaging 43:1196–1206. https://doi.org/10.1002/jmri.25082
Sodhi KS, Khandelwal N, Saxena AK et al (2016) Rapid lung MRI — paradigm shift in evaluation of febrile neutropenia in children with leukemia: a pilot study. Leuk Lymphoma 57:70–75. https://doi.org/10.3109/10428194.2015.104138
Yikilmaz A, Koc A, Coskun A et al (2011) Evaluation of pneumonia in children: comparison of MRI with fast imaging sequences at 1.5T with chest radiographs. Acta Radiol 52:914–919. https://doi.org/10.1258/ar.2011.100429
Sodhi KS, Bhatia A, Nichat V et al (2021) Chest MRI as an emerging modality in the evaluation of empyema in children with specific indications: Pilot study. Pediatr Pulmonol 56:2668–2675. https://doi.org/10.1002/ppul.25457
Nagel SN, Wyschkon S, Schwartz S et al (2016) Can magnetic resonance imaging be an alternative to computed tomography in immunocompromised patients with suspected fungal infections? Feasibility of a speed optimized examination protocol at 3 tesla. Eur J Radiol 85:857–863. https://doi.org/10.1016/j.ejrad.2016.02.009
Sodhi KS, Sharma M, Lee EY et al (2018) Diagnostic utility of 3T lung MRI in children with interstitial lung disease: a prospective pilot study. Acad Radiol 25:380–386. https://doi.org/10.1016/j.acra.2017.09.013
Yan C, Tan X, Wei Q et al (2015) Lung MRI of invasive fungal infection at 3 tesla: evaluation of five different pulse sequences and comparison with multidetector computed tomography (MDCT). Eur Radiol 25:550–557. https://doi.org/10.1007/s00330-014-3432-2
Sodhi KS, Gupta P, Shrivastav A et al (2019) Evaluation of 3 T lung magnetic resonance imaging in children with allergic bronchopulmonary aspergillosis: Pilot study. Eur J Radiol 111:88–92. https://doi.org/10.1016/j.ejrad.2018.12.021
Liszewski MC, Görkem S, Sodhi KS, Lee EY (2017) Lung magnetic resonance imaging for pneumonia in children. Pediatr Radiol 47:1420–1430. https://doi.org/10.1007/s00247-017-3865-2
Chung JH, Huitt G, Yagihashi K et al (2016) Proton magnetic resonance imaging for initial assessment of isolated mycobacterium avium complex pneumonia. Ann Am Thorac Soc 13:49–57. https://doi.org/10.1513/AnnalsATS.201505-282O
Rana P, Sodhi KS, Bhatia A et al (2020) Diagnostic accuracy of 3-T lung magnetic resonance imaging in human immunodeficiency virus-positive children. Pediatr Radiol 50:38–45. https://doi.org/10.1007/s00247-019-04523-0
Sodhi KS, Sharma M, Saxena AK et al (2017) MRI in thoracic tuberculosis of children. Indian J Pediatr 84:670–676. https://doi.org/10.1007/s12098-017-2392-3
Sodhi KS, Ciet P, Vasanawala S, Biederer J (2022) Practical protocol for lung magnetic resonance imaging and common clinical indications. Pediatr Radiol 52:295–311. https://doi.org/10.1007/s00247-021-05090-z
Sodhi KS (2021) Lung MRI in children: the road less travelled. Indian J Radiol Imaging 31:237–241. https://doi.org/10.1055/s-0041-1729126
Yucel S, Aycicek T, Ceyhan Bilgici M et al (2021) 3 Tesla MRI in diagnosis and follow up of children with pneumonia. Clin Imaging 79:213–218. https://doi.org/10.1016/j.clinimag.2021.05.027
Garg MK, Gupta P, Agarwal R et al (2015) MRI: a new paradigm in imaging evaluation of allergic bronchopulmonary aspergillosis? Chest 147:e58–e59. https://doi.org/10.1378/chest.14-2347
Ozcan HN, Gormez A, Ozsurekci Y et al (2017) Magnetic resonance imaging of pulmonary infection in immunocompromised children: comparison with multidetector computed tomography. Pediatr Radiol 47:146–153. https://doi.org/10.1007/s00247-016-3729-1
Gorkem SB, Coskun A, Yikilmaz A et al (2013) Evaluation of pediatric thoracic disorders: comparison of unenhanced fast-imaging-sequence 1.5-T MRI and contrast-enhanced MDCT. AJR Am J Roentgenol 200:1352–1357. https://doi.org/10.2214/AJR.12.9502
Kapur S, Bhalla AS, Jana M (2019) Pediatric chest MRI: a review. Indian J Pediatr 86:842–853. https://doi.org/10.1007/s12098-018-02852-w
Naranje P, Bhalla AS, Sherwani P (2019) Chest tuberculosis in children. Indian J Pediatr 86:448–458. https://doi.org/10.1007/s12098-018-02847-7
Bosch-Marcet J, Serres-Créixams X, Borrás-Pérez V et al (2007) Value of sonography for follow-up of mediastinal lymphadenopathy in children with tuberculosis. J Clin Ultrasound 35:118–124. https://doi.org/10.1002/jcu
Sodhi KS, Bhalla AS, Mahomed N, Laya BF (2017) Imaging of thoracic tuberculosis in children: current and future directions. Pediatr Radiol 47:1260–1268. https://doi.org/10.1007/s00247-017-3866-1
Heuvelings CC, Bélard S, Andronikou S et al (2019) Chest ultrasound compared to chest X-ray for pediatric pulmonary tuberculosis. Pediatr Pulmonol 54:1914–1920. https://doi.org/10.1002/ppul.24500
Moseme T, Andronikou S (2014) Through the eye of the suprasternal notch: point-of-care sonography for tuberculous mediastinal lymphadenopathy in children. Pediatr Radiol 44:681–684. https://doi.org/10.1007/s00247-014-2890-7
Fentress M, Henwood PC, Maharaj P et al (2022) Thoracic ultrasound for TB diagnosis in adults and children. Public Health Action 12:3–6. https://doi.org/10.5588/pha.21.0072
Heuvelings CC, Bélard S, Andronikou S et al (2019) Chest ultrasound findings in children with suspected pulmonary tuberculosis. Pediatr Pulmonol 54:463–470. https://doi.org/10.1002/ppul.24230
Hunter L, Bélard S, Janssen S et al (2016) Miliary tuberculosis: sonographic pattern in chest ultrasound. Infection 44:243–246. https://doi.org/10.1007/s15010-015-0865-8
Wernecke K, Vassallo P, Potter R et al (1990) Mediastinal tumors: sensitivity of detection with sonography compared with CT and radiography. Radiology 175:137–143. https://doi.org/10.1148/RADIOLOGY.175.1.2179987
Jana M, Mittal D, Bhalla AS et al (2021) High resolution transthoracic ultrasound in evaluation of pediatric mediastinal lymphadenopathy. Indian J Pediatr 88:105. https://doi.org/10.1007/s12098-020-03485-8
Peprah KO, Andronikou S, Goussard P (2012) Characteristic magnetic resonance imaging low T2 signal intensity of necrotic lung parenchyma in children with pulmonary tuberculosis. J Thorac Imaging 27:171–174. https://doi.org/10.1097/RTI.0b013e318211abfb
Zeng J, Liu Z, Shen G et al (2019) MRI evaluation of pulmonary lesions and lung tissue changes induced by tuberculosis. Int J Infect Dis 82:138–146. https://doi.org/10.1016/j.ijid.2019.03.004
Author information
Authors and Affiliations
Contributions
K.S.S. conceived, supervised, and supported the work. K.S.S., S.K., M.J., and A.B. drafted the initial manuscript and revised it critically for intellectual content. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sodhi, K.S., Kritsaneepaiboon, S., Jana, M. et al. Ultrasound and magnetic resonance imaging in thoracic tuberculosis in the pediatric population: moving beyond conventional radiology. Pediatr Radiol 53, 2552–2567 (2023). https://doi.org/10.1007/s00247-023-05787-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05787-3