Abstract
Background
Computed tomography (CT) can be used for the early detection of lymphadenitis. Radiomics is able to identify a large amount of hidden information from images. However, few CT-based radiomics studies on cervical lymphadenitis in children have been published.
Objective
This study aimed to investigate the role of visual CT analysis and CT radiomics in differentiating cervical suppurative node necrosis from tuberculous node necrosis in pediatric patients.
Materials and methods
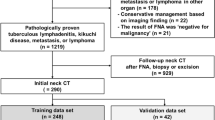
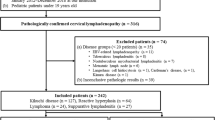
A total of 101 patients with cervical suppurative lymphadenitis (n=52) or cervical tuberculous lymphadenitis (n=49) were included. Clinical data and CT images were retrieved for analysis. For visual observation, 11 major CT features were identified for univariate and multivariate analyses. For radiomics analysis, image segmentation, feature value extraction, and dimension reduction, feature selection and the construction of radiomics-based models were performed through the RadCloud platform.
Results
For the visual observation, significant differences were found between the two groups, including the short diameter of the largest necrotic lymph node (P=0.03), sharp border of the node (P=0.02), fusion of nodes (P=0.02), regular silhouette of the necrotic area (P=0.001), multilocular necrotic area (P=0.02), node calcification (P=0.004), and enhancement degree of the nodal nonnecrotic area (P=0.01). No feature was found to be an independent predictor for suppurative or tuberculous lymphadenitis (P>0.05 for all features). Concerning the radiomics analysis, after feature value extraction and dimension reduction, nine related features were selected. The support vector machine classifier achieved high diagnostic performance in distinguishing suppurative from tuberculous lymphadenitis. The area under the curve, accuracy, sensitivity, and specificity of the support vector machine model test set were 0.89 (95% confidence interval: 0.72–1.00), 0.88, 0.78, and 0.90, respectively.
Conclusion
Compared to observer-based CT image analyses, radiomics model-based CT image analyses exhibit better performance in the differential diagnosis of cervical suppurative and tuberculous lymphadenitis complicated with nodal necrosis in children.
Graphical abstract






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lou F, Zhang T, Ming C et al (2020) Clinic analysis of cervical lymph node lesions in children. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 34:928–931
Lyon SM, Rossman MD (2017) Pulmonary tuberculosis. Microbiol Spectr 5(1):10–1128
Naranje P, Bhalla AS, Sherwani P (2019) Chest tuberculosis in children. Indian J Pediatr 86:448–458
Roy CF, Balakrishnan K, Boudewyns A et al (2023) International Pediatric Otolaryngology Group: Consensus guidelines on the diagnosis and management of nontuberculous mycobacterial cervicofacial lymphadenitis. Int J Pediatr Otorhinolaryngol 166:111469
Baek CH, Kim SI, Ko YH et al (2000) Polymerase chain reaction detection of mycobacterium tuberculosis from fine-needle aspirate for the diagnosis of cervical tuberculous lymphadenitis. Laryngoscope 110:30–34
Mittal P, Handa U, Mohan H et al (2011) Comparative evaluation of fine needle aspiration cytology, culture, and PCR in diagnosis of tuberculous lymphadenitis. Diagn Cytopathol 39:822–826
Ahuja AT, Ying M, Ho SY et al (2008) Ultrasound of malignant cervical lymph nodes. Cancer Imaging 8:48–56
Eisenmenger LB, Wiggins RH 3rd (2015) Imaging of head and neck lymph nodes. Radiol Clin North Am 53:115–132
Schröder RJ, Rost B, Hidajat N et al (2002) Value of contrast-enhanced ultrasound vs. CT and MRI in palpable enlarged lymph nodes of the head and neck. Rofo 174:1099–1106
Holzapfel K, Duetsch S, Fauser C et al (2009) Value of diffusion-weighted MR imaging in the differentiation between benign and malignant cervical lymph nodes. Eur J Radiol 72:381–387
Steinkamp HJ, Hosten N, Richter C et al (1994) Enlarged cervical lymph nodes at helical CT. Radiology 191:795–798
Cunqueiro A, Gomes WA, Lee P et al (2019) CT of the neck: image analysis and reporting in the emergency setting. Radiographics 39:1760–1781
Mayerhoefer ME, Materka A, Langs G et al (2020) Introduction to radiomics. J Nucl Med 61:488–495
Tsai YL, Chen SW, Kao CH et al (2022) Neck lymph node recurrence in HNC patients might be predicted before radiotherapy using radiomics extracted from CT images and XGBoost algorithm. J Pers Med 12:1377
Wang H, Chen X, Liu H et al (2021) Computed tomography-based radiomics for differential of retroperitoneal neuroblastoma and ganglioneuroblastoma in children. Nan Fang Yi Ke Da Xue Xue Bao 41:1569–1576
Grégoire V, Ang K, Budach W et al (2014) Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol 110:172–181
Kayi Cangir A, Orhan K, Kahya Y et al (2021) CT imaging-based machine learning model: a potential modality for predicting low-risk and high-risk groups of thymoma: “impact of surgical modality choice.” World J Surg Oncol 19:147
Cangir AK, Orhan K, Kahya Y et al (2022) A CT-based radiomic signature for the differentiation of pulmonary hamartomas from carcinoid tumors. Diagnostics (Basel) 12:416
Kato H, Kanematsu M, Kato Z et al (2013) Necrotic cervical nodes: usefulness of diffusion-weighted MR imaging in the differentiation of suppurative lymphadenitis from malignancy. Eur J Radiol 82:e28–e35
Srinivas CV, Nair S (2019) Clinicopathological profile of cervical tubercular lymphadenitis with special reference to fine needle aspiration cytology. Indian J Otolaryngol Head Neck Surg 71:205–211
Agarwal A (2020) Paediatric osteoarticular tuberculosis: a review. J Clin Orthop Trauma 11:202–207
Fraser IP (2009) Suppurative lymphadenitis. Curr Infect Dis Rep 11:383–388
Kim WS, Moon WK, Kim IO et al (1997) Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol 168:1005–1009
Luo MY, Liu L, Lai LS et al (2010) Deepgoing study on intrathoracic tuberculous lymphadenitis in adults using multidetector CT. Chin Med J (Engl) 123:1283–1288
Lee S, Yoo JH, Lee SW (2012) Kikuchi disease: differentiation from tuberculous lymphadenitis based on patterns of nodal necrosis on CT. AJNR Am J Neuroradiol 33:135–140
Kim BH, Lee C, Lee JY et al (2022) Initial experience of a deep learning application for the differentiation of Kikuchi-Fujimoto’s disease from tuberculous lymphadenitis on neck CECT. Sci Rep 12:14184
Gillies RJ, Kinahan PE, Hricak H (2015) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Liu A, Wang Z, Yang Y et al (2020) Preoperative diagnosis of malignant pulmonary nodules in lung cancer screening with a radiomics nomogram. Cancer Commun (Lond) 40:16–24
Fasmer KE, Hodneland E, Dybvik JA et al (2021) Whole-volume tumor MRI radiomics for prognostic modeling in endometrial cancer. J Magn Reson Imaging 53:928–937
Li Y, Liu Y, Liang Y et al (2022) Radiomics can differentiate high-grade glioma from brain metastasis: a systematic review and meta-analysis. Eur Radiol 32:8039–8051
Song J, Yin Y, Wang H et al (2020) A review of original articles published in the emerging field of radiomics. Eur J Radiol 127:108991
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design; material preparation, data collection, and analysis were performed by R.Z., S.G., and W.L.; the first draft of the manuscript was written by R.Z. and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was waived by Children’s Hospital of Chongqing Medical University in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, R., Xu, Y., Gao, S. et al. Observer- and radiomics model-based computed tomography classification of suppurative versus tuberculous lymphadenitis complicated with nodal necrosis of the neck in children. Pediatr Radiol 53, 2586–2596 (2023). https://doi.org/10.1007/s00247-023-05761-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05761-z