Abstract
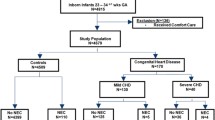
Infants with congenital heart disease (CHD) are at risk for developing both benign hematochezia and necrotizing enterocolitis (NEC). Despite these risks there are very few studies that investigate modifiable risk factors such as feeding practices. It remains unclear what feeding practices should be avoided due to higher incidence of CHD-NEC. We aim to assess the feeding practices across three high volume tertiary centers to establish a relationship between various feeding practices and development of NEC. A multicenter retrospective review of feeding practices at the time of documented hematochezia event that occurred between 1/2019 and 1/2021 in infants with CHD who were less than 6 months of age. NEC was defined as Bells Stage 2 or greater. Age, weight, ventricular morphology, primary diagnoses, feeding route, feed change, and formula type were evaluated. 176 hematochezia events occurred in 121 patients, 72% of these events were considered benign hematochezia with the remaining 28% being true NEC. Single ventricle (SV) physiology (p < 0.05), younger age, < 45 days of life, (p < 0.001), and feeding route were statistically associated with true NEC (p < 0.01). Formula type and recent change in feed administration were not associated with NEC. The caloric density of feeds at the time of hematochezia was nearing significance. The majority of hematochezia events are benign in nature, however, there should be heightened awareness in patients who are SV, younger in age, and those who are post-pylorically fed. There may be some risk in using higher caloric density feeds (> 24 kcal/oz), however, additional research is needed to fully establish this relationship.


Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Siano E, Lauriti G, Ceccanti S, Zani A (2019) Cardiogenic necrotizing enterocolitis: a clinically distinct entity from classical necrotizing enterocolitis. Eur J Pediatr Surg 29(1):14–22. https://doi.org/10.1055/s-0038-1668144
Spinner JA, Morris SA, Nandi D, Costarino AT, Marino BS, Rossano JW, Shamszad P (2020) Necrotizing enterocolitis and associated mortality in neonates with congenital heart disease: a multi-institutional study. Pediatr Crit Care Med 21(3):228–234. https://doi.org/10.1097/PCC.0000000000002133
Lau PE, Cruz SM, Ocampo EC, Nuthakki S, Style CC, Lee TC, Wesson DE, Olutoye OO (2018) Necrotizing enterocolitis in patients with congenital heart disease: a single center experience. J Pediatr Surg 53(5):914–917. https://doi.org/10.1016/j.jpedsurg.2018.02.014
Kelleher ST, McMahon CJ, James A (2021) Necrotizing enterocolitis in children with congenital heart disease: a literature review. Pediatr Cardiol 8:1688–1700. https://doi.org/10.1007/S00246-021-02691-1
Zyblewski SC, Nietert PJ, Graham EM, Taylor SN, Atz AM, Wagner CL (2015) Randomized clinical trial of preoperative feeding to evaluate intestinal barrier function in neonates requiring cardiac surgery. J Pediatr 167(1):47-51.e1. https://doi.org/10.1016/j.jpeds.2015.04.035
McElhinney DB, Hedrick HL, Bush DM, Pereira GR, Stafford PW, Gaynor JW, Spray TL, Wernovsky G (2000) Necrotizing enterocolitis in neonates with congenital heart disease: risk factors and outcomes. Pediatrics 106(5):1080–1087. https://doi.org/10.1542/peds.106.5.1080
del Castillo SL, McCulley ME, Khemani RG, Jeffries HE, Thomas DW, Peregrine J, Wells WJ, Starnes VA, Moromisato DY (2010) Reducing the incidence of necrotizing enterocolitis in neonates with hypoplastic left heart syndrome with the introduction of an enteral feed protocol. Pediatr Crit Care Med 3:373–377. https://doi.org/10.1097/PCC.0b013e3181c01475
Jeffries HE, Wells WJ, Starnes VA, Wetzel RC, Moromisato DY (2006) Gastrointestinal morbidity after Norwood palliation for hypoplastic left heart syndrome. Ann Thorac Surg 81(3):982–987. https://doi.org/10.1016/j.athoracsur.2005.09.001
Nordenström K, Lannering K, Mellander M, Elfvin A (2020) Low risk of necrotising enterocolitis in enterally fed neonates with critical heart disease: an observational study. Arch Dis Child Fetal Neonatal Ed 105(6):609–614. https://doi.org/10.1136/archdischild-2019-318537
Becker KC, Hornik CP, Cotten CM, Clark RH, Hill KD, Smith PB, Lenfestey RW (2015) Necrotizing enterocolitis in infants with ductal-dependent congenital heart disease. Am J Perinatol 32(7):633–638. https://doi.org/10.1055/s-0034-1390349
Iannucci GJ, Oster ME, Mahle WT (2013) Necrotising enterocolitis in infants with congenital heart disease: the role of enteral feeds. Cardiol Young 4:553–559. https://doi.org/10.1017/S1047951112001370
Salvatori G, de Rose DU, Massolo AC, Patel N, Capolupo I, Giliberti P, Evangelisti M, Parisi P, Toscano A, Dotta A, di Nardo G (2022) Current strategies to optimize nutrition and growth in newborns and infants with congenital heart disease: a narrative review. J Clin Med 11(1841):1841. https://doi.org/10.3390/JCM11071841
Cognata A, Kataria-Hale J, Griffiths P, Maskatia S, Rios D, O’Donnell A, Roddy DJ, Mehollin-Ray A, Hagan J, Placencia J, Hair AB (2019) Human milk use in the preoperative period is associated with a lower risk for necrotizing enterocolitis in neonates with complex congenital heart disease. J Pediatr 215:11-16.e2. https://doi.org/10.1016/j.jpeds.2019.08.009
Elgersma KM, Wolfson J, Fulkerson JA, Georgieff MK, Looman WS, Spatz DL, Shah KM, Uzark K, McKechnie AC (2023) Human milk feeding and direct breastfeeding improve outcomes for infants with single ventricle congenital heart disease: propensity score-matched analysis of the NPC-QIC registry. J Am Heart Assoc. https://doi.org/10.1161/JAHA.123.030756
Blanco CL, Hair A, Justice LB, Roddy D, Bonagurio K, Williams PK, Machado D, Marino BS, Chi A, Takao C, Gordon EE, Ashrafi A, Cacho N, Pruetz JD, Costello JM, Cooper DS (2023) A randomized trial of an exclusive human milk diet in neonates with single ventricle physiology. J Pediatr. https://doi.org/10.1016/j.jpeds.2022.11.043
Braudis NJ, Curley MAQ, Beaupre K, Thomas KC, Hardiman G, Laussen P, Gauvreau K, Thiagarajan RR (2009) Enteral feeding algorithm for infants with hypoplastic left heart syndrome poststage I palliation. Pediatr Crit Care Med 10(4):460–466. https://doi.org/10.1097/PCC.0b013e318198b167
Lin M, Zhu H, Zhang R, Wang H (2022) Causes of bloody stools in neonates: a case series report. Transl Pediatr 11(9):1438–1444. https://doi.org/10.21037/tp-22-166
Elgersma KM, McKechnie AC, Schorr EN, Shah KM, Trebilcock AL, Ramel SE, Ambrose MB, Swanson NM, Sommerness SA, Spatz DL (2022) The impact of human milk on outcomes for infants with congenital heart disease: a systematic review. Breastfeed Med 5:393–411
Schuchardt EL, Kaufman J, Lucas B, Tiernan K, Lujan SO, Barrett C (2018) Suspected necrotising enterocolitis after surgery for CHD: an opportunity to improve practice and outcomes. Cardiol Young 28(5):639–646. https://doi.org/10.1017/S1047951117002815
Kataria-Hale J, Gollins L, Bonagurio K, Blanco C, Hair AB (2023) Nutrition for infants with congenital heart disease. Clin Perinatol 50(3):699–713. https://doi.org/10.1016/J.CLP.2023.04.007
Acknowledgements
Amy Schiller on behalf of the Pediatric Acute Care Cardiology Collaborative (PAC3)
Funding
No funding was received to support the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
KP wrote the main manuscript text. ZG prepared graphics. All Authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Palm, K., Trauth, A., Gao, Z. et al. Feeding Practices in Infants with Hematochezia and Necrotizing Enterocolitis on Acute Care Cardiology Units. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03406-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03406-y