Abstract
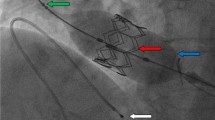
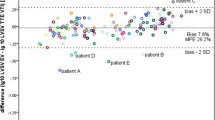
Patients with congenital heart disease (CHD) who undergo cardiac procedures may become hemodynamically unstable. Predictive algorithms that utilize dense physiologic data may be useful. The compensatory reserve index (CRI) trends beat-to-beat progression from normovolemia (CRI = 1) to decompensation (CRI = 0) in hemorrhagic shock by continuously analyzing unique sets of features in the changing pulse photoplethysmogram (PPG) waveform. We sought to understand if the CRI accurately reflects changing hemodynamics during and after a cardiac procedure for patients with CHD. A transcatheter pulmonary valve replacement (TcPVR) model was used because left ventricular stroke volume decreases upon sizing balloon occlusion of the right ventricular outflow tract (RVOT) and increases after successful valve placement. A single-center, prospective cohort study was performed. The CRI was continuously measured to determine the change in CRI before and after RVOT occlusion and successful TcPVR. Twenty-six subjects were enrolled with a median age of 19 (interquartile range (IQR) 13–29) years. The mean (± standard deviation) CRI decreased from 0.66 ± 0.15 1-min before balloon inflation to 0.53 ± 0.16 (p = 0.03) 1-min after balloon deflation. The mean CRI increased from a pre-valve mean CRI of 0.63 [95% confidence interval (CI) 0.56–0.70] to 0.77 (95% CI 0.71–0.83) after successful TcPVR. In this study, the CRI accurately reflected acute hemodynamic changes associated with TcPVR. Further research is justified to determine if the CRI can be useful as an early warning tool in patients with CHD at risk for decompensation during and after cardiac procedures.





Similar content being viewed by others
References
McCracken C, Spector Logan G, Menk Jeremiah S, Knight Jessica H, Vinocur Jeffrey M, Thomas Amanda S, Oster Matthew E, St Louis James D, Moller James H, Kochilas L (2018) Mortality following pediatric congenital heart surgery: an analysis of the causes of death derived from the national death index. J Am Heart Assoc 7(22):e010624. https://doi.org/10.1161/JAHA.118.010624
Berger JT, Holubkov R, Reeder R, Wessel DL, Meert K, Berg RA, Bell MJ, Tamburro R, Dean JM, Pollack MM, Eunice Kennedy Shriver National Institute of Child Health, and Human Development Collaborative Pediatric Critical Care Research Network (2017) Morbidity and mortality prediction in pediatric heart surgery: physiological profiles and surgical complexity. J Thorac Cardiovasc Surg 154(2):620–628.e6. https://doi.org/10.1016/j.jtcvs.2017.01.050
Olive MK, Owens GE (2018) Current monitoring and innovative predictive modeling to improve care in the pediatric cardiac intensive care unit. Transl Pediatr 7(2):120–128. https://doi.org/10.21037/tp.2018.04.03
Moulton SL, Mulligan J, Grudic GZ, Convertino VA (2013) Running on empty? The compensatory reserve index. J Trauma Acute Care Surg 75(6):1053–1059. https://doi.org/10.1097/TA.0b013e3182aa811a
Convertino VA, Grudic G, Mulligan J (1985) Moulton S (2013) Estimation of individual-specific progression to impending cardiovascular instability using arterial waveforms. J Appl Physiol 115(8):1196–1202. https://doi.org/10.1152/japplphysiol.00668.2013
Moulton SL, Mulligan J, Santoro MA, Bui K, Grudic GZ, MacLeod D (2017) Validation of a noninvasive monitor to continuously trend individual responses to hypovolemia. J Trauma Acute Care Surg 83(1 Suppl 1):S104–S111. https://doi.org/10.1097/TA.0000000000001511
Stewart CL, Nawn CD, Mulligan J, Grudic G, Moulton SL, Convertino VA (2016) Compensatory reserve for early and accurate prediction of hemodynamic compromise: case studies for clinical utility in acute care and physical performance. J Spec Oper Med 16(1):6–13
Choi YM, Leopold D, Campbell K, Mulligan J, Grudic GZ, Moulton SL (2018) Noninvasive monitoring of physiologic compromise in acute appendicitis: new insight into an old disease. J Pediatr Surg 53(2):241–246. https://doi.org/10.1016/j.jpedsurg.2017.11.013
Stewart CL, Mulligan J, Grudic GZ, Pyle L, Moulton SL (2015) A noninvasive computational method for fluid resuscitation monitoring in pediatric burns: a preliminary report. J Burn Care Res 36(1):145–150. https://doi.org/10.1097/BCR.0000000000000178
McElhinney DB, Hellenbrand WE, Zahn EM, Jones TK, Cheatham JP, Lock JE, Vincent JA (2010) Short- and medium-term outcomes after transcatheter pulmonary valve placement in the expanded multicenter US melody valve trial. Circulation 122(5):507–516. https://doi.org/10.1161/circulationaha.109.921692
Callahan R, Bergersen L, Baird CW, Porras D, Esch JJ, Lock JE, Marshall AC (2017) Mechanism of valve failure and efficacy of reintervention through catheterization in patients with bioprosthetic valves in the pulmonary position. Ann Pediatr Cardiol 10(1):11–17. https://doi.org/10.4103/0974-2069.197049
Lurz P, Puranik R, Nordmeyer J, Muthurangu V, Hansen MS, Schievano S, Marek J, Bonhoeffer P, Taylor AM (2009) Improvement in left ventricular filling properties after relief of right ventricle to pulmonary artery conduit obstruction: contribution of septal motion and interventricular mechanical delay. Eur Heart J 30(18):2266–2274. https://doi.org/10.1093/eurheartj/ehp258
Khambadkone S, Coats L, Taylor A, Boudjemline Y, Derrick G, Tsang V, Cooper J, Muthurangu V, Hegde SR, Razavi RS, Pellerin D, Deanfield J, Bonhoeffer P (2005) Percutaneous pulmonary valve implantation in humans: results in 59 consecutive patients. Circulation 112(8):1189–1197. https://doi.org/10.1161/circulationaha.104.523266
Esper SA, Pinsky MR (2014) Arterial waveform analysis. Best Pract Res Clin Anaesthesiol 28(4):363–380. https://doi.org/10.1016/j.bpa.2014.08.002
Convertino VA, Wirt MD, Glenn JF, Lein BC (2016) The compensatory reserve for early and accurate prediction of hemodynamic compromise: a review of the underlying physiology. Shock 45(6):580–590. https://doi.org/10.1097/SHK.0000000000000559
Convertino VA, Schiller AM (2017) Measuring the compensatory reserve to identify shock. J Trauma Acute Care Surg 82(6S Suppl 1):S57–S65. https://doi.org/10.1097/TA.0000000000001430
Stewart CL, Mulligan J, Grudic GZ, Talley ME, Jurkovich GJ, Moulton SL (2016) The compensatory reserve index following injury: Results of a prospective clinical trial. Shock 46(3 Suppl 1):61–67. https://doi.org/10.1097/SHK.0000000000000647
Stewart CL, Mulligan J, Grudic GZ, Convertino VA, Moulton SL (2014) Detection of low-volume blood loss: compensatory reserve versus traditional vital signs. J Trauma Acute Care Surg 77 (6):892–897; discussion 897–898. https://doi.org/10.1097/TA.0000000000000423
Johnson MC, Alarhayem A, Convertino V, Carter R 3rd, Chung K, Stewart R, Myers J, Dent D, Liao L, Cestero R, Nicholson S, Muir M, Schwacha M, Wampler D, DeRosa M, Eastridge B (2018) Compensatory reserve index: performance of a novel monitoring technology to identify the bleeding trauma patient. Shock 49(3):295–300. https://doi.org/10.1097/SHK.0000000000000959
Nadler R, Convertino VA, Gendler S, Lending G, Lipsky AM, Cardin S, Lowenthal A, Glassberg E (2014) The value of noninvasive measurement of the compensatory reserve index in monitoring and triage of patients experiencing minimal blood loss. Shock 42(2):93–98. https://doi.org/10.1097/SHK.0000000000000178
Janak JC, Howard JT, Goei KA, Weber R, Muniz GW, Hinojosa-Laborde C, Convertino VA (2015) Predictors of the onset of hemodynamic decompensation during progressive central hypovolemia: comparison of the peripheral perfusion index, pulse pressure variability, and compensatory reserve index. Shock 44(6):548–553. https://doi.org/10.1097/SHK.0000000000000480
Feltes TF, Bacha E, Beekman RH 3rd, Cheatham JP, Feinstein JA, Gomes AS, Hijazi ZM, Ing FF, de Moor M, Morrow WR, Mullins CE, Taubert KA, Zahn EM (2011) Indications for cardiac catheterization and intervention in pediatric cardiac disease: a scientific statement from the American Heart Association. Circulation 123(22):2607–2652. https://doi.org/10.1161/CIR.0b013e31821b1f10
Bonhoeffer P, Boudjemline Y, Qureshi SA, Le Bidois J, Iserin L, Acar P, Merckx J, Kachaner J, Sidi D (2002) Percutaneous insertion of the pulmonary valve. J Am Coll Cardiol 39(10):1664–1669. https://doi.org/10.1016/s0735-1097(02)01822-3
Rhodes John F, Blaufox Andrew D, Seiden Howard S, Asnes Jeremy D, Gross Ronda P, Rhodes Julianna P, Griepp Randall B, Rossi Anthony F (1999) Cardiac arrest in infants after congenital heart surgery. Circulation 100(suppl 2):II-194–II-I99. https://doi.org/10.1161/circ.100.suppl_2.Ii-194
Gupta P, Jacobs JP, Pasquali SK, Hill KD, Gaynor JW, O’Brien SM, He M, Sheng S, Schexnayder SM, Berg RA, Nadkarni VM, Imamura M, Jacobs ML (2014) Epidemiology and outcomes after in-hospital cardiac arrest after pediatric cardiac surgery. Ann Thorac Surg 98(6):2138–2143; discussion 2144. https://doi.org/10.1016/j.athoracsur.2014.06.103
Bose SN, Verigan A, Hanson J, Ahumada LM, Ghazarian SR, Goldenberg N, Stock A, Jacobs JP (2019) Early identification of impending cardiac arrest in neonates and infants in the cardiovascular ICU: a statistical modelling approach using physiologic monitoring data. Cardiol Young 29(11):1340–1348. https://doi.org/10.1017/S1047951119002002
McLellan MC, Connor JA (2013) The Cardiac Children's Hospital Early Warning Score (C-CHEWS). J Pediatr Nurs 28(2):171–178. https://doi.org/10.1016/j.pedn.2012.07.009
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated pediatric risk of mortality score. Crit Care Med 24(5):743–752. https://doi.org/10.1097/00003246-199605000-00004
Eytan D, Jegatheeswaran A, Mazwi ML, Assadi A, Goodwin AJ, Greer RW, Goodfellow SD, Laussen PC (2019) Temporal variability in the sampling of vital sign data limits the accuracy of patient state estimation. Pediatr Crit Care Med 20(7):e333–e341. https://doi.org/10.1097/pcc.0000000000001984
Rusin CG, Acosta SI, Shekerdemian LS, Vu EL, Bavare AC, Myers RB, Patterson LW, Brady KM, Penny DJ (2016) Prediction of imminent, severe deterioration of children with parallel circulations using real-time processing of physiologic data. J Thorac Cardiovasc Surg 152(1):171–177. https://doi.org/10.1016/j.jtcvs.2016.03.083
Ruiz VM, Saenz L, Lopez-Magallon A, Shields A, Ogoe HA, Suresh S, Munoz R, Tsui FR (2019) Early prediction of critical events for infants with single-ventricle physiology in critical care using routinely collected data. J Thorac Cardiovasc Surg 158(1):234–243.e233. https://doi.org/10.1016/j.jtcvs.2019.01.130
McKiernan CA, Lieberman SA (2005) Circulatory shock in children: an overview. Pediatr Rev 26(12):451–460. https://doi.org/10.1542/pir.26-12-451
Hatib F, Jian Z, Buddi S, Lee C, Settels J, Sibert K, Rinehart J, Cannesson M (2018) Machine-learning algorithm to predict hypotension based on high-fidelity arterial pressure waveform analysis. Anesthesiology. https://doi.org/10.1097/aln.0000000000002300
Benov A, Yaslowitz O, Hakim T, Amir-Keret R, Nadler R, Brand A, Glassberg E, Yitzhak A, Convertino VA, Paran H (2017) The effect of blood transfusion on compensatory reserve: a prospective clinical trial. J Trauma Acute Care Surg 83(1 Suppl 1):S71–S76. https://doi.org/10.1097/TA.0000000000001474
Hinojosa-Laborde C, Fernandez JRD, Muniz GW, Nawn CD, Burns RK, Le TH, Porter KB, Hardy JT, Convertino VA (2017) Effect of pain and analgesia on compensatory reserve. J Trauma Acute Care Surg 83(1 Suppl 1):S92–S97. https://doi.org/10.1097/TA.0000000000001544
Acknowledgements
The authors wish to thank the Children’s Hospital Colorado catheterization laboratory for their assistance with the study.
Funding
Development of the CRI algorithm was supported in part by funding from the US Army Medical Research and Material Command (USAMRMC) under Grant Nos. DM09027, W81XWH-15--2-0007, W81XWH-09-1-0750, W81XWH-09-C-0160, W81XWH-11-2-0091, W81XWH-11-2-0085, W81XWH-12-2-0112, and W81XWH-13-C-0121. The views, opinions, and/or findings contained in this manuscript are those of the authors and should not be construed as an official Department of the Army position, policy or decision unless so designated by other documentation. Additional support was provided by NIH/NCATS Colorado CTSA Grant Number UL1 TR002535. Contents are the authors’ sole responsibility and do not necessarily represent official NIH views.
Author information
Authors and Affiliations
Contributions
DEE: Concept/design, data analysis/interpretation, drafting article, critical revision of article, approval of article, data collection. DKL: Concept/design, data analysis/interpretation, critical revision of article, approval of article, data collection. RP: Critical revision of article, approval of article, data collection. NS: Critical revision of article, approval of article, data collection. KC: Statistics, critical revision of article, approval of article. MR: Concept/design, critical revision of article, approval of article. JEZ: Critical revision of article, approval of article. SLM: Critical revision of article, approval of article. GM: Concept/design, data analysis/interpretation, critical revision of article, approval of article. JSK: Concept/design, data analysis/interpretation, critical revision of article, approval of article, data collection.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Ehrmann and Kim have no conflicts of interests to declare. Dr. Moulton developed the compensatory reserve index algorithm utilized in this study. The underlying intellectual property is assigned to Flashback Technologies, Inc (Boulder, Colorado) and the Regents of the University of Colorado. Dr. Moulton licensed the technology from the University of Colorado and co-founded Flashback Technologies, Inc. Dr. Moulton is a consultant at Flashback Technologies, has an equity interest in the company, and receives royalty payments through the University of Colorado. Drs. Leopold, Morgan, Phillips, Shahi, Ross, Zablah, and Ms. Campbell have no conflicts of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Colorado Multi-Institutional Review Board at the University of Colorado) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ehrmann, D.E., Leopold, D.K., Phillips, R. et al. The Compensatory Reserve Index Responds to Acute Hemodynamic Changes in Patients with Congenital Heart Disease: A Proof of Concept Study. Pediatr Cardiol 41, 1190–1198 (2020). https://doi.org/10.1007/s00246-020-02374-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02374-3