Abstract
Background
Peripheral painful end-neuromas decrease quality of life significantly. Drug-resistant painful neuromas often require surgical treatment, nevertheless there is no actual gold standard.
Methods
We retrospectively analyzed 26 patients suffering from painful end-neuromas treated with neuroma excision followed by the perineural fat grafting (PFG). We evaluated the improvement in pain, disability, and quality of life on the long term.All patients were referred to our department between 2009 and 2017. “Visual analogue scale (VAS)”; “disability of the arm, shoulder, and hand (DASH)”; and “World Health Organization Quality of Life (WHOQOL) index” were systematically scored before each surgical intervention and re-evaluated after 24 months.
Results
The majority of neuromas were traumatic (n. 16; 62%) and involved the upper extremity (n. 21; 81%). Eight patients (31%) had already received a previous neuroma excision. After the neuroma excision followed by the PFG, pain decreased 4 points in the VAS scale on average (p < 0.001); disability improved 15 points in the DASH questionnaire (p < 0.001); the quality of life significantly improved in every WHOQOL index domain. Neuroma excision with PFG appeared equally effective both on patients with a primary or a relapsing neuroma.
Conclusions
Neuromectomy with perineural fat grafting is a simple, accessible, and effective technique in end-neuroma pain treatment, owning a low surgical risk and minimal donor site morbidity.
Level of evidence: Level III, therapeutic Study.


Similar content being viewed by others
References
Lu C, Sun X, Wang C, Wang Y, Peng J (2018) Mechanisms and treatment of painful neuromas. Rev Neurosci. https://doi.org/10.1515/revneuro-2017-0077
Taylor CA, Braza D, Rice JB, Dillingham T (2008) The incidence of peripheral nerve injury in extremity trauma. Am J Phys Med Rehabil 87(5):381–385
Baron R, Binder A, Wasner G (2010) Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. https://doi.org/10.1016/S1474-4422(10)70143-5
Krauss EM, Mackinnon SE, Laurido-Soto O et al (2016) Surgical treatment of neuromas improves patient-reported pain, depression, and quality of life. Plast Reconstr Surg 139(2):407–418
Sunderland S (1951) A classification of peripheral nerve injuries producing loss of function. Brain. https://doi.org/10.1093/brain/74.4.491
Chim H, Miller E, Gliniak C, Cohen ML, Guyuron B (2013) The role of different methods of nerve ablation in prevention of neuroma. Plast Reconstr Surg 131(5):1004–1012
Yao C, Zhou X, Zhao B, Sun C, Poonit K, Yan H (2017) Treatments of traumatic neuropathic pain: A systematic review. Oncotarget. https://doi.org/10.18632/oncotarget.16917
Evans GRD, Lee DA (1994) Implantation of the palmar cutaneous branch of the median nerve into the pronator quadratus for treatment of painful neuroma. J Hand Surg Am. https://doi.org/10.1016/0363-5023(94)90006-X
Pet MA, Ko JH, Friedly JL, Mourad PD, Smith DG (2014) Does targeted nerve implantation reduce neuroma pain in amputees? Clin Orthop Relat Res 472:2991–3001
Sood MK, Elliot D (1998) Treatment of painful neuromas of the hand and wrist by relocation into the pronator quadratus muscle. J Hand Surg Br. https://doi.org/10.1016/S0266-7681(98)80177-0
Stahl S, Rosenberg N (2003) Surgical treatment of painful neuroma in medial antebrachial cutaneous nerve. Ann Plast Surg. https://doi.org/10.1097/00000637-200202000-00007
Balcin H, Erba P, Wettstein R, Schaefer DJ, Pierer G, Kalbermatten DF (2009) A comparative study of two methods of surgical treatment for painful neuroma. J Bone Joint Surg (Br). https://doi.org/10.1302/0301-620X.91B6.22145
Koch H, Hubmer M, Welkerling H, Sandner-Kiesling A, Scharnagl E (2004) The treatment of painful neuroma on the lower extremity by resection and nerve stump transplantation into a vein. Foot Ankle Int. https://doi.org/10.1177/107110070402500706
Koch H, Haas F, Hubmer M, Rappl T, Scharnagl E (2003) Treatment of painful neuroma by resection and nerve stump transplantation into a vein. Ann Plast Surg. https://doi.org/10.1097/01.SAP.0000054187.72439.57
Thomsen L, Bellemere P, Loubersac T, Gaisne E, Poirier P, Chaise F (2010) Treatment by collagen conduit of painful post-traumatic neuromas of the sensitive digital nerve: a retrospective study of 10 cases. Chir Main. https://doi.org/10.1016/j.main.2010.07.004
Wagner E, Ortiz C (2011) The painful neuroma and the use of conduits. Foot Ankle Clin. https://doi.org/10.1016/j.fcl.2011.01.004
Krishnan KG, Pinzer T, Schackert G (2005) Coverage of painful peripheral nerve neuromas with vascularized soft tissue: method and results. Neurosurgery. https://doi.org/10.1227/01.NEU.0000156881.10388.D8
Adani R, Tos P, Tarallo L, Corain M (2014) Treatment of painful median nerve neuromas with radial and ulnar artery perforator adipofascial flaps. J Hand Surg Am. https://doi.org/10.1016/j.jhsa.2014.01.007
Peterson SL, Adham MN (2006) Acellular dermal matrix as an adjunct in treatment of neuropathic pain at the wrist. J Trauma. https://doi.org/10.1097/01.ta.0000224139.74143.f9
Louis DS, Hunter LY, Keating TM (1980) Painful neuromas in long below-elbow amputees. Arch Surg. https://doi.org/10.1001/archsurg.1980.01380060040010
Tay SC, Teoh LC, Yong FC, Tan SH (2005) The prevention of neuroma formation by diathermy: an experimental study in the rat common peroneal nerve. Ann Acad Med Singapore 34:362–368
Vora AR, Loescher AR, Boissonade FM, Robinson PP (2005) Ultrastructural characteristics of axons in traumatic neuromas of the human lingual nerve. J Orofac Pain 19:22–33
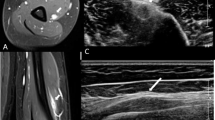
Vaienti L, Gazzola R, Villani F, Parodi PC (2012) Perineural fat grafting in the treatment of painful neuromas. Tech Hand Up Extrem Surg. https://doi.org/10.1097/BTH.0b013e31823cd218
Vaienti L, Merle M, Battiston B, Villani F, Gazzola R (2013) Perineural fat grafting in the treatment of painful end-neuromas of the upper limb: a pilot study. J Hand Surg Eur Vol. https://doi.org/10.1177/1753193412441122
Coleman SR (2002) Hand rejuvenation with structural fat grafting. Plast Reconstr Surg. https://doi.org/10.1097/00006534-200212000-00017
Norman Harden R, Bruehl SP (2006) Diagnosis of complex regional pain syndrome: signs, symptoms, and new empirically derived diagnostic criteria. Clin J Pain. https://doi.org/10.1097/01.ajp.0000194279.36261.3e
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). Am J Ind Med. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
Johnson EW (2001) Visual analog scale (VAS). Am J Phys Med Rehabil. https://doi.org/10.1097/00002060-200110000-00001
(2010) WHOQOL-BREF. In: Preedy VR, Watson RR (eds) Handbook of Disease Burdens and Quality of Life Measures. Springer, New York. https://doi.org/10.1007/978-0-387-78665-0_6927
Caviggioli F, Maione L, Forcellini D, Klinger F, Klinger M (2011) Autologous fat graft in postmastectomy pain syndrome. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0b013e31821e70e7
Maione L, Vinci V, Caviggioli F, Klinger F, Banzatti B, Catania B, Lisa A, Klinger M (2014) Autologous fat graft in postmastectomy pain syndrome following breast conservative surgery and radiotherapy. Aesthet Plast Surg 38:528–532
Caviggioli F, Maione L, Klinger F, Lisa A, Klinger M (2016) Autologous fat grafting reduces pain in irradiated breast: a review of our experience. Stem Cells Int. https://doi.org/10.1155/2016/2527349
Simonacci F, Bertozzi N, Grieco MP, Grignaffini E, Raposio E (2017) Procedure, applications, and outcomes of autologous fat grafting. Ann Med Surg (Lond). https://doi.org/10.1016/j.amsu.2017.06.059
Huang SH, Wu SH, Chang KP et al (2015) Alleviation of neuropathic scar pain using autologous fat grafting. Ann Plast Surg. https://doi.org/10.1097/SAP.0000000000000462
Fredman R, Edkins RE, Hultman CS (2016) Fat grafting for neuropathic pain after severe burns. Ann Plast Surg. https://doi.org/10.1097/SAP.0000000000000674
Negenborn VL, Groen JW, Smit JM, Niessen FB, Mullender MG (2016) The use of autologous fat grafting for treatment of scar tissue and scar-related conditions: a systematic review. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000001850
Balthasar AJR, Beugels J, Piatkowski de Grzymala AA, van der Hulst RRWJ, Hommes JE (2018) Autologous fat transfer as a treatment for peripheral neuropathic pain without apparent cause. Plast Reconstr Surg Glob Open. https://doi.org/10.1097/gox.0000000000001905
Mazzola RF, Cantarella G, Torretta S, Sbarbati A, Lazzari L, Pignataro L (2011) Autologous fat injection to face and neck: from soft tissue augmentation to regenerative medicine. Acta Otorhinolaryngologica Italica 31(2):59–69
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of I.R.C.C.S. Policlinico San Donato, Milan. However, for this kind of retrospective study a formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study. Data were treated anonymously.
Conflict of interest
L. Vaienti, F. Amendola, F. Borelli, G. Zaccaria, and G. Cottone declare that they have no conflict of interest.
Funding statement
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vaienti, L., Amendola, F., Borelli, F. et al. Perineural fat grafting in end-neuroma pain treatment: long-term outcomes. Eur J Plast Surg 44, 249–254 (2021). https://doi.org/10.1007/s00238-020-01664-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01664-6