Abstract
Purpose
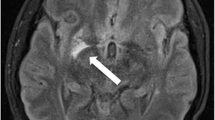
Neurosyphilis can mimic different diseases, not only in its clinical presentation but also on imaging. Treponema pallidum is also known as the “great imitator.” Having an ultimate diagnosis of neurosyphilis is quite critical as this can affect management drastically. Herein, we discuss the case of a 69-year-old female who was treated for neurosyphilis, while having an atypical imaging finding of anterior temporal lobe enhancement that simulated an infection with herpes simplex virus (HSV); we also review the available literature on different imaging findings in both the early and late stages of the disease.
Methods
We performed a literature search using the new PubMed in June 2021. The terms “neurosyphilis”, “MRI”, and “neuroimaging” were used either alone or in combination with “early neurosyphilis” or “late neurosyphilis”. Data on neurosyphilis and imaging findings was mainly derived from review articles, cohort studies, case series, and individual reports.
Conclusion
Neurosyphilis can present with an extensive variation and different patterns on the MRI, and clinicians must be aware of the wide variety in radiological presentations. Anterior temporal lobe involvement is a rare presentation and requires evaluating for neurosyphilis to prevent a missed diagnosis and treatment.


Similar content being viewed by others
Availability of data and material
All data is available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Change history
24 October 2021
The citation shows the author last name as Nour. However, the last name is Aboul Nour. This is now corrected.
References
Santana LM, Valadares E de JA, Rosa-Júnior M (2020) Differential diagnosis of temporal lobe lesions with hyperintense signal on T2-weighted and FLAIR sequences: pictorial essay. Radiol Bras. 53(2):129–136. https://doi.org/10.1590/0100-3984.2018.0117
Thibodeau R, Goel A, Jafroodifar A, Klumpp M, Mirchia K, Swarnkar A (2021) Cerebral syphilitic gumma presenting with intracranial gumma and pathologic vertebrae fractures. Radiol case reports 16(4):916–922. https://doi.org/10.1016/j.radcr.2021.01.056
Czarnowska-Cubała M, Wiglusz MS, Cubała WJ, Jakuszkowiak-Wojten K, Landowski J, Krysta K (2013) MR findings in neurosyphilis–a literature review with a focus on a practical approach to neuroimaging. Psychiatr Danub 25(Suppl 2):S153–S157
Ghanem KG (2010) REVIEW: Neurosyphilis: a historical perspective and review. CNS Neurosci Ther 16(5):e157–e168. https://doi.org/10.1111/j.1755-5949.2010.00183.x
Brightbill TC, Ihmeidan IH, Post MJ, Berger JR, Katz DA (1995) Neurosyphilis in HIV-positive and HIV-negative patients: neuroimaging findings. AJNR Am J Neuroradiol 16(4):703–711
Piura Y, Mina Y, Aizenstein O, Gadoth A (2019) Neurosyphilis presenting as cranial nerve palsy, an entity which is easy to miss. BMJ Case Rep. 12(2):e226509. https://doi.org/10.1136/bcr-2018-226509
Smith MM, Anderson JC (2000) Neurosyphilis as a cause of facial and vestibulocochlear nerve dysfunction: MR imaging features. AJNR Am J Neuroradiol 21(9):1673–1675
Iwamoto K, Aoyagi J, Kiyozuka T, Iwasaki Y, Fujioka T (2009) Neurosyphilis with unilateral optic tract lesion causing homonymous hemianopia. Neurologist 15(6):345–346. https://doi.org/10.1097/NRL.0b013e3181921b0a
Frohman L, Wolansky L (1997) Magnetic resonance imaging of syphilitic optic neuritis/perineuritis. J neuro-ophthalmology Off J North Am Neuro-Ophthalmology Soc 17(1):57–59
El Alaoui TK, Serrou A, AitBenhaddou E, Regragui W, Benomar A, Yahyaoui M (2013) Neurosyphilis revealed by trochlear nerve (IV) palsy. Rev Neurol (Paris) 169(3):279–280. https://doi.org/10.1016/j.neurol.2012.09.009
Hadrane L, Waterkeyn F, Ghijselings L, Dhaene N, Gille M (2008) Neurosyphilis revealed by a multiple cranial neuropathy: magnetic resonance imaging findings. Rev Neurol (Paris) 164(3):253–257. https://doi.org/10.1016/j.neurol.2007.08.001
Komamura H, Nakamura T, Kobayashi J et al (2019) Early neurosyphilis presenting with multiple cranial nerve palsies: a case report of management by combined penicillin-corticosteroid treatment. J Infect Chemother Off J Japan Soc Chemother 25(5):362–364. https://doi.org/10.1016/j.jiac.2018.11.007
Klein TAL, Ridley MB (2014) An old flame reignites: vagal neuropathy secondary to neurosyphilis. J Voice 28(2):255–257. https://doi.org/10.1016/j.jvoice.2013.08.018
Xia K, Guo Z, Xia X et al (2020) Multi-syphilitic gummas in pituitary and cerebellopontine angle in a patient. Pituitary 23(3):253–257. https://doi.org/10.1007/s11102-020-01033-3
Lee CW, Lim M-J, Son D et al (2009) A case of cerebral gumma presenting as brain tumor in a human immunodeficiency virus (HIV)-negative patient. Yonsei Med J 50(2):284–288. https://doi.org/10.3349/ymj.2009.50.2.284
Pollock JM, Greiner F, Lovelady C, Chernova T (2007) Neurosyphilis with unusual ring enhancement. Case illustration J Neurosurg 106(6):1107. https://doi.org/10.3171/jns.2007.106.6.1107
Fargen KM, Alvernia JE, Lin CS, Melgar M (2009) Cerebral syphilitic gummata: a case presentation and analysis of 156 reported cases. Neurosurgery 64(3):566–568. https://doi.org/10.1227/01.NEU.0000337079.12137.89
Li C, Wang S-J, Tang G-C, Liu L-T, Chen G-X (2019) Neuroimaging findings of cerebral syphilitic gumma. Exp Ther Med 18(6):4185–4192. https://doi.org/10.3892/etm.2019.8089
Biller J, Ferro JM (2014) Neurologic aspects of systemic disease. Part III Preface Handb Clin Neurol 121:ix. https://doi.org/10.1016/B978-0-7020-4088-7.09991-0
Elmouden H, Louhab N, Kissani N (2019) Medullary involvement in neurosyphilis: a report of 12 cases and a review of the literature. Spinal cord Ser cases 5:38. https://doi.org/10.1038/s41394-019-0185-9
Wu Y, Wu W (2020) Neurosyphilis presenting with myelitis-case series and literature review. J Infect Chemother Off J Japan Soc Chemother 26(2):296–299. https://doi.org/10.1016/j.jiac.2019.09.007
Pandey S (2011) Magnetic resonance imaging of the spinal cord in a man with tabes dorsalis. J Spinal Cord Med 34(6):609–611. https://doi.org/10.1179/2045772311Y.0000000041
Siu G (2017) Syphilitic meningomyelitis. J Am Osteopath Assoc 117(10):671. https://doi.org/10.7556/jaoa.2017.130
Skalnaya A, Fominykh V, Ivashchenko R et al (2019) Neurosyphilis in the modern era: literature review and case series. J Clin Neurosci Off J Neurosurg Soc Australas 69:67–73. https://doi.org/10.1016/j.jocn.2019.08.033
Bash S, Hathout GM, Cohen S (2001) Mesiotemporal T2-weighted hyperintensity: neurosyphilis mimicking herpes encephalitis. AJNR Am J Neuroradiol 22(2):314–316
Jeong YM, Hwang HY, Kim HS (2009) MRI of neurosyphilis presenting as mesiotemporal abnormalities: a case report. Korean J Radiol 10(3):310–312. https://doi.org/10.3348/kjr.2009.10.3.310
Xiang T, Li G, Xiao L et al (2013) Neuroimaging of six neurosyphilis cases mimicking viral encephalitis. J Neurol Sci 334(1–2):164–166. https://doi.org/10.1016/j.jns.2013.08.019
Fadil H, Gonzalez-Toledo E, Kelley BJ, Kelley RE (2006) Neuroimaging findings in neurosyphilis. J Neuroimaging 16(3):286–289. https://doi.org/10.1111/j.1552-6569.2006.00050.x
Omer TA, Fitzgerald DE, Sheehy N, Doherty CP (2012) Neurosyphilis presenting with unusual hippocampal abnormalities on magnetic resonance imaging and positron emission tomography scans: a case report. J Med Case Rep 6:389. https://doi.org/10.1186/1752-1947-6-389
Hama K, Ishiguchi H, Tuji T, Miwa H, Kondo T (2008) Neurosyphilis with mesiotemporal magnetic resonance imaging abnormalities. Intern Med 47(20):1813–1817. https://doi.org/10.2169/internalmedicine.47.0983
Agayeva N, Karli-Oguz K, Saka E (2013) Teaching NeuroImages: a neurosyphilis case presenting with atypical neuroradiologic findings. Neurology 80(11):e119. https://doi.org/10.1212/WNL.0b013e318287280b
Mignarri A, Arrigucci U, Coleschi P, Bilenchi R, Federico A, Dotti MT (2014) Temporal lobe abnormalities in neurosyphilis. Pract Neurol 14(6):449–450. https://doi.org/10.1136/practneurol-2014-000927
Beiruti K, Abu Awad A, Keigler G, Ryder CH, Shahien R (2019) Atypical development of neurosyphilis mimicking limbic encephalitis. Int J STD AIDS 30(2):194–197. https://doi.org/10.1177/0956462418797873
Denays R, Collier A, Rubinstein M, Atsama P (1999) A 51-year-old woman with disorientation and amnesia. Lancet (London, England) 354(9192):1786. https://doi.org/10.1016/S0140-6736(99)09151-5
Johns DR, Tierney M, Parker SW (1987) Pure motor hemiplegia due to meningovascular neurosyphilis. Arch Neurol 44(10):1062–1065. https://doi.org/10.1001/archneur.1987.00520220060018
Scolding NJ (2009) Central nervous system vasculitis. Semin Immunopathol 31(4):527–536. https://doi.org/10.1007/s00281-009-0183-2
Peng F, Hu X, Zhong X et al (2008) CT and MR findings in HIV-negative neurosyphilis. Eur J Radiol 66(1):1–6. https://doi.org/10.1016/j.ejrad.2007.05.018
Nagappa M, Sinha S, Taly AB et al (2013) Neurosyphilis: MRI features and their phenotypic correlation in a cohort of 35 patients from a tertiary care university hospital. Neuroradiology 55(4):379–388. https://doi.org/10.1007/s00234-012-1017-9
Gállego J, Soriano G, Zubieta JL, Delgado G, Villanueva JA (1994) Magnetic resonance angiography in meningovascular syphilis. Neuroradiology 36(3):208–209. https://doi.org/10.1007/BF00588132
Flint AC, Liberato BB, Anziska Y, Schantz-Dunn J, Wright CB (2005) Meningovascular syphilis as a cause of basilar artery stenosis. Neurology 64(2):391–392. https://doi.org/10.1212/01.WNL.0000149758.57386.B8
Feitoza L de M, Stucchi RSB, Reis F (2020) Neurosyphilis vasculitis manifesting as ischemic stroke. Rev Soc Bras Med Trop. 53:e20190546. https://doi.org/10.1590/0037-8682-0546-2019
Aldrich MS, Burke JM, Gulati SM (1983) Angiographic findings in a young man with recurrent stroke and positive fluorescent treponemal antibody (FTA). Stroke 14(6):1001–1004. https://doi.org/10.1161/01.str.14.6.1001
Holland BA, Perrett LV, Mills CM (1986) Meningovascular syphilis: CT and MR findings. Radiology 158(2):439–442. https://doi.org/10.1148/radiology.158.2.3941870
Pesaresi I, Sabato M, Doria R et al (2015) Susceptibility-weighted imaging in parenchymal neurosyphilis: identification of a new MRI finding. Sex Transm Infect 91(7):489–492. https://doi.org/10.1136/sextrans-2014-051961
Creech KT, Patel KM, Chaudhry U (2021) Tabes dorsalis in a patient presenting with right lower extremity paresthesia and cervical spine pain. Cureus 13(3):e14011. https://doi.org/10.7759/cureus.14011
Clark EG, Danbolt N (1955) The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material; a review and appraisal. J Chronic Dis 2(3):311–344. https://doi.org/10.1016/0021-9681(55)90139-9
Mehrabian S, Raycheva M, Traykova M et al (2012) Neurosyphilis with dementia and bilateral hippocampal atrophy on brain magnetic resonance imaging. BMC Neurol 12:96. https://doi.org/10.1186/1471-2377-12-96
Acknowledgements
The authors thank Karla D. Passalacqua, PhD, at Henry Ford Hospital for editorial services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethics approval
No institutional approval required for Case Reports.
Consent to participate
The subject included has given consent to participate.
Consent for publication
The subject included has given consent and agreed to the publication of the manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jum’ah, A., Aboul Nour, H., Alkhoujah, M. et al. Neurosyphilis in disguise. Neuroradiology 64, 433–441 (2022). https://doi.org/10.1007/s00234-021-02827-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02827-3