Abstract
Background and purpose
While numerous reports have demonstrated intracranial CNS anomalies associated with Klippel–Trenaunay syndrome, to our knowledge, there has not been a large consecutive study examining these anomalies. The aim of this study was to determine the spectrum of intracranial neurovascular manifestations in patients with a clinical diagnosis of Klippel–Tranaunay syndrome.
Methods
Consecutive patients with a clinical diagnosis of Klippel–Trenaunay syndrome, as defined by the International Society for the Study of Vascular Anomalies, who underwent brain contrast-enhanced CT/computed tomography angiography, MRI/magnetic resonance angiography, or digital subtraction angiography at our institution from 2000 to 2019 were included. Studies were evaluated by a neuroradiologist and a senior radiology resident for the presence of cavernous malformations, developmental venous anomalies, venous sinus developmental abnormalities, craniofacial venous malformations, intraosseous venous malformations, and intracranial/extracranial venous abnormalities.
Results
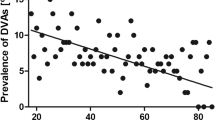
Fifty patients with definite KTS were included. Thirty-four neurovascular anomalies were found in 17 patients (34.0%), including 8 with multiple anomalies. Nine patients had developmental venous anomalies (18.0%), 7 had craniofacial venous malformations (14.0), 6 had venous sinus developmental abnormalities (12.0%), 7 had intraosseous venous malformations (14.0%), and 2 had cavernous malformations (4.0%), and 9 patients had both intracranial venous abnormalities and craniofacial or calvarial findings (13.0%).
Conclusion
Our findings demonstrate that Klippel–Trenaunay syndrome can involve a wide spectrum of intracranial neurovascular anomalies predominantly involving the venous system






Similar content being viewed by others
Abbreviations
- DVA:
-
Developmental venous anomaly
- ISSVA:
-
International Society for the Study of Vascular Anomalies
- KTS:
-
Klippel–Trenaunay syndrome
References
ISSVA Classification of Vascular Anomalies ©2018 International Society for the Study of Vascular Anomalies https://www.issva.org/UserFiles/file/ISSVA-Classification-2018.pdf Accessed 2/4/2020.
John PR (2019) Klippel-Trenaunay syndrome. Tech Vasc Interv Radiol 22(4):100634. https://doi.org/10.1016/j.tvir.2019.100634
Saleem MA, Zahra NE, Hemani F, Jan Ali A, Gilani A (2019) Cerebral cavernous angioma associated with Klippel Trenaunay syndrome treated with gamma knife radiosurgery: case report and literature review. Cureus 11(3):e4318. https://doi.org/10.7759/cureus.4318
Boutarbouch M, Ben Salem D, Gire L, Giroud M, Bejot Y, Ricolfi F (2010) Multiple cerebral and spinal cord cavernomas in Klippel-Trenaunay-Weber syndrome. J Clin Neurosci 17(8):1073–1075. https://doi.org/10.1016/j.jocn.2009.11.013
Kiley MA, Oxbury JM, Coley SC. Intracranial hypertension in Sturge-Weber/Klippel-Trenaunay-Weber overlap syndrome due to impairment of cerebral venous outflow. J Clin Neurosci 2002;9(3):330-3. https://doi.org/10.1054/jocn.2001.1041, 333.
Rathbun JE, Hoyt WF, Beard C (1970) Surgical management of orbitofrontal varix in Klippel-Trenaunay-Weber syndrome. Am J Ophthalmol 70(1):109–112. https://doi.org/10.1016/0002-9394(70)90675-6
Star A, Fuller CE, Landas SK (2010) Intracranial aneurysms in Klippel-Trenaunay/Weber syndromes: case report. Neurosurgery 66(5):E1027–E1028; discussion E8. https://doi.org/10.1227/01.neu.0000368392.69904.be
Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, Drayer BP, Brown B, Rigamonti D, Brown G (1994) The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg 80(3):422–432. https://doi.org/10.3171/jns.1994.80.3.0422
Brinjikji W, El-Rida El-Masri A, Wald JT, Lanzino G (2017) Prevalence of developmental venous anomalies increases with age. Stroke. 48(7):1997–1999. https://doi.org/10.1161/strokeaha.116.016145
Limaye N, Kangas J, Mendola A, Godfraind C, Schlogel MJ, Helaers R et al (2015) Somatic Activating PIK3CA mutations cause venous malformation. Am J Hum Genet 97(6):914–921. https://doi.org/10.1016/j.ajhg.2015.11.011
Brinjikji W, Hilditch CA, Tsang AC, Nicholson PJ, Krings T, Agid R (2018) Facial venous malformations are associated with cerebral developmental venous anomalies. AJNR Am J Neuroradiol 39(11):2103–2107. https://doi.org/10.3174/ajnr.A5811
Roux A, Boddaert N, Grill J, Castel D, Zanello M, Zah-Bi G, Chrétien F, Lefevre E, Ros VD, Zerah M, Puget S, Pallud J, Varlet P (2020) High prevalence of developmental venous anomaly in diffuse intrinsic pontine gliomas: a pediatric control study. Neurosurgery. 86(4):517–523. https://doi.org/10.1093/neuros/nyz298
Roux A, Edjlali M, Porelli S, Tauziede-Espariat A, Zanello M, Dezamis E, Zah-Bi G, Sanson M, Puget S, Capelle L, Varlet P, Oppenheim C, Pallud J (2019) Developmental venous anomaly in adult patients with diffuse glioma: a clinically relevant coexistence? Neurology. 92(1):e55–e62. https://doi.org/10.1212/wnl.0000000000006690
Roux A, Vikkula M, Pallud J (2020) Letter: Is developmental venous anomaly an imaging biomarker of PIK3CA mutated gliomas? Neurosurgery. 86(1):E93. https://doi.org/10.1093/neuros/nyz425
van der Loo LE, Beckervordersandforth J, Colon AJ, Schijns OE (2017) Growing skull hemangioma: first and unique description in a patient with Klippel-Trenaunay-Weber syndrome. Acta Neurochir 159(2):397–400. https://doi.org/10.1007/s00701-016-3012-0
Karadag A, Senoglu M, Sayhan S, Okromelidze L, Middlebrooks EH (2019) Klippel-Trenaunay-Weber syndrome with atypical presentation of cerebral cavernous angioma: a case report and literature review. World Neurosurg 126:354–358. https://doi.org/10.1016/j.wneu.2019.03.132
Yoshinaga T, Yagi K, Morishita T, Abe H, Nonaka M, Inoue T (2018) Cerebral and spinal cavernomas associated with Klippel-Trenaunay syndrome: case report and literature review. Acta Neurochir 160(2):287–290. https://doi.org/10.1007/s00701-017-3408-5
Flemming KD, Lanzino G (2020) Cerebral cavernous malformation: what a practicing clinician should know. Mayo Clin Proc 95:2005–2020. https://doi.org/10.1016/j.mayocp.2019.11.005
Brinjikji W, Nicholson P, Hilditch CA, Krings T, Pereira V, Agid R (2020) Cerebrofacial venous metameric syndrome-spectrum of imaging findings. Neuroradiology. 62:417–425. https://doi.org/10.1007/s00234-020-02362-7
Colletti G, Ierardi AM (2017) Understanding venous malformations of the head and neck: a comprehensive insight. Med Oncol 34(3):42. https://doi.org/10.1007/s12032-017-0896-3
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Presentation: This work has not been heretofore presented.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Covington, T.N., Anderson, K.R., Tollefson, M.M. et al. Intracranial and extracranial vascular manifestations of patients with a clinical diagnosis of Klippel–Trenaunay syndrome. Neuroradiology 63, 409–415 (2021). https://doi.org/10.1007/s00234-020-02560-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02560-3