Abstract
Purpose
The trial aimed to investigate the effectiveness of exogenous melatonin as an adjuvant to pregabalin for relief of pain in patients suffering from painful diabetic neuropathy (PDN).
Patients and methods
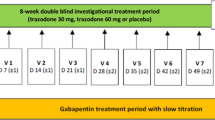
This randomized, double-blind, placebo-controlled trial was carried out between October 2019 and December 2020 in an outpatient specialty clinic in Iran. One-hundred-three type 2 diabetic patients suffering from PDN were randomized into either the melatonin group (n = 52) or the placebo group (n = 51). Besides pregabalin at a dose of 150 mg per day, patients started with melatonin or an identical placebo, at a dose of 3 mg/day at bedtime for 1 week, which was augmented to 6 mg/day for further 7 weeks. The primary outcomes were changes in mean NRS (numerical rating scale) pain score from baseline to endpoint and responder rate (patients with a reduction of 50% and higher in average pain score compared with baseline). Secondary endpoints were changes in mean NRS pain-related sleep-interference score, overall improvement evaluated by Patient and Clinical Global Impressions of Change (PGIC, CGIC), and impact of the intervention on patient’s Health-related quality of life (QOL). All analyses were conducted on an Intention-to-Treat (ITT) analysis data set.
Results
At the study endpoint, treatment with melatonin resulted in a considerably higher reduction in the mean NRS pain score in comparison with placebo (4.2 ± 1.83 vs. 2.9 ± 1.56; P-value < 0.001). In terms of treatment responders, a greater proportion of melatonin-treated patients satisfied the responder criterion than placebo-treated patients (63.5% vs. 43.1%). Melatonin also reduced pain-related sleep interference scores more than did placebo (3.38 ± 1.49 vs. 2.25 ± 1.26; P-value < 0.001). Further, at the endpoint, more improvement was also seen in terms of PGIC, CGIC, and Health-related QOL in patients treated with melatonin than placebo. Melatonin was also well tolerated.
Conclusion
The present results showed that melatonin as an adjunct therapy to pregabalin might be helpful for use in patients with PDN. However, confirmation of these results requires further studies.



Similar content being viewed by others
Availability of data and material
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request up to 2 years after publication.
References
Iqbal Z, Azmi S, Yadav R, Ferdousi M, Kumar M, Cuthbertson DJ, Lim J, Malik RA, Alam U (2018) Diabetic peripheral neuropathy: epidemiology diagnosis and pharmacotherapy. Clin Ther 40(6):828–849
Caputo GM, Cavanagh PR, Ulbrecht JS, Gibbons GW, Karchmer AW (1994) Assessment and management of foot disease in patients with diabetes. N Engl J Med 331(13):854–860
Llewelyn JG (2003) The diabetic neuropathies: types diagnosis and management. J Neurol Neurosurg Psychiatry 74(2):ii15–ii19
Tesfaye S, Boulton AJ, Dickenson AH (2013) Mechanisms and management of diabetic painful distal symmetrical polyneuropathy. Diabetes Care 36(9):2456–2465
Benbow S, Wallymahmed M, MacFarlane I (1998) Diabetic peripheral neuropathy and quality of life. J Assoc Physicians 91(11):733–737
Quattrini C, Tesfaye S (2003) Understanding the impact of painful diabetic neuropathy. Diabetes Metab Res Rev 19(S1):S2–S8
Spallone V (2012) Management of painful diabetic neuropathy: guideline guidance or jungle? Curr DiabRep 12(4):403–413
Tajti J, Szok D, Majláth Z, Csáti A, Petrovics-Balog A, Vécsei L (2016) Alleviation of pain in painful diabetic neuropathy. Expert Opin Drug Metab Toxicol 12(7):753–764
Aslam A, Singh J, Rajbhandari S (2014) Pathogenesis of painful diabetic neuropathy. Pain Res Manag 2014
Stemkowski PL, Smith PA (2012) Sensory neurons ion channels inflammation and the onset of neuropathic pain. Can J Neurol Sci 39(4):416–435
Debnath M, Agrawal S (2016) Diabetic neuropathy: Oxidative stress and neuroinflammation. Med Res 3(8):237-241
Bandeira DM, Da Fonseca LJS, Guedes DS, Rabelo LA, Goulart MO, Vasconcelos SML (2013) Oxidative stress as an underlying contributor in the development of chronic complications in diabetes mellitus. Int J Mol Sci 14(2):3265–3284
Sandireddy R, Yerra VG, Areti A, Komirishetty P, Kumar A (2014) Neuroinflammation and oxidative stress in diabetic neuropathy: futuristic strategies based on these targets. Int J Endocrinol 2014
Sytze van Dam P (2002) Oxidative stress and diabetic neuropathy: pathophysiological mechanisms and treatment perspectives. Diabetes Metab Res Rev 18(3):176–184
Pevet P, Challet E (2011) Melatonin: both master clock output and internal time-giver in the circadian clocks network. Journal of Physiology-Paris 105(4–6):170–182
Emet M, Ozcan H, Yayla M, Halici Z, Hacimuftuoglu A (2016) A review of melatonin its receptors and drugs. The Eurasian journal of medicine 48(2):135
Kostoglou-Athanassiou I (2013) Therapeutic applications of melatonin. Therapeutic advances in endocrinology and metabolism 4(1):13–24
Kuthati Y, Lin SH, Chen J, Wong CS (2019) Melatonin and their analogs as a potential use in the management of neuropathic pain. J Formos Med Assoc 118(8):1177–1186
Chen WW, Zhang X, Huang WJ (2016) Pain control by melatonin: physiological and pharmacological effects. Exp Ther Med 12(4):1963–1968
Kundermann B, Krieg JC, Schreiber W, Lautenbacher S (2004) The effects of sleep deprivation on pain. Pain Res Manag 9(1):25–32
Wang YS, Li YY, Cui W, Li LB, Zhang ZC, Tian BP, Zhang GS (2017) Melatonin attenuates pain hypersensitivity and decreases astrocyte-mediated spinal neuroinflammation in a rat model of oxaliplatin-induced pain. Inflammation 40(6):2052–2061
Kumar A, Meena S, Kalonia H, Gupta A, Kumar P: Effect of nitric oxide in protective effect of melatonin against chronic constriction sciatic nerve injury induced neuropathic pain in rats. Indian J Exp Biol. 2011 Sep; 49(9):664-71.
de Heer EW, Gerrits MM, Beekman AT, Dekker J, van Marwijk HW, de Waal MW, Spinhoven P, Penninx BW, van der Feltz-Cornelis CM (2014) The association of depression and anxiety with pain: a study from NESDA. PloS one 9(10):e106907
Yousaf F, Seet E, Venkatraghavan L, Abrishami A, Chung F, Warner DS (2010) Efficacy and safety of melatonin as an anxiolytic and analgesic in the perioperative period: a qualitative systematic review of randomized trials. The Journal of the American Society of Anesthesiologists 113(4):968–976
Melzack R (1987) The Short-Form Mcgill Pain Questionnaire. Pain 30(2):191–197
Hurst H, Bolton J (2004) Assessing the clinical significance of change scores recorded on subjective outcome measures. J Manipulative Physiol Ther 27(1):26–35
Ware JE (1992) A 36-Item Short-Form Health Survey (SF-36) I: conceptual framework and item selection. Med Care 30:476–483
Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B (2005) The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res 14(3):875–882
Boga JA, Caballero B, Potes Y, Perez-Martinez Z, Reiter RJ, Vega-Naredo I, Coto-Montes A (2019) Therapeutic potential of melatonin related to its role as an autophagy regulator: a review. J Pineal Res 66(1):e12534
Onaolapo AY, Onaolapo OJ (2018) Circadian dysrhythmia-linked diabetes mellitus: examining melatonin’s roles in prophylaxis and management. World J Diabetes 9(7):99
Pourhanifeh MH, Hosseinzadeh A, Dehdashtian E, Hemati K, Mehrzadi S (2020) Melatonin: new insights on its therapeutic properties in diabetic complications. Diabetol Metab Syndr 12:1–20
Danilov A, Kurganova J (2016) Melatonin in chronic pain syndromes. Pain Ther 5(1):1–17
Sivertsen B, Lallukka T, Petrie KJ, Steingrímsdóttir ÓA, Stubhaug A, Nielsen CS (2015) Sleep and pain sensitivity in adults. Pain 156(8):1433–1439
Chiu Y, Silman A, MacFarlane GJ, Ray D, Gupta A, Dickens C, Morriss R, McBeth J (2005) Poor sleep and depression are independently associated with a reduced pain threshold. Results of a population based study. Pain 115(3):316–321
Narita M, Niikura K, Nanjo-Niikura K, Narita M, Furuya M, Yamashita A, Saeki M, Matsushima Y, Imai S, Shimizu T (2011) Sleep disturbances in a neuropathic pain-like condition in the mouse are associated with altered GABAergic transmission in the cingulate cortex. Pain 152(6):1358–1372
Perissin L, Boccalon S, Scaggiante B, Petrelli L, Ortolani F, Porro CA (2004) Diurnal changes of tonic nociceptive responses in mice: evidence for a proalgesic role of melatonin. Pain 110(1–2):250–258
Hastings MH, Goedert M (2013) Circadian clocks and neurodegenerative diseases: time to aggregate? Curr Opin Neurobiol 23(5):880–887
Melikoglu MA, Celik A (2017) Does neuropathic pain affect the quality of sleep? The Eurasian journal of medicine 49(1):40
Golombek DA, Escolar E, Burin LJ, Sánchez MGDB, Cardinali DP (1991) Time-dependent melatonin analgesia in mice: inhibition by opiate or benzodiazepine antagonism. Eur J Pharmacol 194(1):25–30
Lakin M, Miller C, Stott M, Winters W (1981) Involvement of the pineal gland and melatonin in murine analgesia. Life Sci 29(24):2543–2551
Odo M, Koh K, Takada T, Yamashita A, Narita M, Kuzumaki N, Ikegami D, Sakai H, Iseki M, Inada E (2014) Changes in circadian rhythm for mRNA expression of melatonin 1A and 1B receptors in the hypothalamus under a neuropathic pain-like state. Synapse 68(4):153–158
Jensen TS, Finnerup NB (2014) Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. The Lancet Neurology 13(9):924–935
Huang CT, Chiang RPY, Chen CL, Tsai YJ (2014) Sleep deprivation aggravates median nerve injury-induced neuropathic pain and enhances microglial activation by suppressing melatonin secretion. Sleep 37(9):1513–1523
Ambriz-Tututi M, Granados-Soto V (2007) Oral and spinal melatonin reduces tactile allodynia in rats via activation of MT2 and opioid receptors. Pain 132(3):273–280
Tu Y, Sun RQ, Willis WD (2004) Effects of intrathecal injections of melatonin analogs on capsaicin-induced secondary mechanical allodynia and hyperalgesia in rats. Pain 109(3):340–350
Onal SA, Inalkac S, Kutlu S, Kelestimur H (2004) Intrathecal melatonin increases the mechanical nociceptive threshold in the rat. The Journal of the Turkish Society of Algology 16(4):35–40
Wang S, Zhang L, Lim G, Sung B, Tian Y, Chou CW, Hernstadt H, Rusanescu G, Ma Y, Mao J (2009) A combined effect of dextromethorphan and melatonin on neuropathic pain behavior in rats. Brain Res 1288:42–49
Ulugol A, Dokmeci D, Guray G, Sapolyo N, Ozyigit F, Tamer M (2006) Antihyperalgesic but not antiallodynic effect of melatonin in nerve-injured neuropathic mice: possible involvements of the L-arginine NO pathway and opioid system. Life Sci 78(14):1592–1597
Zurowski D, Nowak L, Machowska A, Wordliczek J, Thor P (2012) Exogenous melatonin abolishes mechanical allodynia but not thermal hyperalgesia in neuropathic pain: The role of the opioid system and benzodiazepine-gabaergic mechanism. J Physiol Pharmacol 63(6):641–647
Zangiabadi N, Sheibani V, Asadi-Shekaari M, Shabani M, Jafari M, Asadi AR, Tajadini H, Jarahi M (2011) Effects of melatonin in prevention of neuropathy in STZ-induced diabetic rats. Am J Pharmacol Toxicol 6(2):59–67
Babaei-Balderlou F, Ilkhanipour M, Heidari R, Zare S, Bernousi I (2009) Effect of melatonin on peripheral neuropathic pain in diabetic rat. Iranian Journal of Endocrinology and Metabolism 11(1):79–87
Kahya MC, Nazıroğlu M, Övey İS (2017) Modulation of diabetes-induced oxidative stress apoptosis and Ca2+ entry through TRPM2 and TRPV1 channels in dorsal root ganglion and hippocampus of diabetic rats by melatonin and selenium. Mol Neurobiol 54(3):2345–2360
Seyit D, Degirmenci E, Oguzhanoglu A (2016) Evaluation of electrophysiological effects of melatonin and alpha lipoic acid in rats with streptozotocine induced diabetic neuropathy. Exp Clin Endocrinol Diabetes 124(05):300–306
Babaei-Balderlou F, Zare S (2012) Melatonin improves spatial navigation memory in male diabetic rats. In: Veterinary Research Forum: 2012: Faculty of Veterinary Medicine, Urmia University, Urmia, Iran; 187
Metwally MM, Ebraheim LL, Galal AA (2018) Potential therapeutic role of melatonin on STZ-induced diabetic central neuropathy: a biochemical histopathological immunohistochemical and ultrastructural study. Acta Histochem 120(8):828–836
Afifi NM (2013) Neuroprotective effect of melatonin in a rat model of streptozotocin-induced diabetic neuropathy: light and electron microscopic study. Egyptian Journal of Histology 36(2):321–335
Zhu C, Xu Y, Duan Y, Li W, Zhang L, Huang Y, Zhao W, Wang Y, Li J, Feng T (2017) Exogenous melatonin in the treatment of pain: a systematic review and meta-analysis. Oncotarget 8(59):100582
Altiparmak B, Cil H, Celebi N (2019) Effect of melatonin on the daytime sleepiness side-effect of gabapentin in adults patients with neuropathic pain. Rev Bras Anestesiol 69(2):137–143
Lopez-Canul M, Palazzo E, Dominguez-Lopez S, Luongo L, Lacoste B, Comai S, Angeloni D, Fraschini F, Boccella S, Spadoni G (2015) Selective melatonin MT2 receptor ligands relieve neuropathic pain through modulation of brainstem descending antinociceptive pathways. Pain 156(2):305–317
Posa L, De Gregorio D, Gobbi G, Comai S (2018) Targeting melatonin MT2 receptors: a novel pharmacological avenue for inflammatory and neuropathic pain. Curr Med Chem 25(32):3866–3882
Gobbi G, Lopez-Canul M, Palazzo E, Dominguez-Lopez S, Luongo L, Lacoste B, Comai S, Angeloni D, Fraschini F, Spadoni G (2016) PT628: First in class melatonin MT2 receptors agonists for neuropathic pain. Int J Neuropsychopharmacol 19(1):30
López-Canul M, Comai S, Domínguez-López S, Granados-Soto V, Gobbi G (2015) Antinociceptive properties of selective MT2 melatonin receptor partial agonists. Eur J Pharmacol 764:424–432
Wu FS, Yang YC, Tsai JJ (1999) Melatonin potentiates the GABAA receptor-mediated current in cultured chick spinal cord neurons. Neurosci Lett 260(3):177–180
Wan Q, Man H-Y, Liu F, Braunton J, Niznik HB, Pang SF, Brown GM, Wang YT (1999) Differential modulation of GABA A receptor function by Mel 1a and Mel 1b receptors. Nat Neurosci 2(5):401–403
Xu F, Li J, Ma K, Wang M (1995) Effects of melatonin on hypothalamic γ-aminobutyric acid aspartic acid glutamic acid β-endorphin and serotonin levels in male mice. Neurosignals 4(4):225–231
Ebadi M, Govitrapong P, Phansuwan-Pujitu P, Nelson F, Reiter RJ (1998) Pineal opioid receptors and analgesic action of melatonin. J Pineal Res 24(4):193–200
Dai X, Cui S-g, Li S-r, Chen Q, Wang R (2007) Melatonin attenuates the development of antinociceptive tolerance to delta- but not to mu-opioid receptor agonist in mice. Behav Brain Res 182(1):21–27
Wang J, Wang L, Li M, Jin Q, Dong S (2011) Preliminary analgesic properties of deltorphin-5-methoxytryptamine chimeric opioid peptides. Peptides 32(5):1055–1059
Arreola-Espino R, Urquiza-Marín H, Ambriz-Tututi M, Araiza-Saldaña CI, Caram-Salas NL, Rocha-González HI, Mixcoatl-Zecuatl T, Granados-Soto V (2007) Melatonin reduces formalin-induced nociception and tactile allodynia in diabetic rats. Eur J Pharmacol 577(1–3):203–210
Shavali S, Ho B, Govitrapong P, Sawlom S, Ajjimaporn A, Klongpanichapak S, Ebadi M (2005) Melatonin exerts its analgesic actions not by binding to opioid receptor subtypes but by increasing the release of β-endorphin an endogenous opioid. Brain Res Bull 64(6):471–479
Zhou HY, Chen SR, Pan HL (2011) Targeting N-methyl-D-aspartate receptors for treatment of neuropathic pain. Expert Rev Clin Pharmacol 4(3):379–388
Xu F, Zhao X, Liu H, Shao X, Chu S, Gong X, Ma Z, Gu X (2018) Misaligned feeding may aggravate pain by disruption of sleep-awake rhythm. Anesth Analg 127(1):255–262
Escames G, Leon J, Lopez L, Acuña-Castroviejo D (2004) Mechanisms of N-methyl-D-aspartate receptor inhibition by melatonin in the rat striatum. J Neuroendocrinol 16(11):929–935
Borsani E, Buffoli B, Bonazza V, Reiter RJ, Rezzani R, Rodella LF (2017) Single administration of melatonin modulates the nitroxidergic system at the peripheral level and reduces thermal nociceptive hypersensitivity in neuropathic rats. Int J Mol Sci 18(10):2143
Negi G, Kumar A, Sharma SS (2011) Melatonin modulates neuroinflammation and oxidative stress in experimental diabetic neuropathy: effects on NF-κB and Nrf2 cascades. J Pineal Res 50(2):124–131
Tsuda M, Mizokoshi A, Shigemoto-Mogami Y, Koizumi S, Inoue K (2004) Activation of p38 mitogen-activated protein kinase in spinal hyperactive microglia contributes to pain hypersensitivity following peripheral nerve injury. Glia 45(1):89–95
Jin SX, Zhuang ZY, Woolf CJ, Ji RR (2003) p38 mitogen-activated protein kinase is activated after a spinal nerve ligation in spinal cord microglia and dorsal root ganglion neurons and contributes to the generation of neuropathic pain. J Neurosci 23(10):4017–4022
Esposito E, Paterniti I, Mazzon E, Bramanti P, Cuzzocrea S (2010) Melatonin reduces hyperalgesia associated with inflammation. J Pineal Res 49(4):321–331
Chiang RPY, Huang CT, Tsai YJ (2013) Melatonin reduces median nerve injury-induced mechanical hypersensitivity via inhibition of microglial p38 mitogen-activated protein kinase activation in rat cuneate nucleus. J Pineal Res 54(2):232–244
Hernández-Beltrán N, Moreno CB, Gutiérrez-Álvarez ÁM (2013) Contribution of mitochondria to pain in diabetic neuropathy. Endocrinología y Nutrición (English Edition) 60(1):25–32
Galley HF, McCormick B, Wilson KL, Lowes DA, Colvin L, Torsney C (2017) Melatonin limits paclitaxel-induced mitochondrial dysfunction in vitro and protects against paclitaxel-induced neuropathic pain in the rat. J Pineal Res 63(4):e12444
Yang CH, Yip HK, Chen HF, Yin TC, Chiang JY, Sung PH, Lin KC, Tsou YH, Chen YL, Li YC (2019) Long-term therapeutic effects of extracorporeal shock wave-assisted melatonin therapy on mononeuropathic pain in rats. Neurochem Res 44(4):796–810
Chaudhary S, Parvez S (2018) Valproic acid induced neurotoxicological manifestations and its mitigation by melatonin in rat brain synaptosomes. Arch Med Res 49(7):441–450
Mantovani M, Kaster MP, Pertile R, Calixto JB, Rodrigues ALS, Santos AR (2006) Mechanisms involved in the antinociception caused by melatonin in mice. J Pineal Res 41(4):382–389
Shin DJ, Jeong CW, Lee SH, Yoon MH (2011) Receptors involved in the antinociception of intrathecal melatonin in formalin test of rats. Neurosci Lett 494(3):207–210
M’dahoma S, Poitevin M, Dabala E, Payan H, Gabriel C, Mocaër E, Bourgoin S, Hamon M, (2018) α2-and β2-adrenoreceptor-mediated efficacy of the atypical antidepressant agomelatine combined with gabapentin to suppress allodynia in neuropathic rats with ligated infraorbital or sciatic nerve. Front Pharmacol 9:587
Andersen LPH, Gögenur I, Rosenberg J, Reiter RJ (2016) The safety of melatonin in humans. Clin Drug Investig 36(3):169–175
Acknowledgements
Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences is acknowledged here for supporting this study (Hamadan, Iran, Grant Number: 9808286522). This grant was just for the provision of medicine and placebo and was not assigned to the manuscript writing, editing, and publication fee. The authors thank all patients for helping and participating in the study.
Funding
Vice-Chancellor of Research and Technology of Hamadan University of Medical Sciences provided support for this study (Hamadan, Iran, Grant Number: 9808286522). This grant was just for the provision of medicine and placebo and was not assigned to the manuscript writing, editing, and publication fee.
Author information
Authors and Affiliations
Contributions
Conceptualization: Mehrpooya and Shokri; methodology: Mehrpooya, Shokri, Mohammadi, and Sajedi; data acquisition: Sajedi and Shokri; statistical analysis: Mohammadi; writing—original draft preparation: Shokri; writing—review and editing: Mehrpooya and Mohammadi; interpretation of the results and approval of the final manuscript: all authors.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shokri, M., Sajedi, F., Mohammadi, Y. et al. Adjuvant use of melatonin for relieving symptoms of painful diabetic neuropathy: results of a randomized, double-blinded, controlled trial. Eur J Clin Pharmacol 77, 1649–1663 (2021). https://doi.org/10.1007/s00228-021-03170-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03170-5