Abstract
Purpose
Two to seven percent of the German adult population has a renal impairment (RI) with an estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2. This often remains unrecognized and adjustment of drug therapy is lacking. To determine renal function in clinical routine, the CKD-EPI equation is used to calculate an indexed eGFR (ml/min/1.73m2). For drug dosing, it has to be individualized to a non-indexed eGFR (ml/min) by the patient’s body surface area. Here, we investigated the number of patients admitted to urological wards of a teaching hospital with RI between July and December 2016. Additionally, we correctly used the eGFRnon-indexed for drug and dosage adjustments and to analyse the use of renal risk drugs (RRD) and renal drug-related problems (rDRP).
Methods
In a retrospective observational study, urological patients with pharmacist-led medication reconciliation at hospital admission and eGFRindexed (CKD-EPI) of 15–59 ml/min/1.73m2 were identified. Indexed eGFR (ml/min/1.73m2) was recalculated with body surface area to non-indexed eGFR (ml/min) for correct drug dosing. Medication at admission was reviewed for RRD and based on the eGFRnon-indexed for rDRP, e.g. inappropriate dose or contraindication.
Results
Of 1320 screened patients, 270 (20.5%) presented with an eGFRindexed of 15–59 ml/min/1.73m2. After readjustment, 203 (15.4%) patients had an eGFRnon-indexed of 15–59 ml/min. Of these, 190 (93.6%) used ≥ 1 drugs at admission with 660 of 1209 (54.7%) drugs classified as RRD. At least one rDRP was identified in 115 (60.5%) patients concerning 264 (21.8%) drugs.
Conclusion
Renal impairment is a common risk factor for medication safety in urologic patients admitted to a hospital. Considerable shifts were seen in eGFR-categories when correctly calculating eGFRnon-indexed for drug dosing purposes. The fact that more than half of the study patients showed rDRP at hospital admission underlines the need to consider this risk factor appropriately.
Similar content being viewed by others
Introduction
Renal impairment (RI), defined as an estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73m2 [1], is a relevant health issue in Germany. About 2–7% of the adult population are affected rising to 15–25% in patients aged over 60 years [1,2,3]. Unfortunately, in 72% of these patients, the RI remains unrecognized and only two-thirds of those, who are aware, are in medical care [2]. Adjustment of drug therapy is an important issue of patient safety in this patient group to avoid adverse drug reactions (ADR).
‘Renal risk drugs’ (RRD) either show altered pharmacokinetics or pharmacodynamics in RI or directly affect renal function [3, 4]. Dosage reduction and discontinuation of the drug or possibly harmful drug combinations have to be considered to avoid accumulation or nephrotoxicity, potentially leading to ADR [5, 6]. Additionally, drug activation (e.g. vitamin D) or pharmacological effectiveness (e.g. thiazides) may be influenced by RI [7, 8]. Inappropriate or missing adjustment of RRD to renal function may cause renal drug-related problems (rDRP). Many rDRP are preventable if renal function is consequently considered. However, poor awareness of pre-existing RI and incorrect use of equations for renal function is still a problem. The use of potentially inappropriate drugs and dosages is common in patients with RI [9,10,11,12], increasing the rate of ADR [13,14,15,16].
In routine clinical practice, renal function is mostly determined using the endogenous filtration marker creatinine to calculate an eGFR or an estimated creatinine clearance (Fig. S1) [9].
To stage chronic kidney disease (CKD) for diagnosis, prognosis and treatment, the Kidney Disease Improving Global Outcomes Initiative (KDIGO) recommends the calculation of eGFR using the CKD Epidemiology Collaboration (CKD-EPI) equation and graduates eGFR in six categories [1, 17, 18]. CKD-EPI-equation estimates GFRindexed for a standard body surface area (BSA) of 1.73 m2 and can be used to compare renal function regardless of the individual’s size and weight. Importantly, for drug dosing, the GFRindexed should be individualized for every patient to the units ml/min by adjusting for the BSA calculated from actual weight and height (eGFRnon-indexed) [1, 18, 19]. This is of special importance for patients whose BSA differs significantly from 1.73 m2 and for drugs with a narrow therapeutic index, yet since eGFRindexed is calculated automatically by many clinical laboratories, physicians tend to incorrectly use this parameter for drug dosing.
In comparison, the Cockcroft-Gault (CG) equation considers patients’ weight and estimates a creatinine clearance in ml/min [20]. It can directly be used for drug dosing and has been the standard for dose recommendations in most summary of product characteristics (SPC) in the last decades, but it has to be discussed which weight (e.g. total, ideal, adjusted or lean body weight) to use [21,22,23,24].
In addition to CKD, acute kidney injury (AKI) has to be considered when drugs are prescribed. This is especially important in urologic patients, who often present with urinary flow obstructions at hospital admission. This may be transitory, but still overdosage and inappropriate drug selection are of immediate concern. Estimating renal function in AKI is challenging since creatinine is not in a steady-state [1].
With hospital admission, the physician on ward becomes responsible for a patient’s drug therapy. The ambulant medications are generally continued during hospital stay. Therefore, dosing errors that have been introduced in ambulant care may be continued during the hospital stay and cause ADR, if not identified and corrected at the time of hospital admission. In our hospital, a pharmacist-led medication reconciliation is supporting this process. Since RI often remains unrecognized in outpatients, screening for decreased eGFR and rDRP at this transition of care is important.
To our knowledge, no data exist about the prevalence of impaired renal function in patients admitted to an urologic department of a tertiary teaching hospital. It is currently unknown, if and which RRD are taken by these patients and if rDRP exist. Additionally, the impact of using the eGFRnon-indexed (actual BSA) rather than the eGFRindexed (standard-BSA) in clinical routine has not been addressed yet.
The objective of this study was to determine the number of patients admitted to urological wards presenting with RI and to evaluate how many of these patients changed eGFR-categories when referring to indexed vs. non-indexed eGFR, estimated with the CKD-EPI-equation. In addition, patients with eGFRnon-indexed 15–59 ml/min were further analysed regarding RRD and rDRP concerning pre-existing drug therapy.
Methods
Patients, setting and design
We conducted a retrospective observational study of patients at the time of hospital admission to two urological wards of the University Hospital Munich, Germany, between July 2016 and December 2016. Patients were included if they were ≥ 18 years of age and received a pharmacist-led medication reconciliation at admission, generating a structured medication plan of all prescribed and over the counter drugs used. Readmissions were included, since the study was designed to represent a real-life setting and patient’s renal function may change over time.
The following data were collected: age, gender, height, weight, eGFRindexed, drugs at admission including drugs on-demand and scheduled medications and comorbidities known to affect renal function. Body mass index (BMI), BSA (Mosteller equation) and eGFRnon-indexed were calculated [18, 25, 26].
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the ethics committee at Ludwig-Maximilians-University Munich, registration number 778-16.
Data collection
Data were collected from the hospital’s electronical patient information system (SAP-i.s.h.med, Cerner Corporation, North Kansas City, USA) that includes medical reports, diagnoses and administrative documents. Drugs and dosages were extracted from the medication plans generated by a pharmacist at admission. Comorbidities were recorded either from SAP-i.s.h.med or derived from the indication of drugs taken, e.g. statins for hypercholesterolemia.
Renal impairment
The eGFRindexed was automatically calculated by the clinical laboratory using the CKD-EPI-equation with standardized serum creatinine [27,28,29]. The pharmacist estimated BSA and readjusted the eGFRindexed to eGFRnon-indexed for drug dosing recommendations by using the equation eGFRnon-indexed = eGFRindexed/1.73 m2 × BSA [18].
Identification of ‘renal risk drugs’ and renal drug-related problems
Furthermore, patients with eGFRnon-indexed 15–59 ml/min were identified and their medication at admission was screened for renal risk drugs (RRD) and renal drug-related problems (rDRP). RRD/rDRP were analysed for subgroups of eGFR-categories (15–29, 30–44 and 45–59 ml/min). The medications of patients with eGFRnon-indexed > 60 ml/min usually do not need dose or drug adaption and patients with eGFRnon-indexed < 15 ml/min are routinely under the care of a nephrologist; thus, they were not further analysed in this study.
The evaluation whether a drug was a RRD and whether the dosage was incorrect or contraindicated with the individual’s eGFRnon-indexed was based on the information given in the German SPC or the drug information database AiDKlinik® that refers to the renal dose recommendation portal Dosing® (www.dosing.de). In case of discrepancies, an additional source was consulted [30].
Classification of renal drug-related problems
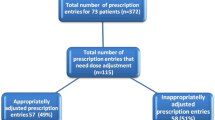
The renal drug-related problems (rDRP) were classified in consensus decision by three clinical pharmacists. rDRP were categorized with regard to ‘PCNE Classification’ and previous studies concerning rDRP (Fig. 1) [3, 4, 31]. All rDRP were classified as potential or manifest depending on the individual’s eGFRnon-indexed. Manifest rDRP are present with the current eGFRnon-indexed. Potential rDRP concern eGFRnon-indexed-values at threshold range (until +15 ml/min) and action must be taken when renal function decreases further. The actual incidence of adverse clinical events resulting from rDRP was not investigated.
Classification of potential/manifest renal drug-related problems depending on an individual’s eGFR (ml/min). The renal drug-related problem (rDRP) of either treatment safety or treatment effectiveness is categorized in one main cause and more than one intervention might be necessary to solve rDRP. CK, creatine kinase; ADR, adverse drug reaction
The rDRP concern either treatment safety or treatment effectiveness and are categorized in one main cause inducing the rDRP. One rDRP may lead to one or more interventions.
The suggested interventions were related to drug level and/or need for ‘monitoring’. Monitoring refers to control of serum blood levels (e.g. electrolytes, creatine kinase) or ADR. Monitoring of serum creatinine and eGFR was not included since it is mandatory in this patient population.
Statistical analysis
Data at admission were analysed using descriptive statistics. Qualitative variables are presented with their frequency distribution. Quantitative variables are expressed as the median and interquartile range (data without normal distribution). For comparison of the patient’s characteristics concerning age and gender, Chi-square test was used for categorical variables (independent samples) and Mann-Whitney U test for continuous variables (without normal distribution, independent samples). Statistical significance was accepted as p < 0.05.
Statistical analyses and figures were performed with Microsoft Excel® 2016 (Seattle, WA, USA) and IBM SPSS Statistics® version 25.0 (Armonk, NY, USA).
Results
Identification and categories of renal impairment: the impact of eGFRindexed versus eGFRnon-indexed
During the 6-month study period, 1341 patients were admitted. For 1320 (98%) patients, pharmacist-led medication reconciliation was performed. The majority of all patients were male (82.6%) and the median age 67 (18–94) years. Baseline characteristics of all patients are shown in Table 1.
As there is an uncertainty regarding which formula is routinely used for drug dosing purposes in clinical routine, we investigated the impact on the number of patients with renal impairment (RI) using eGFRindexed versus eGFRnon-indexed. Two hundred seventy (20.5%) patients had an eGFRindexed of 15–59 ml/min/1.73m2 and 16 (1.2%) patients presented with eGFRindexed < 15 ml/min/1.73m2. However, the median BSA for all patients was noticeably higher than 1.73 m2 (median 1.97 m2, 1.17–2.86). When taking the patients’ actual BSA into account and recalculating to eGFRnon-indexed, 67 (5.1%) patients were no longer in the critical range of 15–59 ml/min (Figs. 2 and 3).
The remaining 203 (15.4%) patients in the critical eGFRnon-indexed-range of 15–59 ml/min were older (median age 76 (30–94) years) in comparison with patients with eGFR ≥ 60 ml/min and significantly more often presented with comorbidities such as arterial hypertension, cardiovascular disease or hyercholesterolemia. There was no significant difference in the occurrence of prostatic hyperthrophy (p = 0.98), diabetes mellitus type 2 (p = 0.32) and urinary flow obstructions (p = 0.08).
Comparing male and female patients with eGFRnon-indexed 15–59 ml/min, male patients presented with higher BMI and BSA, but no significant difference in age (p = 0.31), number of drugs (p = 0.62), and eGFRnon-indexed (p = 0.69) was found. The comorbidities differed regarding hyperuricemia and cardiovascular diseases.
Comparing patients aged < 65 and ≥ 65 years, eGFRnon-indexed did not significantly differ (p = 0.88), while older patients took more drugs (p < 0.05).
RRD and rDRP in patients with eGFRnon-indexed 15–59 ml/min
As the eGFRnon-indexed should correctly be used for dosing drugs, we next deciphered the occurrence of RRD and rDRP in the patients with eGFRnon-indexed of 15–59 ml/min. One hundred ninety (93.6%) of the 203 patients took one or more drugs at admission (Table 2). In total, 1209 drugs were documented for these patients with a median number of 6 (1–18) drugs per patient. Out of these, 660 (54.7%) were identified as RRD with a median of 3 (0–11) RRD per patient. The 1209 drugs taken represented 218 different substances according to the Anatomical Therapeutic Chemical (ATC) classification system with 113 (51.8%) matching the criteria of RRD.
Of the 660 RRD, 264 RRD led to rDRP concerning 76 different substances. This represents 21.8% of all medications and 40.0% of the RRD. One hundred fifteen patients of 190 (60.5%) had rDRP already at hospital admission. The 260 documented rDRP represented a median number of 2 (0–10) rDRP per patient (Table 2). In two cases, the rDRP was a ‘drug combination potentially decreasing renal function’ triggered by three drugs. Thus, the number of RRD (n = 264) is higher than the number of rDRP (n = 260).
Detailed analysis of rDRP
For all patients with rDRP (eGFRnon-indexed 15–59 ml/min; n = 115), more manifest (58.5%) than potential (41.5%) rDRP were found (Fig. 4). Enoxaparin and colecalciferol, followed by ramipril, spironolactone, hydrochlorothiazide, simvastatin and metformin are the drugs most often associated with rDRP (Fig. S2). The most frequent intervention for manifest rDRP would have been ‘monitoring’ and ‘dosage change’, and for potential rDRP ‘dosage change’ and ‘drug change/drug stop’.
Potential and manifest renal drug-related problems (rDRP) (n = 260) in patients with eGFRnon-indexed of 15–59 ml/min and ≥ 1 drug (n = 190). a Type of rDRP. b Causes of rDRP. c Interventions that should be proposed to prescriber to solve rDRP. Potential: eGFR must be monitored, if it decreases, action must be taken. Manifest: rDRP is currently present.
Discussion
In this study, for the first time, the prevalence and the nature of RRD and rDRP were assessed in patients presenting with RI at admission to urological wards in a tertiary teaching hospital. Of note, we found that over half of the drugs taken at admission are RRD with 40.0% of these leading to rDRP. The use of indexed versus non-indexed eGFR has a noticeable impact on the determination of renal function, in turn influencing drug dosing and thus patient safety.
We found 21.7% of patients to have RI with an eGFRindexed < 60 ml/min/1.73m2 at hospital admission. The number of affected patients was expected to be higher in urology, since urinary flow obstructions and prostatic hypertrophy are typical for patients admitted to urologic wards, but this is within the similar range reported by other studies for all hospitalized patients or patients admitted to internal medicine [3, 6]. There was however no difference in the occurrence of prostatic hypertrophy or urinary flow obstructions in the different eGFR-subgroups. We could not distinguish the percentage of patients with AKI or CKD or a combination of both at hospital admission, since eGFR-values from the past were rarely available.
Screening for RI at hospital admission is especially important considering that up to 72% of non-hospitalized CKD patients are not aware of their kidney insufficiency [2] and RI is an established risk factor for DRP [32]. Regarding the adjustment of drug therapy to renal function, it is vital to understand which estimation of GFR or renal clearance to use. For the classification of severity of the disease, international guidelines mainly recommend the use of the CKD-EPI-equation standardized to BSA of 1.73 m2 [1]. For drug dosing purposes, a measurement for renal function in ml/min (eGFRnon-indexed or eKreaCl) should be used [19]. Noteworthy, most patients in this study had a higher BSA (median 1.97 m2, range 1.17–2.86) than the standard BSA of 1.73 m2, which influences the calculation of eGFRnon-indexed. Indeed, we detected a considerable shift of patients between eGFR-subgroups when readjusting for actual BSA, resulting in a distinct decrease in the number of patients to consider for drug therapy adjustment. In fact, obesity is a rising problem in the last years and has to be considered for the estimation of renal function and drug dosing. Recent reviews summarize that for drug dosing, eGFRindexed underestimates renal function, and therefore, eGFRnon-indexed should be used [22, 23]. Indeed, our data suggest that the patient’s individual weight and height have to be increasingly considered, and subsequently, eGFRindexed must be adjusted to patients’ actual BSA for correct drug dosing. This recalculation to eGFRnon-indexed for drug dosing was not considered in comparable studies [3, 4]. Nevertheless, in our opinion, this is a crucial point to be stressed, since many practitioners are not aware of the differences between the calculations and their impact on determining renal function and thus drug dosing.
This study focused on patients with an eGFRnon-indexed 15–59 ml/min for two reasons. Firstly, adjustment of drug therapy is usually necessary for GFRnon-indexed < 60 ml/min [30]. Secondly, whereas patients with < 15 ml/min are normally under supervision of a nephrologist, patients with 15–59 ml/min are generally not and are therefore at increased risk for rDRP. Although we adjusted the eGFRindexed to the actual BSA (eGFRnon-indexed), the number of patients displaying one or more rDRP (61%) and the median number of rDRP/patient was similar to studies from other medical departments using the eGFRindexed [3, 4]. However, in our study, every second drug was classified as RRD with about 40.0% of the RRD associated with rDRP, which is somewhat higher compared with other studies [3]. One reason for this might be that patients are admitted to an university hospital with more serious health problems, demanding consultation of specialists. This could lead to a higher number of drugs taken by patients at a university hospital compared with non-university hospitals. However, we did not test this hypothesis. Manifest rDRP accounted with 58.5% for the majority of detected rDRP in our study. Use of suboptimal drugs, followed by overdosage and the presence of contraindications, were the causes in most cases.
When distinguishing further in eGFR-subgroups, which represent common dosage frames, more manifest rDRP are seen in lower eGFR-ranges. Of note, more than half of manifest rDRP concerning treatment safety occurred in patients with an eGFRnon-indexed 15–29 ml/min. The most frequently prescribed RRD associated with manifest rDRP in our patient population was low molecular weight heparins (LMWH; enoxaparin in this case). The unadjusted dosage of LMWH leads to a higher bleeding risk for patients with RI [30, 33]. Our data indicate that the awareness of correct prescribing of LMWH in patients with RI still seems to be problematic in the ambulant setting and therefore may also be a risk factor in the hospital setting.
Renal function can alter quickly in urologic patients after hospital admission, e.g. impairing in the perioperative period or improving after correction of urinary flow obstructions [34,35,36]. Therefore, we think it is important not only to focus on manifest rDRP but also to point out potential rDRP that may suddenly become relevant. The leading cause for potential rDRP was overdosage, followed by contraindication or the use of a suboptimal drug. This is in line with the findings of other studies where non-optimal dose and non-optimal drugs were the main causes for rDRP [3, 4]. The most frequently prescribed drug associated with potential rDRP was vitamin D. Indeed, there are still uncertainties regarding the use (indication and type of vitamin D derivative) of vitamin D and its derivatives depending on renal function [7]. Physicians follow recommendations to prescribe vitamin D to patients with RI. As the main activation from colecalciferol to calcitriol takes place in the kidneys, a change of prescription to the activated form has to be considered from a certain stage of kidney disease on. In our experience, this is often neglected and there is a need of further guidance how to prescribe vitamin D derivatives depending on the severity of RI.
Additionally, it has to be kept in mind that some drugs are specifically used against their labeling e.g. hydrochlorothiazide in combination with loop diuretics with an eGFR < 30 ml/min, and should not be classified as rDRP. Thus, it is important to use renal dosing references additionally to the SPC to determine RRD.
In non-hospitalized patients, inappropriate prescribing in RI was found in up to 80% and associated with more ADR, a longer hospital stay and a higher mortality risk [10, 12]. Thus, at hospital admission, screening for affected patients is of great importance as a proactive risk management. Physicians and pharmacists should work together to achieve safer drug prescribing [13]. The most significant reduction of inappropriate prescribing in patients with RI has indeed been observed when physicians received immediate feedback from pharmacists [12]. Prescription review followed by recommendations by a pharmacist has been shown to positively influence clinical outcome and even reduce costs of hospital stay [37]. In our study, for manifest and potential rDRP, the three most often recommended interventions to the physician on ward would have been monitoring, change of dosage and change or discontinuation of a drug.
Furthermore, it is important to recalculate the automatically reported eGFRindexed to the eGFRnon-indexed before assessing the medication. In our experience, this recalculation is not usually performed by physicians on wards and the support of a pharmacist would be important. Moreover, the use of medication plans derived from medication reconciliation by a pharmacist at hospital admission, as in this study, can identify patients at risk. It has been shown that these plans are more complete and accurate compared with medication plans prepared by physicians [38, 39].
Some limitations of the study should be considered. This retrospective study focused on rDRP but did not assess possibly related adverse drug reactions, which should be included in future evaluations. Readmissions were included in our study to represent a real-life setting and because patient’s renal function may change over time. However, this might have over- or underestimated the prevalence of RI in our study population. In addition, we assumed comorbidities from the indication of drugs taken by the patients because experiences from previous evaluations revealed that the documentation of diagnoses is often poor. This allows a more complete characterisation of the comorbidities in our study population. However, at the same time, due to drugs given without indication or due to diseases not treated adequately with drugs, errors may be included in our evaluation.
Conclusion
Our study provides novel evidence that urological patients with RI take a high number of RRD at hospital admission, leading to a substantial number of rDRP. This may be a risk factor for patient safety during the hospital stay. In addition, our analyses demonstrate considerable shifts of patients between eGFR-categories when recalculating eGFR from standard-BSA (indexed eGFR; ml/min/1.73m2) to individual BSA (non-indexed eGFR; ml/min) for drug dosing purposes. This is an important point to avoid over- and underdosing or mistakes in contraindications that are frequently overlooked so far.
Future goals should be to develop a risk assessment to simplify the identification of the concerned patients during the pharmacist-led medication reconciliation at admission and to investigate the best way to inform physicians on ward about inappropriate drug use to ensure appropriate prescribing during the hospital stay.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADR:
-
adverse drug reactions
- AKI:
-
acute kidney injury
- BMI:
-
body mass index
- BSA:
-
body surface area
- CK:
-
creatine kinase
- CKD:
-
chronic kidney disease
- CKD-EPI:
-
chronic kidney disease epidemiology collaboration
- CG:
-
Cockcroft-Gault
- eGFR:
-
estimated glomerular filtration rate
- rDRP:
-
renal drug-related problems
- KDIGO:
-
Kidney Disease Improving Global Outcomes Initiative
- LMWH:
-
low molecular weight heparins
- RI:
-
renal impairment
- RRD:
-
renal risk drugs
- SPC:
-
summary of product characteristics
References
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Girndt M, Trocchi P, Scheidt-Nave C, Markau S, Stang A (2016) The prevalence of renal failure. Results from the German Health Interview and Examination Survey for Adults, 2008-2011 (DEGS1). Deutsches Arzteblatt International 113 (6):85–91. doi:https://doi.org/10.3238/arztebl.2016.0085
Blix HS, Viktil KK, Moger TA, Reikvam A (2006) Use of renal risk drugs in hospitalized patients with impaired renal function--an underestimated problem? Nephrol Dial Transplant 21 (11):3164–3171. doi:https://doi.org/10.1093/ndt/gfl399
Holm H, Bjerke K, Holst L, Mathiesen L (2015) Use of renal risk drugs in patients with renal impairment. Int J Clin Pharm 37(6):1136–1142. https://doi.org/10.1007/s11096-015-0175-3
Brater DC (2009) Drug dosing in patients with impaired renal function. Clin Pharmacol Ther 86(5):483–489. https://doi.org/10.1038/clpt.2009.135
Hartmann B, Czock D, Keller F (2010) Drug therapy in patients with chronic renal failure. Deutsches Arzteblatt International 107(37):647–655
Cardoso MP, Pereira LAL (2018) Native vitamin D in pre-dialysis chronic kidney disease. Nefrologia : publicacion oficial de la Sociedad Espanola Nefrologia 39:18–28. https://doi.org/10.1016/j.nefro.2018.07.004
Jentzer JC, DeWald TA, Hernandez AF (2010) Combination of loop diuretics with thiazide-type diuretics in heart failure. J Am Coll Cardiol 56(19):1527–1534. https://doi.org/10.1016/j.jacc.2010.06.034
Munar MY, Singh H (2007) Drug dosing adjustments in patients with chronic kidney disease. Am Fam Physician 75(10):1487–1496
Dorks M, Allers K, Schmiemann G, Herget-Rosenthal S, Hoffmann F (2017) Inappropriate medication in non-hospitalized patients with renal insufficiency: a systematic review. J Am Geriatr Soc 65(4):853–862. https://doi.org/10.1111/jgs.14809
Long CL, Raebel MA, Price DW, Magid DJ (2004) Compliance with dosing guidelines in patients with chronic kidney disease. Ann Pharmacother 38(5):853–858. https://doi.org/10.1345/aph.1D399
Tesfaye WH, Castelino RL, Wimmer BC, Zaidi STR (2017) Inappropriate prescribing in chronic kidney disease: a systematic review of prevalence, associated clinical outcomes and impact of interventions. Int J Clin Pract 71(7). https://doi.org/10.1111/ijcp.12960
Hassan Y, Al-Ramahi R, Abd Aziz N, Ghazali R (2009) Drug use and dosing in chronic kidney disease. Ann Acad Med Singap 38(12):1095–1103
Hassan Y, Al-Ramahi RJ, Aziz NA, Ghazali R (2009) Impact of a renal drug dosing service on dose adjustment in hospitalized patients with chronic kidney disease. Ann Pharmacother 43(10):1598–1605. https://doi.org/10.1345/aph.1M187
Hug BL, Witkowski DJ, Sox CM, Keohane CA, Seger DL, Yoon C, Matheny ME, Bates DW (2009) Occurrence of adverse, often preventable, events in community hospitals involving nephrotoxic drugs or those excreted by the kidney. Kidney Int 76(11):1192–1198. https://doi.org/10.1038/ki.2009.353
Breton G, Froissart M, Janus N, Launay-Vacher V, Berr C, Tzourio C, Helmer C, Stengel B (2011) Inappropriate drug use and mortality in community-dwelling elderly with impaired kidney function--the Three-City population-based study. Nephrol Dial Transplant 26(9):2852–2859. https://doi.org/10.1093/ndt/gfq827
Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, Kurella Tamura M, Feldman HI (2014) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis 63(5):713–735. https://doi.org/10.1053/j.ajkd.2014.01.416
National Kidney Foundation (2014) Frequently asked questions about GFR estimates. USA. https://www.kidney.org/sites/default/files/12-10-4004_FAQ-ABE.pdf
European Medicines Agency (2015) Guideline on the evaluation of the pharmacokinetics of medicinal products in patients with decreased renal function. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-evaluation-pharmacokinetics-medicinal-products-patients-decreased-renal-function_en.pdf
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16(1):31–41
Morrish GA, Pai MP, Green B (2011) The effects of obesity on drug pharmacokinetics in humans. Expert Opin Drug Metab Toxicol 7(6):697–706. https://doi.org/10.1517/17425255.2011.570331
Hart LA, Anderson GD (2018) Methods of estimating kidney function for drug dosing in special populations. Clin Pharmacokinet 57:943–976. https://doi.org/10.1007/s40262-018-0628-7
Chang AR, Zafar W, Grams ME (2018) Kidney function in obesity-challenges in indexing and estimation. Adv Chronic Kidney Dis 25(1):31–40. https://doi.org/10.1053/j.ackd.2017.10.007
Hudson JQ, Nolin TD (2018) Pragmatic use of kidney function estimates for drug dosing: the tide is turning. Adv Chronic Kidney Dis 25(1):14–20. https://doi.org/10.1053/j.ackd.2017.10.003
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317(17):1098. https://doi.org/10.1056/nejm198710223171717
Fancher KM, Sacco AJ, Gwin RC, Gormley LK, Mitchell CB (2016) Comparison of two different formulas for body surface area in adults at extremes of height and weight. JS Oncol Pharm Pract 22(5):690–695. https://doi.org/10.1177/1078155215599669
Stevens LA, Schmid CH, Zhang YL, Coresh J, Manzi J, Landis R, Bakoush O, Contreras G, Genuth S, Klintmalm GB, Poggio E, Rossing P, Rule AD, Weir MR, Kusek J, Greene T, Levey AS (2010) Development and validation of GFR-estimating equations using diabetes, transplant and weight. Nephrol Dial Transplant 25(2):449–457. https://doi.org/10.1093/ndt/gfp510
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Stevens LA, Schmid CH, Greene T, Zhang YL, Beck GJ, Froissart M, Hamm LL, Lewis JB, Mauer M, Navis GJ, Steffes MW, Eggers PW, Coresh J, Levey AS (2010) Comparative performance of the CKD epidemiology collaboration (CKD-EPI) and the modification of diet in renal disease (MDRD) study equations for estimating GFR levels above 60 mL/min/1.73 m2. Am J Kidney Dis 56 (3):486–495. doi:https://doi.org/10.1053/j.ajkd.2010.03.026
Ashley C, Dunleavy A (2017) The renal drug handbook: the ultimate prescribing guide for renal practitioners, vol 4th edition. Radcliffe Publishing, Abingdon, UK
Pharmaceutical Care Network Europe Foundation (PCNE) (2017) Classification for Drug related problems V8.02
Falconer N, Barras M, Cottrell N (2018) Systematic review of predictive risk models for adverse drug events in hospitalized patients. Br J Clin Pharmacol 84(5):846–864. https://doi.org/10.1111/bcp.13514
Hoffmann P, Keller F (2012) Increased major bleeding risk in patients with kidney dysfunction receiving enoxaparin: a meta-analysis. Eur J Clin Pharmacol 68(5):757–765. https://doi.org/10.1007/s00228-011-1149-6
Zarbock A, Koyner JL, Hoste EAJ, Kellum JA (2018) Update on perioperative acute kidney injury. Anesth Analg 127(5):1236–1245. https://doi.org/10.1213/ane.0000000000003741
Better OS, Arieff AI, Massry SG, Kleeman CR, Maxwell MH (1973) Studies on renal function after relief of complete unilateral ureteral obstruction of three months’ duration in man. Am J Med 54(2):234–240. https://doi.org/10.1016/0002-9343(73)90228-3
Cheung CM, Ponnusamy A, Anderton JG (2008) Management of acute renal failure in the elderly patient: a clinician’s guide. Drugs Aging 25(6):455–476. https://doi.org/10.2165/00002512-200825060-00002
Jourdan JP, Muzard A, Goyer I, Ollivier Y, Oulkhouir Y, Henri P, Parienti JJ, Breuil C (2018) Impact of pharmacist interventions on clinical outcome and cost avoidance in a university teaching hospital. Int J Clin Pharm 40:1474–1481. https://doi.org/10.1007/s11096-018-0733-6
Abdulghani KH, Aseeri MA, Mahmoud A, Abulezz R (2018) The impact of pharmacist-led medication reconciliation during admission at tertiary care hospital. Int J Clin Pharm 40(1):196–201. https://doi.org/10.1007/s11096-017-0568-6
Leguelinel-Blache G, Arnaud F, Bouvet S, Dubois F, Castelli C, Roux-Marson C, Ray V, Sotto A, Kinowski JM (2014) Impact of admission medication reconciliation performed by clinical pharmacists on medication safety. Eur J Int Med 25(9):808–814. https://doi.org/10.1016/j.ejim.2014.09.012
Acknowledgements
Open Access funding provided by Projekt DEAL. This work was supported by Stiftung Patient und Klinische Pharmazie, Munich, Germany.
Funding
This work was supported by the interprofessional doctoral programme Clinical Pharmacy, Ludwig-Maximilians-University Munich, Germany and by the Stiftung Patient und Klinische Pharmazie, Munich, Germany.
Author information
Authors and Affiliations
Contributions
Sarah Seiberth participated in the design of the study, was responsible for acquisition of data, classification of rDRP, performed the analysis and drafted the manuscript. Dominik Bauer participated as a clinical pharmacist in the classification of the rDRP and critically reviewed the manuscript. Ulf Schönermarck made substantial contributions to the conception of the study, interpretation of results and critically reviewed the manuscript. Hanna Mannell helped with statistical questions, analysis of the data and revision of the manuscript. Christian Stief critically revised the manuscript for important intellectual content. Joerg Hasford made substantial contributions to the conception and design of the study, including analyses, and manuscript preparation. Dorothea Strobach made substantial contributions to the conception and the design of the study, classified rDRP and was involved in result interpretation and manuscript preparation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. Ethical approval was obtained from the ethics committee at Ludwig-Maximilians-University Munich, registration number 778-16.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 88 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seiberth, S., Bauer, D., Schönermarck, U. et al. Correct use of non-indexed eGFR for drug dosing and renal drug-related problems at hospital admission. Eur J Clin Pharmacol 76, 1683–1693 (2020). https://doi.org/10.1007/s00228-020-02953-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-02953-6