Abstract
Purpose
Para-aminosalicylic acid (PAS) is currently one of the add-on group C medicines recommended by the World Health Organization for multidrug-resistant tuberculosis treatment. At the recommended doses (8–12 g per day in two to three divided doses) of the widely available slow-release PAS formulation, studies suggest PAS exposures are lower than those reached with older PAS salt formulations and do not generate bactericidal activity. Understanding the PASER dose-exposure–response relationship is crucial for dose optimization. The objective of our study was to establish a representative population pharmacokinetics model for PASER and evaluate the probability of bactericidal and bacteriostatic target attainment with different dosing regimens.
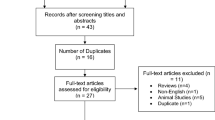
Methods
To this end, we validated and optimized a previously published population pharmacokinetic model on an extended dataset. The probability of target attainment was evaluated for once-daily doses of 12 g, 14 g, 16 g and 20 g PASER.
Results
The final optimized model included the addition of variability in bioavailability and allometric scaling with body weight on disposition parameters. Peak PAS concentrations over minimum inhibitory concentration of 100, which is required for bactericidal activity are achieved in 53%, 65%, 72% and 84% of patients administered 12, 14, 16 and 20 g once-daily PASER, respectively, when MIC is 1 mg/L. For the typical individual, the exposure remained above 1 mg/L for ≥ 98% of the dosing interval in all the evaluated PASER regimens.
Conclusion
The pharmacokinetic/pharmacodynamic parameters linked to bactericidal activity should be determined for 14 g, 16 g and 20 g once-daily doses of PASER.






Similar content being viewed by others
References
WHO Consolidated Guidelines on Drug-Resistant Tuberculosis Treatment. Geneva: World Health Organization; 2019
Treatment of pulmonary tuberculosis with streptomycin and para-aminosalicylic acid; a Medical Research Council investigation. Br Med J. 1950;2(4688):1073–85
The prevention of streptomycin resistance by combined chemotherapy; a Medical Research Council investigation. Br Med J. 1952;1:1157–62
Isoniazid in combination with streptomycin or with P.A.S. in the treatment of pulmonary tuberculosis; fifth report to the Medical Research Council by their Tuberculosis Chemotherapy Trials Committee. Br Med J. 1953;2(4844):1005–14
Various combinations of isoniazid with streptomycin or with P.A.S. in the treatment of pulmonary tuberculosis; seventh report to the Medical Research Council by their Tuberculosis Chemotherapy Trials Committee. Br Med J. 1955;1(4911):435–45
Yue WY, Cohen SS (1966) Toleration and absorption of sodium para-aminosalicylate and para-aminosalicylic acid (neopasalate). Comparison with other forms of para-aminosalicylic acid. Dis Chest 49(2):165–174
de Kock L, Sy SKB, Rosenkranz B, Diacon AH, Prescott K, Hernandez KR, Yu M, Derendorf H, Donald PR (2014) Pharmacokinetics of para-aminosalicylic acid in HIV-uninfected and HIV-coinfected tuberculosis patients receiving antiretroviral therapy, managed for multidrug-resistant and extensively drug-resistant tuberculosis. Antimicrob Agents Chemother 58(10):6242–6250
Citron KM, Kuper SW (1959) Para-aminosalicylic-acid (PAS) concentrations in the serum during treatment with various PAS preparations. Tubercle. 40:443–452
Donald PR, Diacon AH (2015) Para-aminosalicylic acid: the return of an old friend. Lancet Infect Dis 15(9):1091–1099
Abulfathi AA, Donald PR, Adams K, Svensson EM, Diacon AH, Reuter H (May 2020) The pharmacokinetics of para-aminosalicylic acid and its relationship to efficacy and intolerance. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.14395
Jindani A, Aber VR, Edwards EA, Mitchison DA (1980) The early bactericidal activity of drugs in patients with pulmonary tuberculosis. Am Rev Respir Dis 121(6):939–949
Charles F (1955) The treatment of pulmonary tuberculosis with intravenous PAS-infusions. Tubercle. 36(2):40–44
Reisner D (1966) Comparison of single and divided daily dosages of isoniazid and PAS in the treatment of pulmonary tuberculosis. XV. A report of the Veterans Administration-Armed Forces Cooperative. Study on the chemotherapy of tuberculosis. Am Rev Respir Dis 94(6):849–857
Paser (Jacobus Pharmaceutical Company, Inc.). https://medlibrary.org/lib/rx/meds/paser/. 2010
WHO treatment guidelines for drug- resistant tuberculosis October 2016 Revision
Peloquin CA, Henshaw TL, Huitt GA, Berning SE, Nitta AT, James GT (1994) Pharmacokinetic evaluation of para-aminosalicylic acid granules. Pharmacother J Hum Pharmacol Drug Ther 14(1):40–46
Sy SKB, de Kock L, Diacon AH, Werely CJ, Xia H, Rosenkranz B, van der Merwe L, Donald PR (2015) N-acetyltransferase genotypes and the pharmacokinetics and tolerability of para-aminosalicylic acid in patients with drug-resistant pulmonary tuberculosis. Antimicrob Agents Chemother 59(7):4129–4138
Liwa AC, Schaaf HS, Rosenkranz B, Seifart HI, Diacon AH, Donald PR (2013) Para-aminosalicylic acid plasma concentrations in children in comparison with adults after receiving a granular slow-release preparation. J Trop Pediatr 59(2):90–94
Wan SH, Pentikainen PJ, Azarnoff DL (1974) Bioavailability of aminosalicylic acid and its various salts in humans III: absorption from tablets. J Pharm Sci 63(5):708–711
Peloquin CA, Zhu M, Adam RD, Singleton MD, Nix DE (2001) Pharmacokinetics of para -aminosalicylic acid granules under four dosing conditions. Ann Pharmacother 35(11):1332–1338
Heifets LB (1991) Antituberculosis drugs: antimicrobial activity in vitro, p 13–58. In Heifets LB (Ed), Drug Susceptibility in the Chemotherapy of Mycobacterial Infections
Kibleur Y, Brochart H, Schaaf HS, Diacon AH, Donald PR (2014) Dose regimen of para-aminosalicylic acid gastro-resistant formulation (PAS-GR) in multidrug-resistant tuberculosis. Clin Drug Investig 34(4):269–276
Bartmann K (Karl). Antituberculosis drugs. Springer Berlin Heidelberg; 1988
Mayer RL, Eisman PC, Gisi TA, Konopka EA (1958) The chemotherapeutic activity upon chromogenic mycobacteria of certain derivatives of thiocarbanilide (Su 1906), thiazoline (Su 3068), and thiazolidinone (Su 3912). Am Rev Tuberc 77(4):694–702
Furesz S (1970) Chemical and biological properties of rifampicin. Antibiot Chemother Fortschritte Adv Prog 16:316–351
Walter A (1950) Die tuberkulostatische Wirksamkeit verschiedener PAS-Präparate in vitro. DMW - Dtsch Medizinische Wochenschrift. 75(17):587–587
Heilmeyer L (1950) Weitere Erfahrungen mit Streptomycin, PAS und TBI (Conteben) in der Behandlung der internen Tuberkulosen. DMW - Dtsch Medizinische Wochenschrift 75(15):473–477
Ngaimisi E, Minzi O, Mugusi S, Sasi P, Riedel KD, Suda A, Ueda N, Bakari M, Janabi M, Mugusi F, Bertilsson L, Burhenne J, Aklillu E, Diczfalusy U (2014) Pharmacokinetic and pharmacogenomic modelling of the CYP3A activity marker 4 -hydroxycholesterol during efavirenz treatment and efavirenz/rifampicin co-treatment. J Antimicrob Chemother 69(12):3311–3319
Svensson EM, Aweeka F, Park J-G, Marzan F, Dooley KE, Karlsson MO (2013) Model-based estimates of the effects of efavirenz on bedaquiline pharmacokinetics and suggested dose adjustments for patients coinfected with HIV and tuberculosis. Antimicrob Agents Chemother 57(6):2780–2787
Lee LSU, Pham P, Flexner C (2012) Unexpected drug-drug interactions in human immunodeficiency virus (HIV) therapy: induction of UGT1A1 and bile efflux transporters by Efavirenz. Ann Acad Med Singap 41(12):559–562
Jones JS (1954) Intravenous P.A.S. in relation to pulmonary tuberculotherapy, with an account of 1,145 transfusions. Br J Tuberc Dis Chest 48(4):286–297
Hollander AG (1955) Para-aminosalicylic acid-resin complex: studies in absorption, serum electrolytes, and tolerance. Am Rev Tuberc. 72(4):548–551
Riska N, Tennberg C (1962) Optimal PAS dosage. Am Rev Respir Dis 86:430–433
Riska N (1959) PAS therapy with a daily unfractionated dose. Acta Tuberc Scand 37:104–111
Acknowledgments
We are grateful to Mats Karlsson and Lénaïg Tanneau for the initial analyses plan and to Bernd Rosenkranz and Sherwin Sy for providing the datasets.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. AAA and EMS are supported by PanACEA, which is part of the European and Developing Countries Clinical Trials Partnership (EDCTP) 2 programme supported by the European Union (grant number TRIA2015–1102-PanACEA).
Author information
Authors and Affiliations
Contributions
AAA contributed in developing the research questions, data formatting, designing and execution of the modelling and simulation study, interpreting the results and drafting the manuscript. PA contributed in data formatting, designing of the modelling study and critical review of the manuscript. PRD, AHD and HR contributed in the conceptual design of the study, interpreting the results and critical review of the manuscript. EMS contributed in developing the research questions, designing and supervision of the modelling and simulation study, interpreting the results and critical review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics declaration
Stellenbosch University’s Health Research Ethics Committee (S19/01/007) approved this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 428 kb)
Rights and permissions
About this article
Cite this article
Abulfathi, A.A., Assawasuwannakit, P., Donald, P.R. et al. Probability of mycobactericidal activity of para-aminosalicylic acid with novel dosing regimens. Eur J Clin Pharmacol 76, 1557–1565 (2020). https://doi.org/10.1007/s00228-020-02943-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-02943-8