Abstract
Purpose
The aim of this systematic review was to examine and compare differences in the way medication exposures are classified in studies using linked administrative data to investigate outcomes following medication use during pregnancy. This was undertaken with a focus on studies investigating specific neonatal outcomes following prenatal exposure to selective serotonin reuptake inhibitors (SSRIs).
Methods
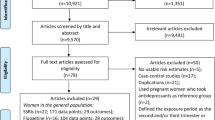
We searched Medline and Embase to identify studies that used linked administrative data to investigate specific neonatal outcomes (congenital malformations, birth weight, gestational age) following prenatal exposure to SSRIs.
Results
Key factors such as dose, duration and timing of exposure were inconsistently addressed in the studies identified. In addition, there was a great deal of variability in the way medication exposures were classified and how women who stop taking their medication before or during early pregnancy are handled in analyses. Furthermore, there are issues in assuming how and when women who receive a dispensing for a medication actually take it during pregnancy. This creates a great deal of uncertainty around medication exposure during pregnancy in studies using linked administrative data, potentially resulting in biased risk estimates.
Conclusions
There is a need for greater focus on determining the most effective and accurate way of using linked administrative data to investigate outcomes following medication use during pregnancy in an effort to minimise potential biases.


Similar content being viewed by others
References
Mitchell A (2003) Systematic identification of drugs that cause birth defects - a new opportunity [editorial]. N Engl J Med 349(26):2556–2559
Irl C, Hasford J (2000) Assessing the safety of drugs in pregnancy: the role of prospective cohort studies. Drug Saf 22(3):169–177
Källén BAJ (2005) Methodological issues in the epidemiological study of the teratogenicity of drugs. Congenit Anom (Kyoto) 45(2):44–51
Schaefer C, Ornoy A, Clementi M, Meister R, Weber-Schoendorfer C (2008) Using observational cohort data for studying drug effects on pregnancy outcome—methodological considerations. Reprod Toxicol 26(1):36–41
Andrews EB, Tennis P (2007) Promise and pitfalls of administrative data in evaluating pregnancy outcomes. Pharmacoepidemiol Drug Saf 16(11):1181–1183
Holman CDJ, Bass JA, Rouse IL, Hobbs MST (1999) Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 23(5):453–459
Brent RL (2001) Addressing environmentally caused human birth defects. Pediatr Rev 22(5):153–165
Alwan S, Reefhuis J, Rasmussen SA, Friedman JM (2011) Patterns of antidepressant medication use among pregnant women in a united states population. J Clin Pharmacol 51(2):264–270
Grzeskowiak LE, Gilbert AL, Morrison JL (2011) Investigating outcomes following the use of SSRIs for treating depression in pregnancy: a focus on methodological issues. Drug Saf 34(11):1027–1048
Malm H, Klaukka T, Neuvonen PJ (2005) Risks associated with selective serotonin reuptake inhibitors in pregnancy. Obstet Gynecol 106(6):1289–1296
Oberlander TF, Warburton W, Misri S, Riggs W, Aghajanian J, Hertzman C (2008) Major congenital malformations following prenatal exposure to serotonin reuptake inhibitors and benzodiazepines using population-based health data. Birth Defects Res B Dev Reprod Toxicol 83(1):68–76
Pedersen LH, Henriksen TB, Vestergaard M, Olsen J, Bech BH (2009) Selective serotonin reuptake inhibitors in pregnancy and congenital malformations: population based cohort study. BMJ 339(231):b3569
Kornum JB, Nielsen RB, Pedersen L, Mortensen PB, Norgaard M (2010) Use of selective serotonin-reuptake inhibitors during early pregnancy and risk of congenital malformations: updated analysis. Clin Epidemiol 2:29–36
Colvin L, Slack Smith L, Stanley FJ, Bower C (2011) Dispensing patterns and pregnancy outcomes for women dispensed selective serotonin reuptake inhibitors in pregnancy. Birth Defects Res A Clin Mol Teratol 91:142–152
Davis RL, Rubanowice D, McPhillips H, Raebel MA, Andrade SE, Smith D et al (2007) Risks of congenital malformations and perinatal events among infants exposed to antidepressant medications during pregnancy. Pharmacoepidemiol Drug Saf 16(10):1086–1094
Berard A, Ramos E, Rey E, Blais L, St-Andre M, Oraichi D (2007) First trimester exposure to paroxetine and risk of cardiac malformations in infants: the importance of dosage. Birth Defects Res B Dev Reprod Toxicol 80(1):18–27
Wogelius P, Nørgaard M, Gislum M, Pedersen L, Munk E, Mortensen PB et al (2006) Maternal use of selective serotonin reuptake inhibitors and risk of congenital malformations. Epidemiology 17(6):701–704
Wen SW, Yang Q, Garner P, Fraser W, Olatunbosun O, Nimrod C et al (2006) Selective serotonin reuptake inhibitors and adverse pregnancy outcomes. Am J Ostet Gynecol 194(4):961–966
Cole JA, Ephross SA, Cosmatos IS, Walker AM (2007) Paroxetine in the first trimester and the prevalence of congenital malformations. Pharmacoepidemiol Drug Saf 16(10):1075–1085
Simon GE, Cunningham ML, Davis RL (2002) Outcomes of prenatal antidepressant exposure. Am J Psychiatry 159(12):2055–2061
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C (2006) Neonatal outcomes after prenatal exposure to selective serotonin reuptake inhibitor antidepressants and maternal depression using population-based linked health data. Arch Gen Psychiatry 63(8):898–906
Oberlander TF, Warburton W, Misri S, Aghajanian J, Hertzman C (2008) Effects of timing and duration of gestational exposure to serotonin reuptake inhibitor antidepressants: population-based study. Br J Psychiatry 192(5):338–343
Bakker MK, Kolling P, van den Berg PB, de Walle HEK, de Jong van den Berg LTW (2008) Increase in use of selective serotonin reuptake inhibitors in pregnancy during the last decade, a population-based cohort study from the Netherlands. Br J Clin Pharmacol 65(4):600–606
Kallen B, Nilsson E, Olausson PO (2011) Antidepressant use during pregnancy: comparison of data obtained from a prescription register and from antenatal care records. Eur J Clin Pharmacol 67(8):839–845
Tanner K, Sabrine N, Wren C (2005) Cardiovascular malformations among preterm infants. Pediatrics 116(6):e833–e838
Toh S, Mitchell AA, Werler MM, Hernández-Díaz S (2008) Sensitivity and specificity of computerized algorithms to classify gestational periods in the absence of information on date of conception. Am J Epidemiol 167(6):633–640
Cole JA, Modell JG, Haight BR, Cosmatos IS, Stoler JM, Walker AM (2007) Bupropion in pregnancy and the prevalence of congenital malformations. Pharmacoepidemiol Drug Saf 16(5):474–484
Espnes MG, Bjørge T, Engeland A (2011) Comparison of recorded medication use in the Medical Birth Registry of Norway with prescribed medicines registered in the Norwegian Prescription Database. Pharmacoepidemiol Drug Saf 20:243–248
Stephansson O, Granath F, Svensson T (2011) Drug use during pregnancy in Sweden–assessed by the Prescribed Drug Register and the Medical Birth Register. Clin Epidemiol 3:43–50
Olesen C, Sondergaard C, Thrane N, Lauge Nielsen G, de Jong-van den Berg L, Olsen J et al (2001) Do pregnant women report use of dispensed medications? Epidemiology 12(5):497–501
Acknowledgments
JLM was supported by a Heart Foundation South Australian Cardiovascular Research Network Fellowship (CR10A4988).
Conflict of interest
The authors declare that they have no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grzeskowiak, L.E., Gilbert, A.L. & Morrison, J.L. Exposed or not exposed? Exploring exposure classification in studies using administrative data to investigate outcomes following medication use during pregnancy. Eur J Clin Pharmacol 68, 459–467 (2012). https://doi.org/10.1007/s00228-011-1154-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-011-1154-9