Abstract
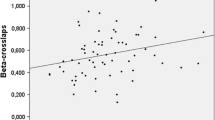
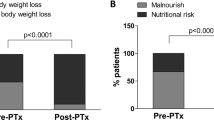
The hypercalciuria evolution and other bone metabolism parameters were evaluated in patients with tuberculosis after treatment. Twenty-two patients with tuberculosis and 54 normal subjects were studied; they consumed an average diet (calcium intake 1000 mg/day). Ten of these patients and nine normal subjects were also studied after a low calcium diet (400 mg/calcium/day) and after a load of oral calcium of 1000 mg (calcium absorption test). The study with an average diet was performed after 1 week (basal) and 3, 6, and 12 months after the antituberculosis treatment was started; the calcium absorption test was carried out 2 weeks, 3 and 12 months after the treatment was started. On an average diet, patients with tuberculosis presented, at baseline state, lower calcidiol levels than normal controls. Serum calcitriol levels at baseline were higher than at 6 and 12 months. Serum parathyroid hormone (PTH) levels in patients with tuberculosis were lower than in normal controls at baseline, but these levels were similar to controls at 3, 6, and 12 months after treatment. During the calcium absorption test and under basal conditions, patients with tuberculosis showed lower serum PTH and calcidiol levels in all the dietetic situations than in normal controls. However, serum calcitriol levels were higher than in controls after the restrictive diet. After 3 months of treatment, urinary calcium excretion was normal in patients with tuberculosis during the average and low diets, but higher than in control group after calcium load. After 12 months of treatment, all the biochemical parameters of the patients with tuberculosis were similar to the control group under all the dietetic situations. These data indicate that antituberculous treatment, although it may contribute to the production of some alteration in the calcium and vitamin D metabolism, basically favors the correction of disturbances associated with tuberculosis.
Similar content being viewed by others
References
Martinez ME, Gonzalez J, Sanchez-Cabezudo MJ, Peña JM, Vazquez JJ, Felsenfeld A (1993) Evidence of absorption hypercalciuria in tuberculosis patients. Calcif Tissue Int 53:384–387
Candranel J, HAJ, Milleron B, Paillard F, Akoun G, Garabedian M (1988) Vitamin D metabolism in tuberculosis: producstion of 1,25(OH)D3 by cells recovered by bronchoalveolar lavage and the role of this metabolite in calcium homeostasis. Am Rev Resp Dis 138:984–989
Adams JS, Motlin RL, Diaz MM, Barnes TF (1989) Potentiation of the macrophage 25-hydroxy vitamin D hydroxylation reaction by human tuberculous pleural fluid. J Clin Endocrinol Metab 64:457–460
CadranelJ, Garabedian M, Milleron B, Guilloso H, AknounG, HanceAJ (1990) 1-25(OH)2D3 production by T lymphocytes and alveolar macrophages recovered by lavage from normocalcemic patients with tuberculosis. J Clin Invest 85: 1588–1593
Felsenfeld A, Drezner MK, Llack F (1986) Hypercalcemia and elevated calcitriol in maintenance dialysis patients with tuberculosis. Arch Intern Med 146:1941–1945
Pouchot J, Dreyfuss D, Gorden JP, Mier L, Remy P, Esdaile JM, Coste F, Vinceneux P (1993) Ectopic production of 1,25-dihydroxyvitamin D3 in tuberculosis. Nephrol Dial Transplant 8:560–562
Brodie MJ, Boobis AR, Dollery CT, Hillyard CJ, Brown DJ, Macintyre I, Park BK (1980) Rifampin and vitamin D metabolism. Clin Pharmacol Ther 27:810–814
Brodie MJ, Boobis AR, Hillyard CJ, Abeyasekera G, Stevenson JC, Macintyre I, Park BK (1982) Clin Pharmacol Ther 32:525–531
Williams SE, Wardman AG, Taylor GA, Peacock M, Cooke NJ (1985) Long-term study of the effects of rifampicin and isoniaziid on vitamin D metabolism. 66:49–54
Davies PD, Brown RC, Church HA, Woodhead JS (1987) The effect of antituberculosis chemotherapy on vitamin D and calcium metabolism. Tubercle 68:261–266
Perry W, Brown J, Eroogo MA, Stang TCB (1982) Calcium metabolism during rifampicin and isoniazid therapy for tuberculosis. JR Soc Med 75:533–536
Martinez ME, Miguel JL, Selgas R, Balaguer G, Catalan P, Carmona AR, Sanchez Sicilia L (1986) Compensating by solar irradiation of depletion of 25(OH)D in CAPD patients. Nephron 42:268–269
Bell NH, Shaw S, Turner RT (1984) Evidence that 1-25 dihydroxyvitamin D3 inhibits the hepatic production of 25-hydroxyvitamin D in man. J Clin Invest 74:1540–1544
Chan TY, Poon P, Pang J, Swaninathan R, Chan-CH, Nisar M, Williams CS, Davies PD (1994) A study of calcium and vitamin D metabolism in Chinese patients with pulmonary tuberculosis. J Trop Med Hyg 97(1):26–30
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Martinez, M.E., Gonzalez, J., Sanchez-Cabezudo, M.J. et al. Remission of hypercalciuria in patients with tuberculosis after treatment. Calcif Tissue Int 59, 17–20 (1996). https://doi.org/10.1007/s002239900078
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s002239900078