Abstract
Vertebral fractures (VFx) occur most frequently in the mid-thoracic and thoraco-lumbar regions, which experience the highest mechanical loading along the spine. The prevalence and incidence of VFx by their location and severity, and their relationship with bone mineral density (BMD), are seldom reported in randomized clinical trial cohorts. The VERO trial randomized 1360 postmenopausal women with at least two moderate or one severe VFx to receive either teriparatide or risedronate for up to 24 months. In this post hoc analysis, we describe the centrally read distribution and severity of prevalent and incident VFx, and the association of their location with the baseline BMD. At baseline, 21.4% of all evaluable vertebral bodies had a prevalent VFx; most commonly at L1, T12, L2 and T11 (38.5%, 37.4%, 25.3% and 23.5% of patients, respectively). Patients with prevalent VFx only at T12/L1 showed a higher baseline BMD compared to patients with VFx at other levels. At month 24, 100 patients had 126 incident VFx (teriparatide: 35; risedronate: 91). The most frequent incident VFx occurred at T12 (n = 17, 1.6% of patients), followed by L1 and T11 (n = 14, 1.3% both). The frequency of incident VFx was lower at all vertebral levels in patients given teriparatide. These results confirm prior reports that VFx occurs more frequently at mid-thoracic and thoraco-lumbar regions of the spine. Patients with these VFx locations have higher BMD than those who fracture at other sites, suggesting a role for mechanical stress in the etiology of VFx. Teriparatide is superior to risedronate in the prevention of VFx at these common fracture locations.
Trial registration ClinicalTrials.gov Identifier: NCT01709110
Similar content being viewed by others
Introduction
Osteoporosis is characterized by a microarchitectural deterioration of bone tissue and increased skeletal fragility [1]. Vertebral fractures (VFx) are the most common osteoporotic fracture [2]. Approximately, 30–50% of women and 20–30% of men will develop VFx during their lives with half experiencing multiple VFx [3,4,5]. Although most VFx are detected during the investigation of back pain, a significant number are incidentally detected during workup of patients without pain [6, 7]. However, both symptomatic and asymptomatic VFx are associated with increased morbidity and mortality [8,9,10], and are the main risk factor for developing new vertebral and other osteoporotic fractures [11, 12]. This underscores the importance of accurately diagnosing osteoporotic VFx.
The frequency of VFx varies depending on the vertebral level. Population-based studies from different geographies have shown a similar bimodal pattern of prevalent and incident VFx [13,14,15,16]. In the Rochester Epidemiology Project of 300 women over the age of 50 years, there was a concentration of prevalent VFx in the mid-thorax and thoraco-lumbar region [13]. The EVOS study, involving 13,562 men and women over the age of 50 years recruited from the general population in 30 European centers, established the highest prevalence of VFx at the mid-thoracic (T6–T8) and the thoraco-lumbar region (T12–L1) [14]. Similarly, bimodal peaks in the distribution of incident vertebral fractures were observed in the Rotterdam study comprising nearly 3500 men and women over the age of 55 years; T12 and L1 were the most commonly fractured vertebrae [16]. However, results from controlled clinical trials on the prevalence and incidence of VFx, by vertebral level and severity, and their relationship to bone mineral density (BMD) are sparse. Additionally, whether teriparatide, a bone-forming drug, has a similar effect on VFx in different locations of the spine with potentially different loading characteristics has not been studied.
The vertebral fracture treatment comparisons in osteoporotic women (VERO) trial was the first active-controlled, double-dummy study that included fracture outcomes as the primary endpoint in postmenopausal women with severe osteoporosis. The trial compared the treatment effects of teriparatide, with those of risedronate. Results from VERO showed compelling evidence that teriparatide was associated with a lower risk of new vertebral and clinical fractures at month 12 and month 24 [17, 18]. Spine X-rays were centrally evaluated by radiologists (blinded to study treatments) using predefined, stringent criteria for the diagnosis of vertebral fracture. Here, we present the results from a post hoc analysis of VERO that aimed to describe the distribution of prevalent, and new and/or worsening incident vertebral fractures by their location in the spine and their severity. We analyzed the association between the VFx location and the BMD at hip and spine. We also report the treatment effects of teriparatide versus risedronate on new VFx, separately analyzing those vertebral levels with highest rate of VFx and highest mechanical loading.
Methods
Study Design and Participants
The study design of VERO has previously been described in detail [17]. In summary, VERO was an international, multicenter, randomized, double-blind, active-controlled, parallel-group, 24-month trial. Postmenopausal women with severe osteoporosis were randomized following a 1:1 scheme to receive either injectable subcutaneous teriparatide (20 µg daily) plus an oral weekly placebo, or oral risedronate (35 mg weekly) plus an injectable subcutaneous daily placebo for up to 24 months. Patients were enrolled at 116 centers in 14 countries across Europe, South and North America.
Eligible participants were ambulatory postmenopausal women aged > 45 years with a baseline BMD T-score less than or equal to − 1.50 standard deviations (SD) at the femoral neck, total hip, or lumbar spine, assessed at the study site. Patients had to have radiographic evidence of at least two moderate (a reduction in vertebral body height of 26–40%) or one severe (> 40% reduction) prevalent vertebral fragility fracture according to the classification of Genant et al. [19]. Patients were excluded if they had: (a) low serum 25-hydroxy-vitamin D (25OHD) levels (< 9.2 ng/mL or 23 nmol/L), (b) abnormally elevated serum intact parathyroid hormone (PTH [1–84]) at baseline (> 72 pg/mL or > 7.6 pmol/L), or (c) significantly impaired renal function as defined by a calculated endogenous creatinine clearance of < 30 mL/min/m2. Prior use of bisphosphonates or other osteoporosis drugs was allowed.
An incident VFx was defined as a vertebral body height loss of at least 20% (and 4 mm) of a vertebra that was unfractured at baseline. This assessment was based on a 6-point measurement of the vertebral bodies from T4 to L4, and confirmed by an increase by one or more severity grades per the semiquantitative grading (SQ) scale by Genant et al. [19]. Worsening of a baseline pre-existing VFx was diagnosed if the decrease in vertebral height was at least one severity grade in the SQ assessment. All VFx were centrally adjudicated by two radiologists blinded to treatment (BioClinica, San Francisco, CA, USA).
A recent bisphosphonate use was defined as: (a) a total of six or more months of treatment with any oral bisphosphonate, either intermittently or continuously, within 3 years prior to screening, or (b) intravenous zoledronic acid at any dose within 4 years of screening, or (c) intravenous ibandronate or pamidronate at any dose within 12 months prior to screening. A patient was considered as having a recent clinical vertebral fragility fracture if she had at least one painful vertebral fragility fracture within the 12 months prior to the screening visit.
In this post- hoc analysis, we describe the distribution of prevalent vertebral fractures at baseline according to their location and severity. Further, the incident new and/or worsening vertebral fractures were assessed at month 12 and month 24 based on their location and treatment arms. An additional analysis was performed to estimate the association between baseline lumbar spine, femoral neck and total hip BMD scores and the vertebral fracture location at baseline in three predefined patient subgroups: (a) patients with at least one prevalent fracture at T12 and/or L1 and no fractures at any other vertebral body (Group A), (b) patients with prevalent fractures at any vertebral site different from T12 and/or L1 (Group B), and (c) patients with at least one prevalent fracture at T12 and/or L1 and at least one fracture at any other vertebral site (Group C).
Statistical Analyses
Continuous baseline characteristics were summarized as mean and SD, and categorical variables were presented as counts and percentages. The Chi-square test of independence and Wald tests from simple lineal regression analyses were used to compare baseline demographic, and clinical characteristics, including baseline BMD, among the three predefined groups of patients defined based on the location of the prevalent VFx. Additionally, two-sample Chi-square tests for equality of proportions without continuity corrections were used for pairwise comparisons between the groups. The association of the baseline BMD with the fracture location was estimated with an adjusted multivariable linear regression model including patient group (according to VFx location), age (years) and weight (kilograms). No correction for the multiplicity of the test was applied. Two-sided p values were reported, and a p value < 0.05 was considered as a statistically significant result. Analyses were conducted using SAS version 9·4.
Results
In total, 1360 patients were assessed for spine X-rays, including 17,413 evaluable vertebral bodies, at baseline. Central readers could not evaluate 267 (1.5%) vertebral bodies due to insufficient quality of the X-ray image (presence of artefacts, incorrect patient positioning or patient motion). At months 12 and 24, 1159 and 1049 patients were assessed for a total of 14,987 and 13,454 evaluable vertebral bodies, respectively. Mean (SD) age at baseline was 72.1 (8.7) years (min–max: 45–93 years; Table 1). The mean (SD) number of prevalent vertebral fractures by patient was 2.7 (2.0).
At baseline, 21.4% of all evaluable vertebral bodies had a prevalent VFx. These fractures were predominantly located at L1, T12, L2, T11 and T8 (38.5%, 37.4%, 25.3%, 23.5% and 23.1% of the patients, respectively; Fig. 1). A total of 524 (3.0%) of all assessed vertebral bodies had a prevalent fracture at L1, which was the most frequently affected level; this was followed by 509 (2.9%) fractures at T12, 344 (2.0%) fractures at L2, and 320 and 314 (1.8% each) fractures at T11 and T8, respectively. The majority of prevalent vertebral fractures, particularly at T12 (66.2%) and L1 (65.5%) levels, were severe (SQ3) according to the Genant classification [19] (Fig. 1).
Patients with at least one prevalent VFx at T12 and/or L1 and at least one fracture at another vertebral level (Group C) were statistically significantly older, and had shorter stature than patients in Group A (with at least one prevalent fracture at T12 and/or L1 and no fractures in any other vertebral body), and patients in Group B (with prevalent fractures at any level other than T12 and/or L1) (Table 1). Patients in Group C also showed a higher frequency of pre-randomization recent clinical VFx (41.6%) than patients in the other two groups (32.6% and 34.1% in Group A and B, respectively; Table 1).
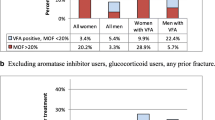
In contrast, the patients who had prevalent fractures at the most commonly fractured sites (T12 and/or L1 only, Group A), showed a statistically significant higher BMD at the lumbar spine and the total hip than the other two groups (Table 1 and Fig. 2). The multivariable model adjusted by age and body weight yielded similar results (Supplemental Table 1).
Baseline bone mineral density for lumbar spine, femoral neck and total hip by prevalent vertebral fracture locations. Group A: patients with at least one prevalent fracture at T12 and/or L1 and no fractures at any other vertebral body; Group B: patients with prevalent fractures at any vertebral site different from T12 and/or L1; Group C: patients with at least one prevalent fracture at T12 and/or L1 and at least one fracture at any other vertebral site. *p = 0.002 Group A versus Groups B and C; **p < 0.001 Group C versus Groups A and B; ***p < 0.05 Group B versus Group A. Differences in bone mineral density (g/cm2) between the different groups were estimated with a simple linear regression model. Pairwise comparisons were performed to estimate the differences between the groups and p values obtained from the corresponding Wald test. No correction for multiplicity testing was applied
At Month 12, 53 patients (4.6%) had 73 new and/or worsened incident VFx (25 and 48 in the teriparatide and risedronate groups, respectively). Over the full 24-month trial, 100 patients (9.5%) had 126 new and/or worsened incident VFx (35 and 91 in the teriparatide and risedronate groups, respectively). The most frequent new VFx during the 24-month study was T12 (17/1049: 1.6% of patients; 13.5% of all new fractures), followed by L1 and T11 (14/1049: 1.3% both), T9 (13/1049: 1.2%), and T8 (12/1049: 1.1%).
Of the 100 patients presenting with new and/or worsened incident VFx during of the study, 89 patients had a new moderate (SQ2) or severe (SQ3) incident VFx. The percentage of incident VFx was lower at all levels with teriparatide at month 24 (Fig. 3).
Discussion
The most common location of prevalent VFx in the VERO cohort of postmenopausal women with severe osteoporosis, confirms previous reports from population-based radiographic epidemiological surveys, as well as the results of the Vertebral Fracture Arm of the FIT trial [20]. The two most common VFx locations at the baseline visit involved the thoraco-lumbar union, with nearly 40% of the enrolled patients having a prevalent fracture at L1 and/or T12. The semiquantitative analysis also revealed that the more severe (SQ3) VFx, corresponding to a vertebral body height loss more than 40% according to the classification by Genant et al. [19], occurred at these very same vertebral levels. Surgical series evaluating kyphoplasty and vertebroplasty procedures also identified the thoraco-lumbar junction as the most common location for severe VFx and the levels most commonly subjected to cement augmentation in the absence of metastatic bone disease [21,22,23,24].
Biomechanical models developed to explain variations on the location of VFx suggest that these variabilities arise from location-specific loading during different activities of daily living. Mid-thoracic and thoraco-lumbar regions were found to experience preferentially higher mechanical loading than other regions of the spine due to the selective activation of the multifidus muscle fascicles in the thoraco-lumbar region [25]. Additionally, high-thoracic kyphosis occurring around T7–T8 may account for greater anterior bending moments and increased compressive and shear forces in this region [26]. The increased incidence of fractures at the thoraco-lumbar junction might also be the consequence of higher load-bearing in this region due to the absence of rib cage support [27].
We have also found that patients who had a prevalent VFx at the most common sites in our series (T12 and/or L1) (Group A), coincides with the vertebrae with the highest load-bearing forces [25]. Patients with fractures at T12 and/or L1 demonstrate statistically significant higher spine and total hip BMD than patients with prevalent vertebral fractures at any other levels (Group B), and in patients with fractures at T12/L1 and any other spine level (Group C). Previous studies have shown that the association between spine and proximal femur BMD and VFx differ according to the affected vertebral level. Nevitt et al. [20] analyzed 6802 patients from the Vertebral Fracture Arm of the FIT trial and showed that each SD decrease in spinal BMD was associated with a 2.1 times greater odds of new VFx in the upper spine (T4–T10), compared with 1.5 times for the lower spine (T11–L4) with a statistically significant difference between the two ratios. Similar results were found for femoral neck BMD. Using QCT-based volumetric BMD, Anderson et al. [28] showed that upper spine (T4–T10) fractures appear to be more strongly related with BMD than lower spine (T11–L4) fractures. These results suggest that the effects of loading and mechanical stress may be more relevant to fracture risk than the areal BMD at thoraco-lumbar junction level. It should be noted that the lumbar spine BMD analyses in VERO excluded vertebrae affected by VFx or other artifacts.
As expected, subjects in Group C (patients with at least one prevalent fracture at T12 and/or L1 and at least one fracture at other vertebral site) showed the lowest BMD values at all sites (spine, femoral neck and total hip).
Our analysis of the prospective phase of VERO yielded consistent results in the location of the newly diagnosed VFx, that were more common at the higher load-bearing levels, including the mid-thoracic and the thoraco-lumbar regions (Fig. 3). At all spinal levels analyzed (T4 to L4), patients receiving teriparatide showed a lower incidence of incident fractures compared to risedronate. However, the biggest absolute reductions in VFx risk in teriparatide-treated patients occurred at the higher load-bearing levels, including the mid-thoracic and the thoraco-lumbar regions (Fig. 3). These vertebral levels are at the highest risk for fractures, with the largest absolute risk reductions of teriparatide versus risedronate occurring at T9 (− 1.7%) and T12 (− 1.3%) (Fig. 3). These findings suggest that the antifracture effects of teriparatide are more pronounced in the most loaded vertebrae compared with risedronate which shows a more even distribution of antifracture efficacy in both loaded and unloaded vertebrae.
Our analysis has some limitations. The definitions of the three groups by VFx location and number according to observed vertebral-level fracture frequency, are somewhat arbitrary, but are consistent with the observed peak in fracture prevalence at T12 and L1. Alternative subgroup definitions based on mid-thoracic VFx were not considered given the low numbers of fractures and subsequently limited the statistical power. We did not evaluate kyphosis, which may influence compressive forces along the spine. Given the inclusion criteria in VERO, mild VFx (i.e. those with a vertebral body height loss of 20–25%) are likely under-represented in the analysis of prevalent fractures. Therefore, our results may not be generalized to patients with fewer or less-severe VFx. However, the analysis of only moderate and severe VFx reduces the potential error in the adjudication of VFx and increases the clinical relevance of the findings since moderate/severe VFx are more strongly associated with clinical fracture and increased future fracture risk [29]. Moreover, the distribution of prevalent and incident VFx in the VERO study is similar when compared with study cohorts with less-severe osteoporosis or those randomly selected from the general population [3,4,5,6,7,8,9].
Strengths of our study include the centralized radiological evaluation of the spine radiographs, that was carried out by radiologists blinded to study treatments, using strict quantitative and semiquantitative definitions for incident VFx. Furthermore, VERO was conducted in a double-blind double-dummy format with a primary endpoint of VFx, which is the most rigorous study design.
The prevalent and incident VFx location data from VERO confirm with previous findings from epidemiological studies and interventional trials that these fractures occur most frequently in the mid-thoracic and thoraco-lumbar regions of the spine. It has been suggested that fractures in these locations are dependent to a greater degree on mechanical loading of the vertebrae. Our data confirm that patients with fractures in these most common and most loaded locations have higher BMD than patients with VFx in other locations. The observation that teriparatide is more effective at preventing VFx at these highly loaded vertebrae may suggest a synergy between teriparatide anabolic effect with increased mechanical loading, as it has been suggested in animal models [30, 31]. A recent meta-analysis of hip fracture in clinical trials comparing teriparatide to placebo or active comparator showed that hip fractures were reduced by 56% but that the effect in upper extremity fractures was neutral. This possibly supports the hypothesis that higher mechanical loading enhances teriparatide antifracture efficacy [32].
In conclusion, we provide supportive evidence for data documenting the most frequent location of VFx being at vertebral levels likely to bear the highest load, and that teriparatide versus risedronate may demonstrate synergy with mechanical load in offering greater protection to vertebrae experiencing the highest loading.
References
Black DM, Rosen CJ (2016) Clinical practice. Postmenopausal osteoporosis. N Engl J Med 374:254–262. https://doi.org/10.1056/NEJMcp1513724
Ensrud KE, Schousboe JT (2011) Vertebral fractures. N Engl J Med 364:1634–1642. https://doi.org/10.1056/NEJMcp1009697
O'Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1018. https://doi.org/10.1002/jbmr.5650110719
Davies KM, Stegman MR, Heaney RP, Recker RR (1996) Prevalence and severity of vertebral fracture: the Saunders County Bone Quality Study. Osteoporos Int 6:160–165
Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ 3rd (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–227. https://doi.org/10.1002/jbmr.5650070214
Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL, Group IS (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20:557–563. https://doi.org/10.1359/JBMR.041214
Bartalena T, Rinaldi MF, Modolon C, Braccaioli L, Sverzellati N, Rossi G, Rimondi E, Busacca M, Albisinni U, Resnick D (2010) Incidental vertebral compression fractures in imaging studies: lessons not learned by radiologists. World J Radiol 2:399–404. https://doi.org/10.4329/wjr.v2.i10.399
Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC, Black DM (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 48:241–249. https://doi.org/10.1111/j.1532-5415.2000.tb02641.x
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220. https://doi.org/10.1001/archinte.159.11.1215
Nevitt MC, Thompson DE, Black DM, Rubin SR, Ensrud K, Yates AJ, Cummings SR (2000) Effect of alendronate on limited-activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Fracture Intervention Trial Research Group. Arch Intern Med 160:77–85. https://doi.org/10.1001/archinte.160.1.77
Lindsay R, Silverman SL, Cooper C, Hanley DA, Barton I, Broy SB, Licata A, Benhamou L, Geusens P, Flowers K, Stracke H, Seeman E (2001) Risk of new vertebral fracture in the year following a fracture. JAMA 285:320–323. https://doi.org/10.1001/jama.285.3.320
Siris ES, Genant HK, Laster AJ, Chen P, Misurski DA, Krege JH (2007) Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos Int 18:761–770. https://doi.org/10.1007/s00198-006-0306-8
Melton LJ 3rd, Kan SH, Frye MA, Wahner HW, O'Fallon WM, Riggs BL (1989) Epidemiology of vertebral fractures in women. Am J Epidemiol 129:1000–1011. https://doi.org/10.1093/oxfordjournals.aje.a115204
Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, O'Neill TW (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Marwaha RK, Tandon N, Gupta Y, Bhadra K, Narang A, Mani K, Mithal A, Kukreja S (2012) The prevalence of and risk factors for radiographic vertebral fractures in older Indian women and men: Delhi Vertebral Osteoporosis Study (DeVOS). Arch Osteoporos 7:201–207. https://doi.org/10.1007/s11657-012-0098-8
Van der Klift M, De Laet CE, McCloskey EV, Hofman A, Pols HA (2002) The incidence of vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res 17:1051–1056. https://doi.org/10.1359/jbmr.2002.17.6.1051
Kendler DL, Marin F, Zerbini CAF, Russo LA, Greenspan SL, Zikan V, Bagur A, Malouf-Sierra J, Lakatos P, Fahrleitner-Pammer A, Lespessailles E, Minisola S, Body JJ, Geusens P, Möricke R, López-Romero P (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391(10117):230–240. https://doi.org/10.1016/s0140-6736(17)32137-2
Body JJ, Marin F, Geusens P, Zerbini C, Fahrleitner-Pammer A, Moericke R, Casado E, Stepan JJ, Minisola S, Lespessailles E, López-Romero P, Kendler DL (2018) Efficacy of teriparatide compared with risedronate on FRAX®-defined major osteoporotic fractures: a post-hoc analysis of the VERO clinical trial. J Bone Miner Res 33(Suppl 1):113
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148. https://doi.org/10.1002/jbmr.5650080915
Nevitt MC, Ross PD, Palermo L, Musliner T, Genant HK, Thompson DE (1999) Association of prevalent vertebral fractures, bone density, and alendronate treatment with incident vertebral fractures: effect of number and spinal location of fractures. The Fracture Intervention Trial Research Group. Bone 25:613–619. https://doi.org/10.1016/s8756-3282(99)00202-1
Coumans JV, Reinhardt MK, Lieberman IH (2003) Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg 99(1 Suppl):44–50. https://doi.org/10.3171/spi.2003.99.1.0044
Trout AT, Kallmes DF, Kaufmann TJ (2006) New fractures after vertebroplasty: adjacent fractures occur significantly sooner. Am J Neuroradiol 27:217–223
Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, Eastell R, Shabe P, Talmadge K, Boonen S (2009) Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 373(9668):1016–1024. https://doi.org/10.1016/S0140-6736(09)60010-6
Martinez-Ferrer A, Blasco J, Carrasco JL, Macho JM, Roman LS, Lopez A, Monegal A, Guañabens N, Peris P (2013) Risk factors for the development of vertebral fractures after percutaneous vertebroplasty. J Bone Miner Res 28:1821–1829. https://doi.org/10.1002/jbmr.1899
Bruno AG, Burkhart K, Allaire B, Anderson DE, Bouxsein ML (2017) Spinal loading patterns from biomechanical modeling explain the high incidence of vertebral fractures in the thoracolumbar region. J Bone Miner Res 32:1282–1290. https://doi.org/10.1002/jbmr.3113
Briggs AM, van Dieen JH, Wrigley TV, Greig AM, Phillips B, Lo SK, Bennell KL (2007) Thoracic kyphosis affects spinal loads and trunk muscle force. Phys Ther 87:595–607. https://doi.org/10.2522/ptj.20060119
Christiansen BA, Bouxsein ML (2010) Biomechanics of vertebral fractures and the vertebral fracture cascade. Curr Osteoporos Rep 8:198–204. https://doi.org/10.1007/s11914-010-0031-2
Anderson DE, Demissie S, Allaire BT, Bruno AG, Kopperdahl DL, Keaveny TM, Kiel DP, Bouxsein ML (2014) The associations between QCT-based vertebral bone measurements and prevalent vertebral fractures depend on the spinal locations of both bone measurement and fracture. Osteoporos Int 25:559–566. https://doi.org/10.1007/s00198-013-2452-0
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, Adachie JD (2003) Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone 33:522–532. https://doi.org/10.1016/S8756-3282(03)00241-2
Li J, Duncan RL, Burr DB, Gattone VH, Turner CH (2003) Parathyroid hormone enhances mechanically induced bone formation, possibly involving L-type voltage-sensitive calcium channels. Endocrinology 144:1226–1233. https://doi.org/10.1210/en.2002-220821
Sugiyama T, Saxon LK, Zaman G, Moustafa A, Sunters A, Price JS, Lanyon LE (2008) Mechanical loading enhances the anabolic effects of intermittent parathyroid hormone (1–34) on trabecular and cortical bone in mice. Bone 43:238–248. https://doi.org/10.1016/j.bone.2008.04.012
Díez-Pérez A, Marin F, Eriksen EF, Kendler DL, Krege JH, Delgado-Rodríguez M (2018) Effects of teriparatide on hip and upper limb fractures in patients with osteoporosis: a systematic review and meta-analysis. Bone 120:1–8. https://doi.org/10.1016/j.bone.2018.09.020
Acknowledgements
We are indebted to Anja Gentzel-Jorczyk (Clinical Trial Coordinator), Estrella Crespo and Laura Briones (Data Management) for their contribution to the study, Richi Taneja, Eli Lilly Services India Pvt Ltd, for the editorial assistance, the members of the investigational teams at the study centers, and the women who participated in the study.
Funding
The Eli Lilly and Company funded the VERO clinical trial.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by PG, FM and PL-R. The first draft of the manuscript was written by PG, FM and PL-R, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Geusens received consultant and/or speaker fees from Lilly, and research support from Pfizer, Abbott, Lilly, Amgen, MSD, Roche, UCB, BMS, Mylan and Novartis. Dr. Kendler received honoraria, research grants, and/or consultant fees from Amgen, Lilly, Radius, Pfizer, and UCB. Dr. Fahrleitner-Pammer received speaker fees from Amgen, Alexion, BMS, Lilly, Fresenius, Sandoz, Shire and UCB. Drs. Marin and López-Romero are employees and shareholders of Lilly.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The following investigators randomized at least one patient in the VERO trial: Argentina: A. Alvarisqueta, A. Bagur, C. Gómez, L. Maffei, F. Massari; Austria: E. Boschitz, A. Fahrleitner-Pammer, G. Höfle, H. Koller, C. Muschitz, E. Preisinger; Belgium: I. Beyer, J.J. Body, K. de Vlam, V. Gangji, P. Geusens, E. Gielen, S. Goemare, M. Leon, J.-Y. Reginster, M. Van den Berghe, R. Witvrouw; Brazil: J. Borges, M. Castro, L.A. Russo, C.A. Zerbini; Canada: J. Adachi, J.P. Brown, A. Cheung, S. Kaiser, A. Karaplis, D.L. Kendler, F. Morin, W. Olszynski, S. Seigel; Czech Republic: E. Dokoupilova, M. Ladova, R. Pikner, J. Stepan, V. Zikan; France: R. Chapurlat, J. Fulpin, C. Marcelli, M. Laroche, E. Lespessailles, T. Thomas; Germany: G. Dahmen, J. Fakler, I. Frieling, P. Hadji, R. Möricke, F. Thomasius, L. Unger, V. Ziller; Greece: M. Daniilidis, E. Foufoulas, G. Ioannidis, M. Kita, I. Kyrkos, I. Panagiotopoulos, S. Pnevmaticos; Hungary: E. Kanakaridu, K. Kudlak, P. Lakatos, K. Nagy, P. Somogyi, P. Suranyi, Z. Valkusz; Italy: G. Bianchi, M.L. Brandi, S. Giannini, G. Isaia, S. Minisola, G. Osella, M. Rossini; Poland: T. Blicharski, J. Brzezicki, P. Leszczynski, M. Mazurek, M. Rell-Bakalarska, J. Supronik; Spain: M.J. Amerigo, M. Bernad, E. Casado, N. Chozas, M. Díaz-Curiel, J. Malouf-Serra, J.A. Román, F.J. Tarazona; USA and Puerto Rico: N. Binkley, M. Bolognese, P. Bressler, M. Carroll, A. Chang, D. Cox, A. de la Llana, A. Dulgeroff, H. El-Kadi, M. Goldberg, S. Greenspan, H. Kenney, A. Kivitz, M.E. Lewiecki, M. Lillestol, P. Miller, A. Myers, P. Norwood, M. Perini, S. Rao, R.R. Recker, C.P. Recknor, H. Rodríguez, K.G. Saag, R. Sachson, C. Shuhart, O. Soto-Raíces, M. Spiegel.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Geusens, P., Kendler, D.L., Fahrleitner-Pammer, A. et al. Distribution of Prevalent and Incident Vertebral Fractures and Their Association with Bone Mineral Density in Postmenopausal Women in the Teriparatide Versus Risedronate VERO Clinical Trial. Calcif Tissue Int 106, 646–654 (2020). https://doi.org/10.1007/s00223-020-00683-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-020-00683-6