Abstract
Rationale
Epidemiological data indicate that drivers testing positive for an opioid drug are twice as likely to cause a fatal car crash; however, there are limited controlled data available.
Objectives
The primary aim of this study was to assess the effects of a therapeutic dose range of oxycodone alone and in combination with alcohol on simulated driving performance.
Methods
Healthy participants (n = 10) completed this within-subject, double-blind, placebo-controlled, randomized outpatient study. Six 7-h sessions were completed during which oxycodone (0, 5, 10 mg, p.o.) was administered 30 min before alcohol (0, 0.8 g/kg (15% less for women), p.o.) for a total of 6 test conditions. Driving assessments and participant-, observer-rated, psychomotor and physiological measures were collected in regular intervals before and after drug administration.
Results
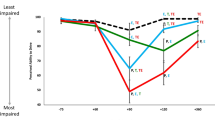
Oxycodone alone (5, 10 mg) did not produce any changes in driving outcomes or psychomotor task performance, relative to placebo (p > 0.05); however, 10 mg oxycodone produced increases in an array of subjective ratings, including sedation and impairment (p < 0.05). Alcohol alone produced driving impairment (e.g., decreased lateral control) (p < 0.05); however, oxycodone did not potentiate alcohol-related driving or subjective effects.
Conclusions
These preliminary data suggest that acute doses of oxycodone (5, 10 mg) do not significantly impair acuity on laboratory-based simulated driving models; however, 10 mg oxycodone produced increases in self-reported outcomes that are not compatible with safe driving behavior (e.g., sedation, impairment). Additional controlled research is needed to determine how opioid misuse (higher doses; parenteral routes of administration) impacts driving risk.



Similar content being viewed by others
References
American Pain Society. Pain management and dosing guide. 2016. http://americanpainsociety.org/uploads/education/PAMI_Pain_Mangement_and_Dosing_Guide_02282017.pdf
Babalonis S, Lofwall MR, Nuzzo PA, Siegel AJ, Walsh SL (2013) Abuse liability and reinforcing efficacy of oral tramadol in humans. Drug Alcohol Depend 129(1-2):116–124
Babalonis S, Hampson AJ, Lofwall MR, Nuzzo PA, Walsh SL (2015) Quinine as a potential tracer for medication adherence: a pharmacokinetic and pharmacodynamic assessment of quinine alone and in combination with oxycodone in humans. J Clin Pharmacol 55(12):1332–1343
Bernhoft IM, Hels T, Lyckegaard A, Houwing S, Verstraete AG (2012) Prevalence and risk of injury in Europe by driving with alcohol, illicit drugs and medicines. Procedia Soc Behav Sci 48:2907–2916
Berning A, Compton R, Wochinger K (2015) Results of the 2013–2014 National Roadside Survey of alcohol and drug use by drivers. Traffic Safety Facts Research Note. Report No. DOT HS 812 118. National Highway Traffic Safety Administration, Washington, DC
Brown TL, Milavetz G, Gaffney G, Spurgin A (2018) Evaluating drugged driving: effects of exemplar pain and anxiety medications. Traffic Inj Prev 19:S97–S103
Chihuri S, Li G (2017a) Use of prescription opioids and motor vehicle crashes: a meta analysis. Accid Anal Prev 109:123–131
Chihuri S, Li G (2017b) Trends in prescription opioids detected in fatally injured drivers in 6 US states: 1995-2015. Am J Public Health 107:1487–1492
Chihuri S, Li G (2019) Use of prescription opioids and initiation of fatal 2-vehicle crashes. JAMA Netw Open 2:e188081
Esser MB, Guy GP Jr, Zhang K, Brewer RD (2019) Binge drinking and prescription opioid misuse in the US, 2012–2014. Am J Prev Med 57:197–208
Ferreira DH, Boland JW, Phillips JL, Lam L, Currow DC (2018) The impact of therapeutic opioid agonists on driving-related psychomotor skills assessed by a driving simulator or an on-road driving task: a systematic review. Palliat Med 32:786–803
Fraser HF, Van Horn GD, Martin WR, Wolbach AB, Isbell H (1961) Methods for evaluating addiction liability. (A) “Attitude” of opiate addicts toward opiate-like drugs. (B) A short-term “direct” addiction test. J Pharmacol Exp Ther 133:371–387
Galski T, Williams JB, Ehle HT (2000) Effects of opioids on driving ability. J Pain Symptom Manage 19:200–208
Hayley AC, Downey LA, Green M, Shiferaw B, Kenneally M, Keane M, Adams M, Shehabi Y (2019) Driving simulator performance after administration of analgesic doses of ketamine with dexmedetomidine or fentanyl. J Clin Psychopharmacol 39:446–454
Hedlund J, Macek K (2018) Drug-impaired driving: marijuana and opioids raise critical issues for states. Governor’s Highway Safety Association, Washington, DC https://www.ghsa.org/resources/DUID18
Irwin C, Iudakhina E, Desbrow B, McCartney D (2017) Effects of acute alcohol consumption on measures of simulated driving: a systematic review and meta-analysis. Accid Anal Prev 102:248–266
Jongen S, Vuurman EF, Ramaekers JG, Vermeeren A (2016) The sensitivity of laboratory tests assessing driving related skills to dose-related impairment of alcohol: a literature review. Accid Anal Prev 89:31–48
King AC, de Wit H, McNamara PJ, Cao D (2011) Rewarding, stimulant, and sedative alcohol responses and relationship to future binge drinking. Arch Gen Psychiatry 68:389–399
King AC, McNamara PJ, Hasin DS, Cao D (2014) Alcohol challenge responses predict future alcohol use disorder symptoms: a 6-year prospective study. Biol Psychiatry 75:798–806
King AC, Cao D, de Wit H, O’Connor SJ, Hasin DS (2019) The role of alcohol response phenotypes in the risk for alcohol use disorder. Br J Psych 5(e38):1–3
Kirkpatrick MG, de Wit H (2013) In the company of others: social factors alter acute alcohol effects. Psychopharmacology (Berl) 230:215–226
Kress HG, Kraft B (2005) Opioid medication and driving ability. Eur J Pain 9:141–144
Lacey JH, Kelley-Baker T, Berning A, Romano E, Ramirez A, Yao J, Moore C, Brainard K, Carr K, Pell K, Compton R (2016) Drug and alcohol crash risk: a case-control study (Report No. DOT HS 812 355). National Highway Traffic Safety Administration, Washington, DC
Lenne MG, Dietze P, Rumbold GR, Redman JR, Triggs TJ (2003) The effects of the opioid pharmacotherapies methadone, LAAM and buprenorphine, alone and in combination with alcohol, on simulated driving. Drug Alcohol Depend 72:271–278
Linnoila M, Hakkinen S (1974) Effects of diazepam and codeine, alone and in combination with alcohol, on simulated driving. Clin Pharmacol Ther 15:368–373
Martin CS, Earleywine M, Musty RE, Perrine MW, Swift RM (1993) Development and validation of the biphasic alcohol effects scale. Alcohol Clin Exp Res 17(1):140–146
Miceli L, Bednarova R, Rizzardo A, Samogin V, Della Rocca G (2015) Development of a test for recording both visual and auditory reaction times, potentially useful for future studies in patients on opioids therapy. Drug Des Devel Ther 9:817
National Center for Statistics and Analysis (2019) Alcohol-impaired driving: 2018 data (Traffic Safety Facts. Report No. DOT HS 812 864). National Highway Traffic Safety Administration, Washington, DC
National Survey on Drug Use and Health, Center for Behavioral Health Statistics and Quality. Results from the 2018 National Survey on Drug Use and Health: detailed tables. Rockville (MD): SAMHSA; 2019. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables
Nilsen HK, Landro NI, Kaasa S, Jenssen GD, Fayers P, Borchgrevink PC (2011) Driving functions in a video simulator in chronic non-malignant pain patients using and not using codeine. Eur J Pain 15:409–415
Rush CR (2001) Pretreatment with hydromorphone, a mu-opioid agonist, does not alter the acute behavioral and physiological effects of ethanol in humans. Alcohol Clin Exp Res 25:9–17
Setnik B, Sokolowska M, Johnson F, Oldenhof J, Romach M (2014) Evaluation of the safety, pharmacodynamic, and pharmacokinetic effects following oral coadministration of immediate-release morphine with ethanol in healthy male participants. Hum Psychopharmacol 29:251–265
Strand MC, Arnestad M, Fjeld B, Morland J (2017) Acute impairing effects of morphine related to driving: a systematic review of experimental studies to define blood morphine concentrations related to impairment in opioid-naive subjects. Traffic Inj Prev 18:788–794
Strand MC, Vindenes V, Gjerde H, Morland JG, Ramaekers JG (2019) A clinical trial on the acute effects of methadone and buprenorphine on actual driving and cognitive function of healthy volunteers. Br J Clin Pharmacol 85:442–453
Tori ME, Larochelle MR, Naimi TS (2020) Alcohol or benzodiazepine co-involvement with opioid overdose deaths in the United States, 1999-2017. JAMA Netw Open 3:e202361
Walsh SL, Nuzzo PA, Lofwall MR, Holtman JR Jr (2008) The relative abuse liability of oral oxycodone, hydrocodone and hydromorphone assessed in prescription opioid abusers. Drug Alcohol Depend 98:191–202
Yadav AK, Velaga NR (2019) Laboratory analysis of driving behavior and self-perceived physiological impairment at 0.03%, 0.05% and 0.08% blood alcohol concentrations. Drug Alcohol Depend 205:107630
Zacny JP, Gutierrez S (2011) Subjective, psychomotor, and physiological effects of oxycodone alone and in combination with ethanol in healthy volunteers. Psychopharmacology (Berl) 218:471–481
Acknowledgments
We thank Dr. Samy-Claude Elayi for patient support, the UK Investigational Pharmacy for preparing study medication, and the staff at the University of Kentucky (UK) Center on Drug and Alcohol Research for research support: Victoria Vessels, Emily Greene, Lindy Howe, and Russell Lewis.
Funding
This study was funded by grants from the National Institute on Drug Abuse (R56 DA036635 [SLW]) and the National Center for Advancing of Translational Sciences (KL2 TR000116-04 [SB]; UL1TR001998 [UK CTSA]).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All participants provided sober, written informed consent prior to participation and were paid for their participation. The study was approved by the University of Kentucky Institutional Review Board and was conducted in accordance with the Helsinki guidelines for ethical research.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Babalonis, S., Coe, M.A., Nuzzo, P.A. et al. Acute administration of oxycodone, alcohol, and their combination on simulated driving—preliminary outcomes in healthy adults. Psychopharmacology 238, 539–549 (2021). https://doi.org/10.1007/s00213-020-05702-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05702-w